Most people try to improve their gut health the wrong way.
So if you are struggling with gut issues such as bloating, constipation, IBS,SIBO, SIFO and candida, here's the ultimate plan for improving them.
Master thread🧵
So if you are struggling with gut issues such as bloating, constipation, IBS,SIBO, SIFO and candida, here's the ultimate plan for improving them.
Master thread🧵
*Standard disclaimer that nothing in this thread should be used as a substitute for medical advice and that plenty of people will not have to apply all of these in order to experience improvements*
When it comes to our health, everything starts from and depends on the gut.
From low testosterone, histamine intolerance, depression, chronic fatigue, ED and skin problems, all the way to hair loss, optimizing ones gut health is a non-negotiable step in improving any health issue that he might want to.

When it comes to our health, everything starts from and depends on the gut.
From low testosterone, histamine intolerance, depression, chronic fatigue, ED and skin problems, all the way to hair loss, optimizing ones gut health is a non-negotiable step in improving any health issue that he might want to.


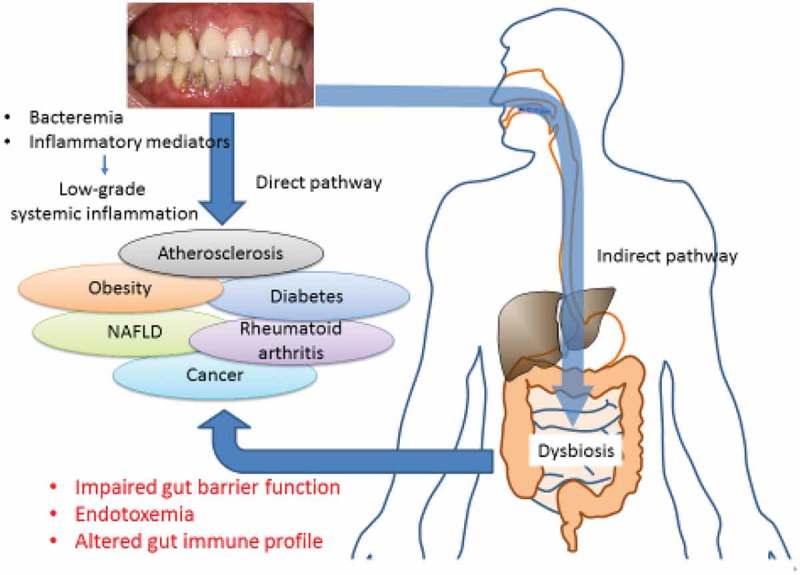
Our gut is connected to every single one of the organs in the human body, so it's fair to say that everything is affected by a great part from it.
You know this to be true if you've ever struggled with a gut issue but in case you haven't and are skeptical about this claim, you can check out these 3 basic studies (one for the skin, one for the immune system and one for testosterone):
pmc.ncbi.nlm.nih.gov/articles/PMC79…
pmc.ncbi.nlm.nih.gov/articles/PMC49…
pmc.ncbi.nlm.nih.gov/articles/PMC76…

You know this to be true if you've ever struggled with a gut issue but in case you haven't and are skeptical about this claim, you can check out these 3 basic studies (one for the skin, one for the immune system and one for testosterone):
pmc.ncbi.nlm.nih.gov/articles/PMC79…
pmc.ncbi.nlm.nih.gov/articles/PMC49…
pmc.ncbi.nlm.nih.gov/articles/PMC76…


But the question remains, how can you improve the state of your gut since most likely, most of the advice that's out there such as "eat more fiber", hasn't really helped you.
Well we have two parts when it comes to this answer.
The first one is the non-negotiable things all of us must apply in order to have a healthy gut microbiome in the long run.
The second one is more contextual one and addresses specific issues such as pathogen overgrowths or IBS for example.
So let's dive in.
Well we have two parts when it comes to this answer.
The first one is the non-negotiable things all of us must apply in order to have a healthy gut microbiome in the long run.
The second one is more contextual one and addresses specific issues such as pathogen overgrowths or IBS for example.
So let's dive in.

Part 1: The non-negotiables.
First and foremost, avoid the following foods that can negatively impact gut health in general:
1. The consumption of highly processed foods.
These are problematic for a variety of reasons.
Most of them for example will have emulsifiers and preservatives in them which are shown to disrupt the gut microbiome by altering bacterial composition and increasing inflammation.
Then most will be devoided of nutrients and the ones that aren’t often are high in histamine and also packaged in ways that leads to the leakage of toxins such ass aluminum (thik canned seafood for example).
