A significant discovery in the fight against #LongCovid!
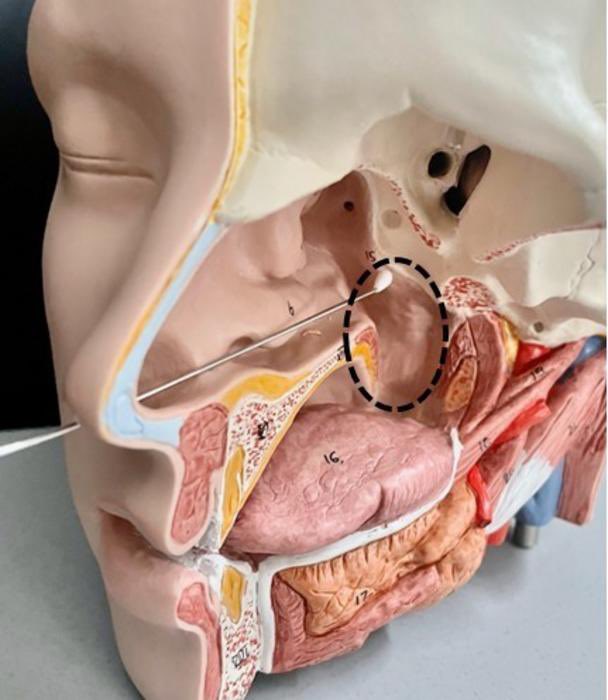
➡️ Researchers have identified the epipharynx, a part of the pharynx, as a key site for chronic inflammation driven by residual SARS-CoV-2 RNA. 1/
➡️ Researchers have identified the epipharynx, a part of the pharynx, as a key site for chronic inflammation driven by residual SARS-CoV-2 RNA. 1/

Using a next-generation molecular mapping technology called Visium HD spatial transcriptomics, researchers from Japan provided the world's first high-resolution spatial gene expression analysis of the epipharynx in patients with longCOVID. 2/ 