2. The consumption of too many acellular carbs (think refined sugars).
These in excess promote the growth of harmful bacteria and yeast, leading to dysbiosis.
They also increase gut permeability by disrupting tight junction proteins.
3. Artificial sweeteners such as aspartame, sucralose, saccharin and acesulfame potassium.
Even though it is in fact true that in order for these to show a direct and immediate impact on things such as cancer, the doses that are required are quite high, in the context of gut health, even in small amounts they can alter gut bacterial diversity, reducing beneficial species like Bifidobacterium and increasing pro-inflammatory bacteria.
4. High O6 and trans fats.
Trans and easily oxidized fats produce pro inflammatory cytokines, damaging the gut lining and are also shown to reduce beneficial bacteria.
5. Excessive alcohol intake (if you have any gut issue, take a 2 month break from all alcoholic beverages, and if you have any pathogen overgrowth avoid all beers, ciders and wines for 4 months).
Alcohol is known to disrupt tight junctions, reduce microbial diversity and in the case of detoxing, it will of course over burden the liver.
6. Hybridized grains.
Overall, after 1960 we started creating wheat hybrids with the purpose of the plant being able to survive some pretty harsh climates.
Now the gluten that’s presented in hybridized grains is so hard to digest that it will inevitably lead to your gut taking such as big hit if they are consumed very often.
Note: Gluten is a mixture of different protein types (mainly gliadin and glutenin) or a protein composite that is found in things such as wheat, rye and barley.
Not only that but please also consider that we no longer sprout or ferment the grains a lot of the times which is designed to break down some of the gluten but also compounds such as phytic acid.
Then in a lot of countries such as the states, grains are probably the number 2 (soy is probably the number 1) thing that is sprayed with enormous amounts of herbicides such as glyphosate.
Gluten also triggers the release of zonulin (a protein that regulates the permeability of the intestinal wall by modulating the tight junctions).
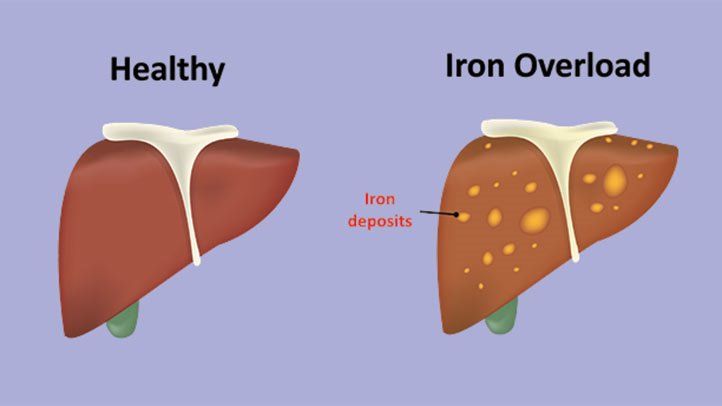
Then, we have the issue of mycotoxin contamination and of course the fact that plenty of grains are fortified with folic acid and forms of iron that are basically iron shavings.
Some people are also sensitive to plant albumin.
7. A1 dairy and the overconsumption of dairy overall (even too much milk can dilute stomach acid for example and cause issues).
A2 dairy have proline in the 67 position of the beta casein chain while A1 dairy have histidine.
This can make a night and day difference when consuming dairy and makes A1 dairy a no go for people struggling with mast cell issues and and will inevitably lead to inflammation compared to A2.
8. The over consumption of high-FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) foods such as onions, garlic, beans, lentils, wheat, apples, pears, stone fruits, honey, high-fructose fruits etc that lead to fast fermentation by gut bacteria.
9. Foods rich in phytates and oxalates that will bind to minerals such as zinc, iron, and calcium, reducing their absorption and potentially impairing gut cell function.
10. The overconsumption of caffeine (>100mg/day) increases peristalsis and reduces mucus production.
11. Herbicides and pesticides like glyphosate that act as antibiotics and reduce beneficial gut bacteria. Note: N-phosphomethylglycine aka glyphosate, works by inhibiting the enzyme 5-enolpyruvylshikimate-3-phosphate (EPSP) synthase.
This results in disrupting the shikimic acid pathway and reducing the aromatic amino acids.
In general, the shikimic acid pathway is responsible for the production of vitamins and aromatic amino acids such as phenylalanine through EPSP synthase so disrupting it negatively affects eNOS, the pancreas, adrenals, SOD, CAT and GPx enzymes, glutamate, GABA, the metabolism of retinoic acid and inhibiting GGT plus G6PD and can even exacerbate the damage that aluminum causes.