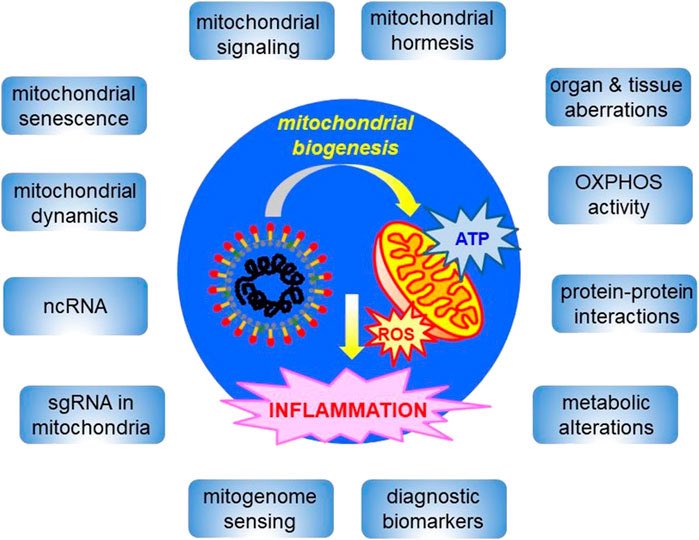
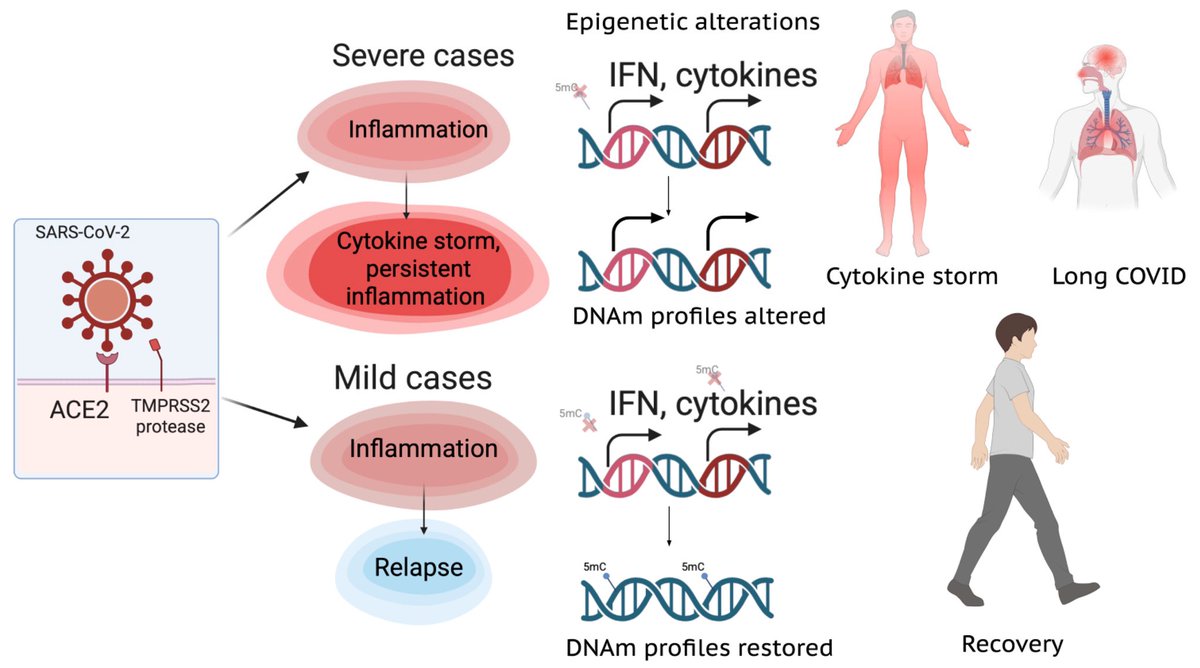
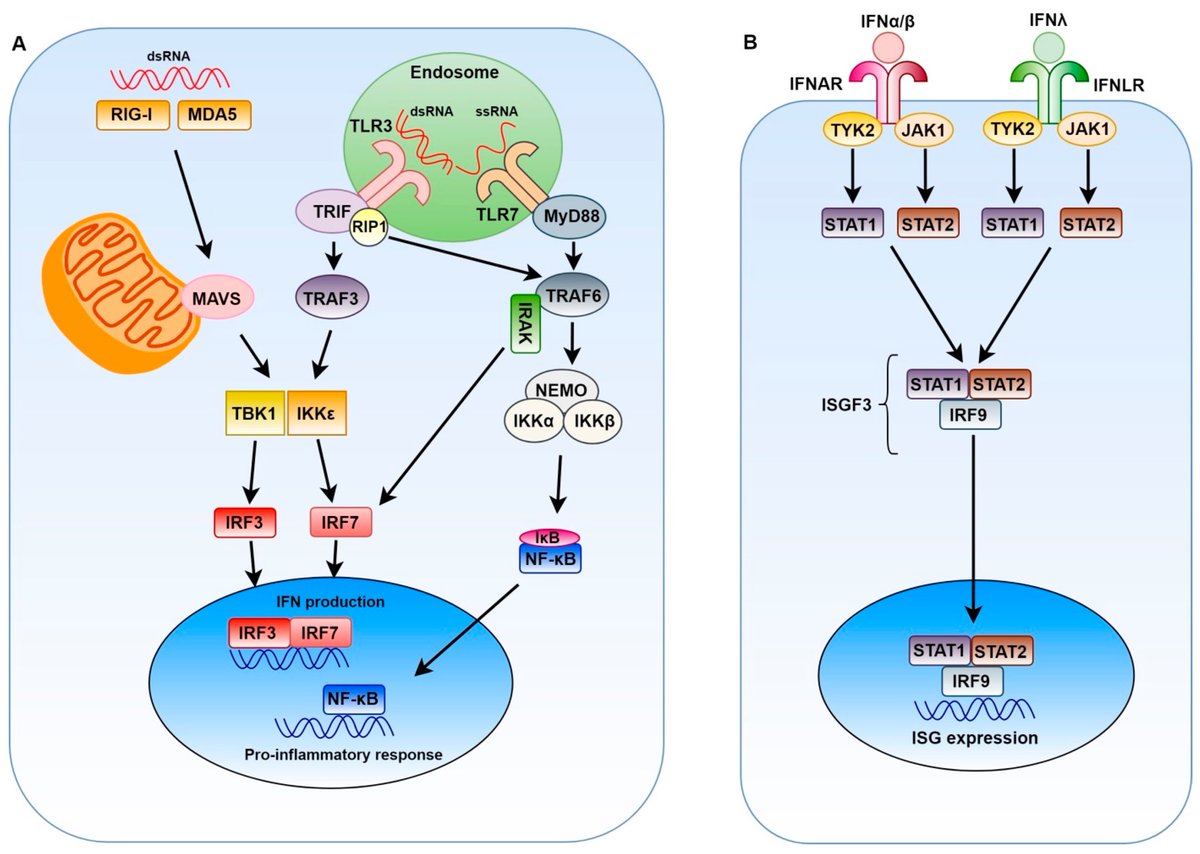
According to the study, the viral RNA from SARS-CoV-2 can persist in the epipharynx for more than six months post-infection, and here they activate local immune signals in specialized cells like B cells, plasmacytoid dendritic cells, and ciliated epithelial cells. 3/ 

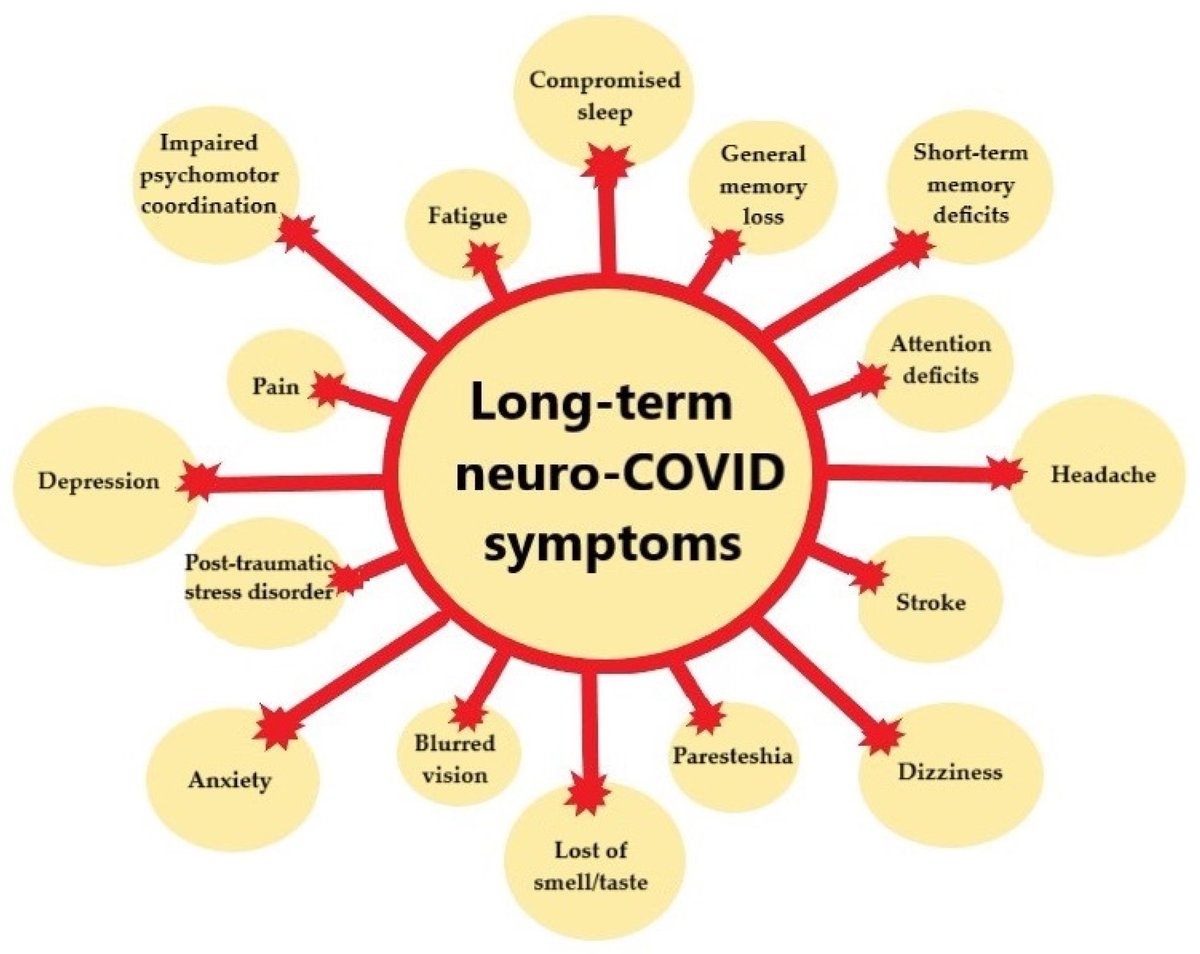
This signaling potentially contributes to the chronic symptoms experienced by patients with long COVID, which include fatigue, persistent cough, dizziness, and cognitive issues continuing for months after the acute phase of infection. 4/ 
Using advanced technique, the researchers found that the residual viral RNA isn't merely leftover debris; instead, it actively triggers immune responses and inflammation. 5/ 
The epipharynx is one of the most important sites for SARS-CoV-2 infection, yet its anatomical location makes it difficult to observe w/out endoscopic evaluation. This region will gain more research attention as a potential target in understanding and treating longCOVID 6/ 
To address the issue, the team explored epipharyngeal abrasive therapy (EAT) as a treatment. EAT is a treatment for chronic epipharyngitis that has been practiced in since the 1960s, involving the swabbing of the epipharynx with a 1% zinc chloride solution. 7/ 
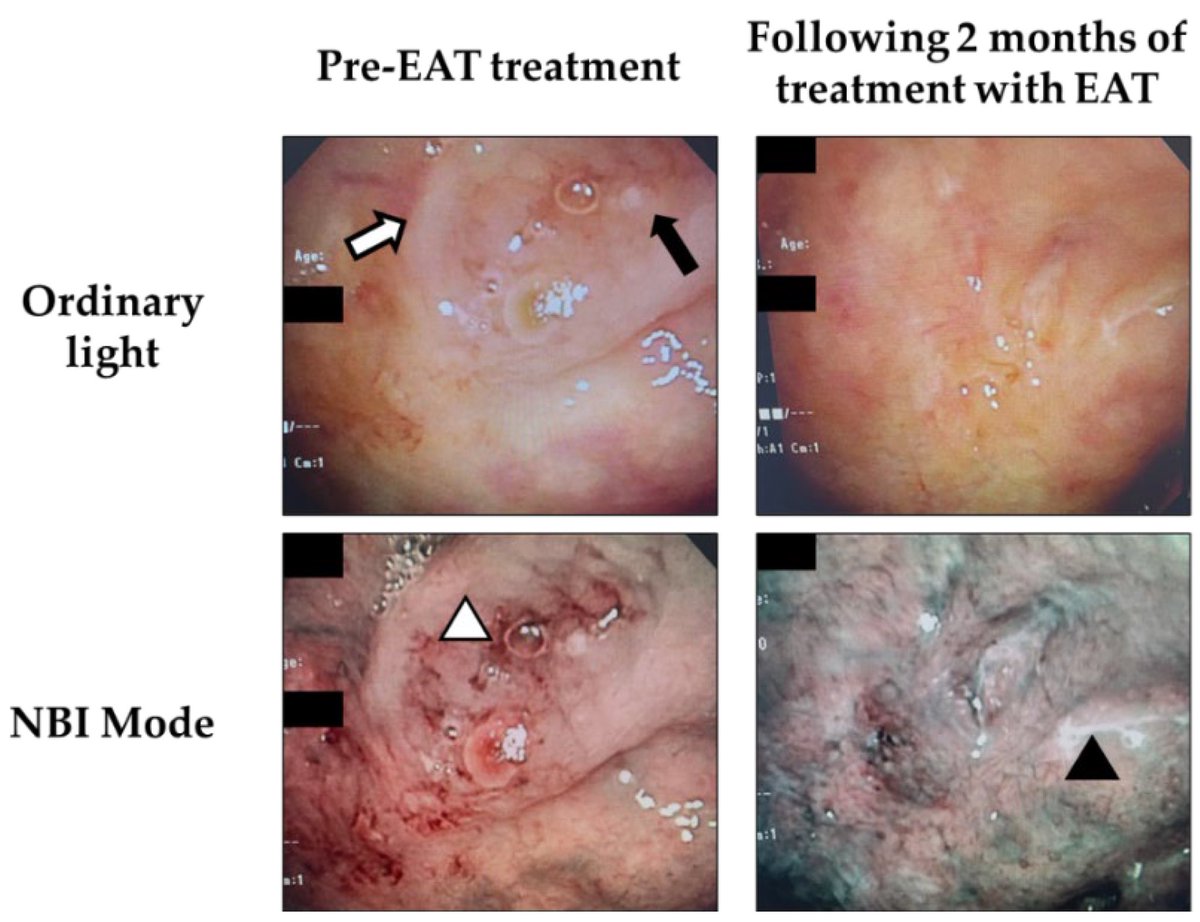
After three months of weekly EAT treatment, the patients showed a remarkable improvement in symptoms. 8/ 
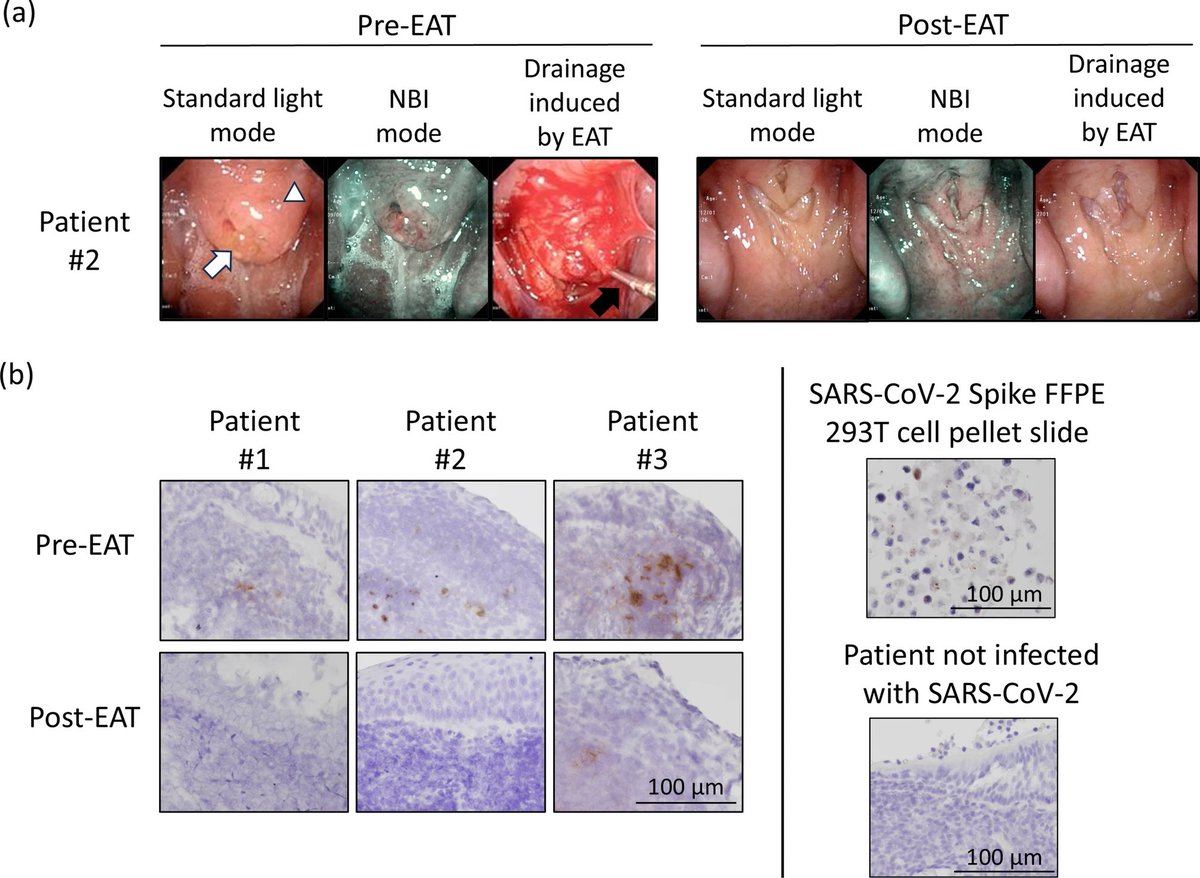
On a closer analysis, the researchers observed a significant reduction in the viral RNA and a suppression of inflammatory responses marked by a decrease in expression of signaling molecules like pro-inflammatory cytokines and antibody-related genes. 