First and foremost, avoid the following foods that can negatively impact gut health in general:
1. The consumption of highly processed foods.
These are problematic for a variety of reasons.
Most of them for example will have emulsifiers and preservatives in them which are shown to disrupt the gut microbiome by altering bacterial composition and increasing inflammation.
Then most will be devoided of nutrients and the ones that aren’t often are high in histamine and also packaged in ways that leads to the leakage of toxins such ass aluminum (thik canned seafood for example).
2. The consumption of too many acellular carbs (think refined sugars).
These in excess promote the growth of harmful bacteria and yeast, leading to dysbiosis.
They also increase gut permeability by disrupting tight junction proteins.
3. Artificial sweeteners such as aspartame, sucralose, saccharin and acesulfame potassium.
Even though it is in fact true that in order for these to show a direct and immediate impact on things such as cancer, the doses that are required are quite high, in the context of gut health, even in small amounts they can alter gut bacterial diversity, reducing beneficial species like Bifidobacterium and increasing pro-inflammatory bacteria.
4. High O6 and trans fats.
Trans and easily oxidized fats produce pro inflammatory cytokines, damaging the gut lining and are also shown to reduce beneficial bacteria.
5. Excessive alcohol intake (if you have any gut issue, take a 2 month break from all alcoholic beverages, and if you have any pathogen overgrowth avoid all beers, ciders and wines for 4 months).
Alcohol is known to disrupt tight junctions, reduce microbial diversity and in the case of detoxing, it will of course over burden the liver.
6. Hybridized grains.
Overall, after 1960 we started creating wheat hybrids with the purpose of the plant being able to survive some pretty harsh climates.
Now the gluten that’s presented in hybridized grains is so hard to digest that it will inevitably lead to your gut taking such as big hit if they are consumed very often.
Note: Gluten is a mixture of different protein types (mainly gliadin and glutenin) or a protein composite that is found in things such as wheat, rye and barley.
Not only that but please also consider that we no longer sprout or ferment the grains a lot of the times which is designed to break down some of the gluten but also compounds such as phytic acid.
Then in a lot of countries such as the states, grains are probably the number 2 (soy is probably the number 1) thing that is sprayed with enormous amounts of herbicides such as glyphosate.
Gluten also triggers the release of zonulin (a protein that regulates the permeability of the intestinal wall by modulating the tight junctions).
Then, we have the issue of mycotoxin contamination and of course the fact that plenty of grains are fortified with folic acid and forms of iron that are basically iron shavings.
Some people are also sensitive to plant albumin.
7. A1 dairy and the overconsumption of dairy overall (even too much milk can dilute stomach acid for example and cause issues).
A2 dairy have proline in the 67 position of the beta casein chain while A1 dairy have histidine.
This can make a night and day difference when consuming dairy and makes A1 dairy a no go for people struggling with mast cell issues and and will inevitably lead to inflammation compared to A2.
8. The over consumption of high-FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) foods such as onions, garlic, beans, lentils, wheat, apples, pears, stone fruits, honey, high-fructose fruits etc that lead to fast fermentation by gut bacteria.
9. Foods rich in phytates and oxalates that will bind to minerals such as zinc, iron, and calcium, reducing their absorption and potentially impairing gut cell function.
10. The overconsumption of caffeine (>100mg/day) increases peristalsis and reduces mucus production.
11. Herbicides and pesticides like glyphosate that act as antibiotics and reduce beneficial gut bacteria. Note: N-phosphomethylglycine aka glyphosate, works by inhibiting the enzyme 5-enolpyruvylshikimate-3-phosphate (EPSP) synthase.
This results in disrupting the shikimic acid pathway and reducing the aromatic amino acids.
In general, the shikimic acid pathway is responsible for the production of vitamins and aromatic amino acids such as phenylalanine through EPSP synthase so disrupting it negatively affects eNOS, the pancreas, adrenals, SOD, CAT and GPx enzymes, glutamate, GABA, the metabolism of retinoic acid and inhibiting GGT plus G6PD and can even exacerbate the damage that aluminum causes.

Then, provide the following dietary nutrients that are crucial for many things such as HCL production, digestive enzymes, bile production, preventing the oxygenation of the gut, butyrate production, intestinal barrier health and more.
These are: Vitamin K, zinc, B vitamins, glycine, CHOLINE, selenium, vitamin C, (some) iodine, glutamine, magnesium, potassium, sodium (a lot of people neglect how crucial sodium is for our digestion) and vitamin A.