9/
The spatial gene analysis post-treatment revealed that EAT promotes the removal of damaged ciliated epithelium. Additionally, it also downregulates the overactive immune pathways, underscoring its promising role in immune modulation and tissue repair. 10/ 
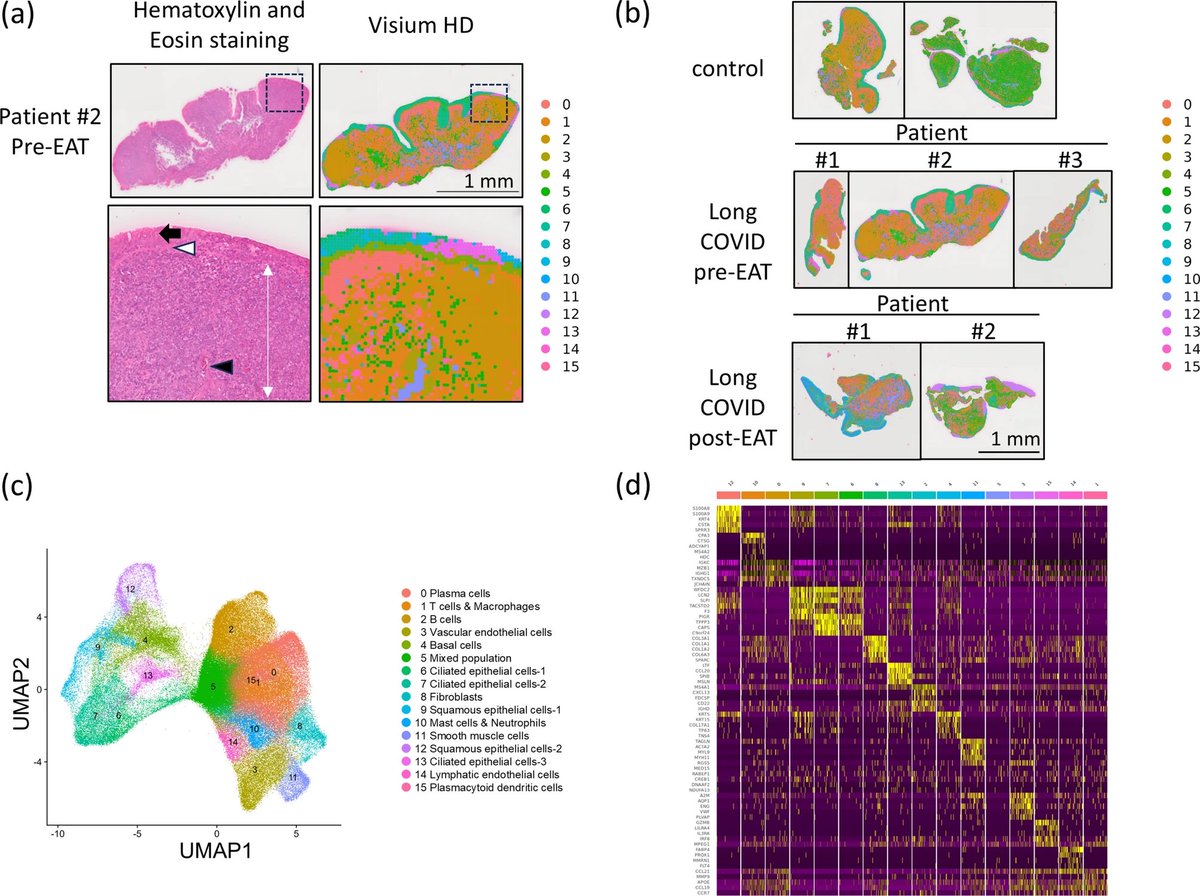
Spatial transcriptomic analysis has enabled a deeper understanding of the biology of longCOVID from a completely different perspective than conventional approaches, including the potential application of a treatment already in clinical use in Japan. 11/
While most existing treatments focus on managing these symptoms, this study goes deeper, identifying the epipharynx as a hidden reservoir of viral RNA and immune disruption, thereby opening new avenues for more targeted therapies. 12/
The study marks a significant leap in medical science, especially in light of estimates showing that 31–69% of recovered COVID-19 patients continue to suffer lingering symptoms. 13/13
nature.com/articles/s4159…
nature.com/articles/s4159…
• • •
Missing some Tweet in this thread? You can try to
force a refresh