Zinc for example is a mineral so crucial for our gut health that when we consume too little of it the intestinal barrier literally falls apart.
“So what can i eat?”
A list of relatively safe foods that provide these key nutrients would include things like:
•Ruminant bone in meats
•Sea salt
•Pasture-raised eggs
•Organic organ meats
•Quality bone marrow
•White fish and oysters if you can source them right
•Soups
•Sprouted white rice
•Some potatoes
•Organic fruit
•Coconut oil
•Grass fed tallow and EVOO
•Vegetables that you find easy to digest and have in fact benefits such as asparagus, mushrooms, garlic, carrots and zucchini for example
•Manuka honey or maple syrup in moderation (unless you have a profound pathogen overgrowth)
•Spices such as Ceylon cinnamon
•Pro and prebiotic rich foods (unless you have a profound pathogen overgrowth or MCAS)
And in general, single ingredient foods that have more benefits for your digestion than downsides.



These are: Vitamin K, zinc, B vitamins, glycine, CHOLINE, selenium, vitamin C, (some) iodine, glutamine, magnesium, potassium, sodium (a lot of people neglect how crucial sodium is for our digestion) and vitamin A.
Zinc for example is a mineral so crucial for our gut health that when we consume too little of it the intestinal barrier literally falls apart.
“So what can i eat?”
A list of relatively safe foods that provide these key nutrients would include things like:
•Ruminant bone in meats
•Sea salt
•Pasture-raised eggs
•Organic organ meats
•Quality bone marrow
•White fish and oysters if you can source them right
•Soups
•Sprouted white rice
•Some potatoes
•Organic fruit
•Coconut oil
•Grass fed tallow and EVOO
•Vegetables that you find easy to digest and have in fact benefits such as asparagus, mushrooms, garlic, carrots and zucchini for example
•Manuka honey or maple syrup in moderation (unless you have a profound pathogen overgrowth)
•Spices such as Ceylon cinnamon
•Pro and prebiotic rich foods (unless you have a profound pathogen overgrowth or MCAS)
And in general, single ingredient foods that have more benefits for your digestion than downsides.




Then, make sure to avoid the following dietary HABITS.
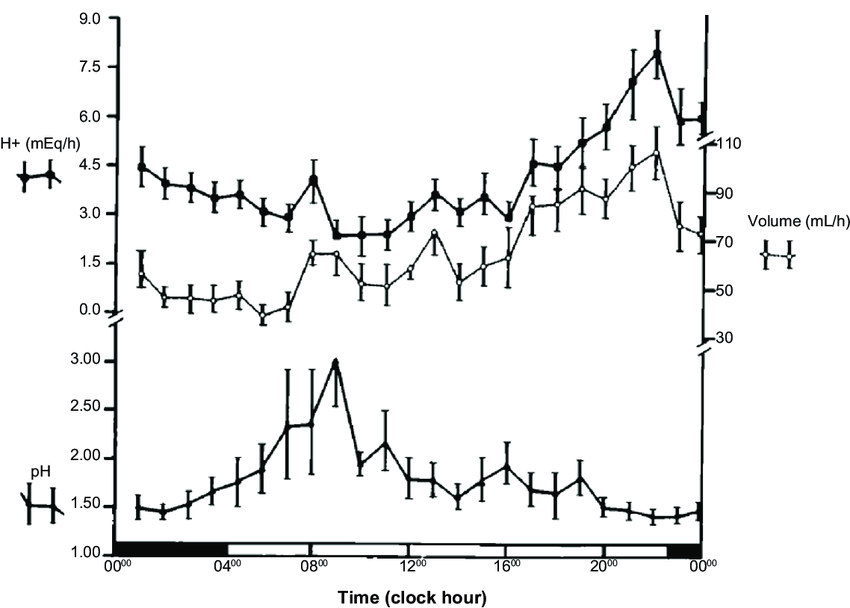
1. Irregular eating patterns that reduce gastric acid and enzyme production and disrupt the gut’s circadian rhythm, microbial balance and motility.
2. Eating too quickly or large portion sizes both of which will lead to incomplete digestion and fermentation in the gut.
3. Eating late at night will also disrupt the gut’s circadian rhythm, impairing microbial balance and motility.
It will also increase the risk of acid reflux, as lying down after eating allows stomach acid to enter the esophagus.
4. Inadequate hydration which was previously discussed and will reduce mucus production while also slowing motility.
5. Frequent snacking.
Eating something every 1-2 hours, does not allow the migrating motor complex (MMC (a cyclical pattern of peristaltic activity that occurs during fasting state)) to clear bacteria from the small intestine for example.
6. Eating stressed.
It's called "rest and digest" for a reason.
Stress ruins our digestion and you can approach this from multiple angles.
pubmed.ncbi.nlm.nih.gov/22314561/
It reduces blood flow, it severely decreases the expression of lysozyme which is responsible for killing bacteria (way more than even stomach acid) and in general ruins our gut.
I know that managing stress can be proven hard but try to eat every one of your meals consciously. It's a good start and it WILL pay off.
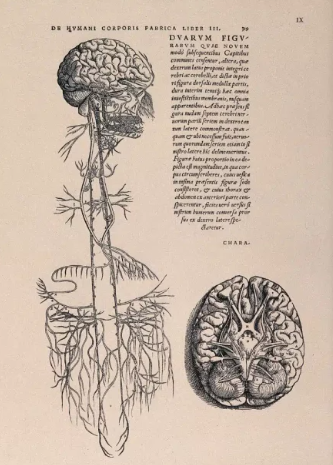
You can also try stimulating the vagus nerve.
When it comes to the vagus nerve, it affects the parasympathetic control of digestion and heart rate but even speech through the recurrent laryngeal nerve.
Some of its branches include the aortic nerve, the anterior vagan trunk, the pharyngeal never, the superior laryngeal nerve, the aortic nerve, the inferior cervical nerve and the recurrent laryngeal nerve.
Except for the adrenals, it supplies (motor) parasympathetic fibers to all the organs (electrically stimulating the vagus nerve, has been shown to slow the heart rate).
This is also why a lot of the time people try to stimulate the vagus nerve in order to relax or even to lower blood pressure and why deep and slow breathing has a relaxing effect (it stimulates the vagus nerve).
In fact, you can try the following right now.
Breathe very slowly and aim to get one breath every 10 seconds (try a 4 second inhale and a 6 second exhale (since the exhale triggers the relaxation response). You can also try breathing for 4 seconds, holding your breath for 1 and exhaling for 5 seconds.
If you do 5-6 rounds of these, you will find yourself more relaxed.
Other things that you can try out (do not laugh, they work) are loudly gargling water, massages (which increase GABA a LOT as well), stretching and getting a bucket of cold water and some ice and only putting your face in.

1. Irregular eating patterns that reduce gastric acid and enzyme production and disrupt the gut’s circadian rhythm, microbial balance and motility.
2. Eating too quickly or large portion sizes both of which will lead to incomplete digestion and fermentation in the gut.
3. Eating late at night will also disrupt the gut’s circadian rhythm, impairing microbial balance and motility.
It will also increase the risk of acid reflux, as lying down after eating allows stomach acid to enter the esophagus.
4. Inadequate hydration which was previously discussed and will reduce mucus production while also slowing motility.
5. Frequent snacking.
Eating something every 1-2 hours, does not allow the migrating motor complex (MMC (a cyclical pattern of peristaltic activity that occurs during fasting state)) to clear bacteria from the small intestine for example.
6. Eating stressed.
It's called "rest and digest" for a reason.
Stress ruins our digestion and you can approach this from multiple angles.
pubmed.ncbi.nlm.nih.gov/22314561/
It reduces blood flow, it severely decreases the expression of lysozyme which is responsible for killing bacteria (way more than even stomach acid) and in general ruins our gut.
I know that managing stress can be proven hard but try to eat every one of your meals consciously. It's a good start and it WILL pay off.
You can also try stimulating the vagus nerve.
When it comes to the vagus nerve, it affects the parasympathetic control of digestion and heart rate but even speech through the recurrent laryngeal nerve.
Some of its branches include the aortic nerve, the anterior vagan trunk, the pharyngeal never, the superior laryngeal nerve, the aortic nerve, the inferior cervical nerve and the recurrent laryngeal nerve.
Except for the adrenals, it supplies (motor) parasympathetic fibers to all the organs (electrically stimulating the vagus nerve, has been shown to slow the heart rate).
This is also why a lot of the time people try to stimulate the vagus nerve in order to relax or even to lower blood pressure and why deep and slow breathing has a relaxing effect (it stimulates the vagus nerve).
In fact, you can try the following right now.
Breathe very slowly and aim to get one breath every 10 seconds (try a 4 second inhale and a 6 second exhale (since the exhale triggers the relaxation response). You can also try breathing for 4 seconds, holding your breath for 1 and exhaling for 5 seconds.
If you do 5-6 rounds of these, you will find yourself more relaxed.
Other things that you can try out (do not laugh, they work) are loudly gargling water, massages (which increase GABA a LOT as well), stretching and getting a bucket of cold water and some ice and only putting your face in.

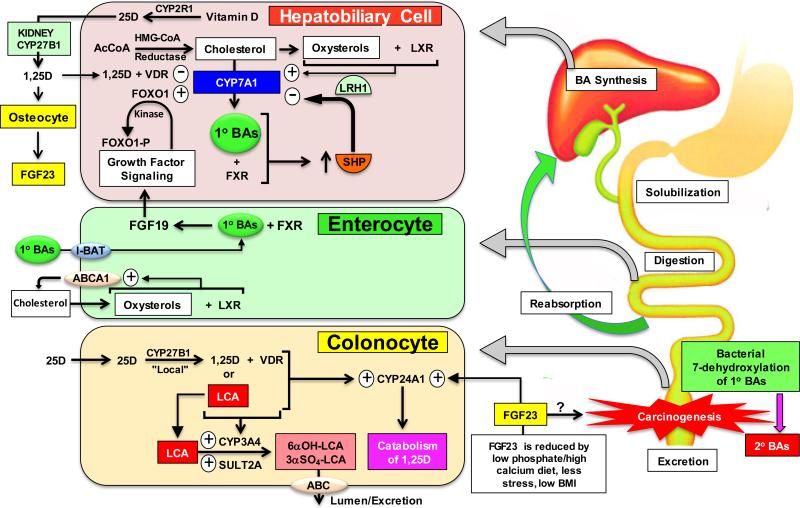
Then, do not neglect sunlight and vitamin D.
Vitamin D for example:
-Regulates the expression of tight junction proteins such as claudins, occludins, and zonula occludens-1 (ZO-1).
-Promotes the growth of beneficial bacteria, such as Lactobacillus and Bifidobacterium, which produce short-chain fatty acids (SCFAs) like butyrate.
-Suppresses pathogenic bacteria, such as Clostridium difficile, by enhancing antimicrobial peptide production.
-Acts as an immune modulator by binding to VDRs in immune cells, such as T-cells, B-cells, and macrophages, within the gut-associated lymphoid tissue (GALT).
-Promotes the differentiation of T-regulatory cells.
-Stimulates the production of antimicrobial peptides, such as cathelicidins and β-defensins, enhances epithelial cell proliferation and wound healing by upregulating growth factors like transforming growth factor-beta (TGF-β).
-Downregulates oncogenic pathways.
When it comes to sunlight in general it stimulates alpha-MSH, a peptide with antimicrobial and anti-inflammatory properties, effective against Candida, E. coli, and Staphylococcus aureus for example.

Vitamin D for example:
-Regulates the expression of tight junction proteins such as claudins, occludins, and zonula occludens-1 (ZO-1).
-Promotes the growth of beneficial bacteria, such as Lactobacillus and Bifidobacterium, which produce short-chain fatty acids (SCFAs) like butyrate.
-Suppresses pathogenic bacteria, such as Clostridium difficile, by enhancing antimicrobial peptide production.
-Acts as an immune modulator by binding to VDRs in immune cells, such as T-cells, B-cells, and macrophages, within the gut-associated lymphoid tissue (GALT).
-Promotes the differentiation of T-regulatory cells.
-Stimulates the production of antimicrobial peptides, such as cathelicidins and β-defensins, enhances epithelial cell proliferation and wound healing by upregulating growth factors like transforming growth factor-beta (TGF-β).
-Downregulates oncogenic pathways.
When it comes to sunlight in general it stimulates alpha-MSH, a peptide with antimicrobial and anti-inflammatory properties, effective against Candida, E. coli, and Staphylococcus aureus for example.


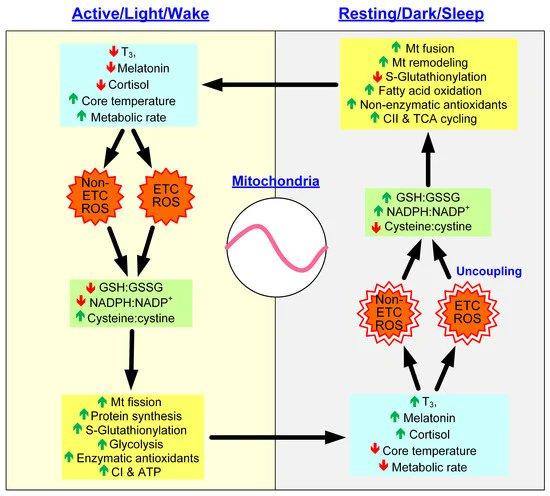
Go to sleep.
Melatonin for example acts as a potent antioxidant in the gastrointestinal tract, enhances mucosal repair and regulates gut motility.
Also, during sleep, immune cells like T-cells and B-cells in the gut are replenished and primed to combat pathogens.
Melatonin for example acts as a potent antioxidant in the gastrointestinal tract, enhances mucosal repair and regulates gut motility.
Also, during sleep, immune cells like T-cells and B-cells in the gut are replenished and primed to combat pathogens.
https://x.com/Helios_Movement/status/1933489252232253571
Work on bile.
The gut eliminates LPS and other toxins via stool, with bile as a carrier for example.
So poor bile flow makes impossible to resolve common "gut" issues such as SIBO.
But before you hop on TUDCA (something that can backfire a lot if the lining is harmed), realize that without:
-Choline
-Glycine
-Taurine
-Vitamin C (without it 7-alpha-hydroxylase won't work that great).
-Vitamin D/Sunlight
-Magnesium
-Healthy HCL
-B6
-NOT doing crazy fats
-Circadian health
-Eating some bitter foods
Nothing will really work in the long run.
Then, be aware of toxins.
The gut eliminates LPS and other toxins via stool, with bile as a carrier for example.
So poor bile flow makes impossible to resolve common "gut" issues such as SIBO.
But before you hop on TUDCA (something that can backfire a lot if the lining is harmed), realize that without:
-Choline
-Glycine
-Taurine
-Vitamin C (without it 7-alpha-hydroxylase won't work that great).
-Vitamin D/Sunlight
-Magnesium
-Healthy HCL
-B6
-NOT doing crazy fats
-Circadian health
-Eating some bitter foods
Nothing will really work in the long run.
Then, be aware of toxins.
Then, be aware of toxins such as xenoestrogens (think plastics, fragrances etc).
pubmed.ncbi.nlm.nih.gov/29101397/
These also are some underrated reasons when it comes to why more and more people struggling with pathogen overgrowths.
Besides this some fungi overall bind heavy metals like mercury to their cell walls as a protective mechanism.
Also if you are in the health space you are probably consuming supplements, but you might need to cut back if you want a healthy gut.
Most people underestimate the damage that common supplement additives can cause to their gut when one is gunning down 20+ pills a day (which is not that uncommon).
Of course you can't avoid all additives in all supplements.
You just calculate the ROI and trust me, it's not there when someone is consuming over 20 pills with additives such as:
-Silicon dioxide -Titanium dioxide
-Artificial colorings such as red 40, blue 2, yellow 5
-Polyethylene
and so on.
pubmed.ncbi.nlm.nih.gov/29101397/
These also are some underrated reasons when it comes to why more and more people struggling with pathogen overgrowths.
Besides this some fungi overall bind heavy metals like mercury to their cell walls as a protective mechanism.
Also if you are in the health space you are probably consuming supplements, but you might need to cut back if you want a healthy gut.
Most people underestimate the damage that common supplement additives can cause to their gut when one is gunning down 20+ pills a day (which is not that uncommon).
Of course you can't avoid all additives in all supplements.
You just calculate the ROI and trust me, it's not there when someone is consuming over 20 pills with additives such as:
-Silicon dioxide -Titanium dioxide
-Artificial colorings such as red 40, blue 2, yellow 5
-Polyethylene
and so on.
Part 2: Contextual.
First consider the following gut-related tests: Urea breath test, stool antigen test for H. pylori antigens, breath tests that measure hydrogen, methane, or hydrogen sulfide after lactulose/glucose ingestion, a stool analysis for candida, fungal culture, CHROMagar Candida.
"George, i've told that i have IBS, how will this help?".
Because we are trying to figure out what's causing it and a lot of people with IBS for example actually have SIBO.
First consider the following gut-related tests: Urea breath test, stool antigen test for H. pylori antigens, breath tests that measure hydrogen, methane, or hydrogen sulfide after lactulose/glucose ingestion, a stool analysis for candida, fungal culture, CHROMagar Candida.
"George, i've told that i have IBS, how will this help?".
Because we are trying to figure out what's causing it and a lot of people with IBS for example actually have SIBO.

If anything comes back positive, focus on tight junction health since without this, antifungals and biofilms disruptors can make the condition worse.
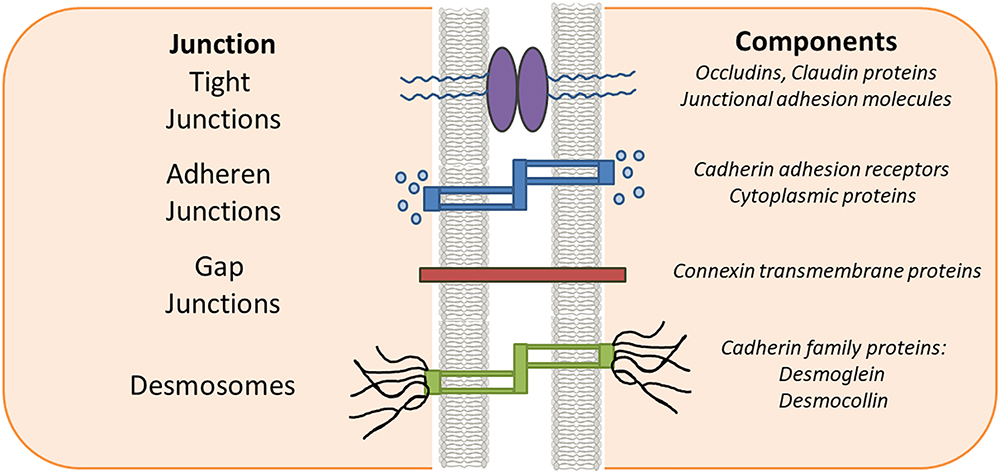
Tight junctions (TJs) are protein-based structures (their structure is broken down in a moment) that form a selective barrier between epithelial (the top region of adjacent epithelial cells) and endothelial cells primarily in the gastrointestinal (GI) tract which makes them components of the intestinal mucosal barrier.
Without TJs enterocytes and colonocytes can not function properly and overall, tight junctions are essential for preventing the uncontrolled passage of things such as bacteria, toxins and undigested food into the bloodstream maintaining a selective barrier (they allow regulated paracellular transport of small molecules such as ions, water and glucose for example through claudin pores).
They also assist the gut-associated lymphoid tissue (GALT), limit translocation of lipopolysaccharides (LPS), facilitate mucus layer integrity and do much more which is why increased permeability or leaky gut, leads to system inflammation (TLR4 is activated and cytokines such as IL-6 and TNF-a are activated after LPS, food antigens or toxins enter circulation for example), contributes to to food sensitivities (IgG-mediated), autoimmune disorder and of course, issues such as pathogen overgrowths, IBS and IBD where for example even up to 80% of people with IBS have increased permeability.
Now TJs are made out of:
1. Transmembrane proteins such as:
-Claudins which is a family of 27 proteins that determine TJ permeability (claudin-1 and -3 for example form tight seals, while claudin-2 increases pore size).
-Occludin that enhances TJ stability and regulates paracellular transport by organising TJ strands and linking them to the actin cytoskeleton via ZO protein for example or by regulating paracellular transport of ions and small molecules.
-JAMs that modulate TJ assembly and immune cell transmigration.
For example, they contribute to the initial formation of TJs by recruiting scaffolding proteins and facilitating cell-cell adhesion.
They also interact with claudins and occludin while also regulating leukocyte and monocyte transmigration across endothelial and epithelial barriers.
-Tricellulin that strengthens junctions at tricellular contacts (where three cells meet).
For example, it forms a barrier to prevent paracellular flux of macromolecules and pathogens at these sites while also binding to LSR (lipolysis-stimulated lipoprotein receptor) to maintain tricellular integrity.
2. Intracellular scaffolding proteins such as:
-Zonula occludens (ZO) proteins are members of the membrane-associated guanylate kinase (MAGUK) family and serve as intracellular scaffolding proteins that place TJ transmembrane proteins (claudins, occludin, JAMs, tricellulin) to the actin cytoskeleton, stabilize TJ structure and mediate signaling.
-Associated (cytoskeletal) proteins actin and myosin filaments in the cytoskeleton dynamically regulate TJ opening/closing via phosphorylation responding to mechanical and biochemical cues.
Tight junctions (TJs) are protein-based structures (their structure is broken down in a moment) that form a selective barrier between epithelial (the top region of adjacent epithelial cells) and endothelial cells primarily in the gastrointestinal (GI) tract which makes them components of the intestinal mucosal barrier.
Without TJs enterocytes and colonocytes can not function properly and overall, tight junctions are essential for preventing the uncontrolled passage of things such as bacteria, toxins and undigested food into the bloodstream maintaining a selective barrier (they allow regulated paracellular transport of small molecules such as ions, water and glucose for example through claudin pores).
They also assist the gut-associated lymphoid tissue (GALT), limit translocation of lipopolysaccharides (LPS), facilitate mucus layer integrity and do much more which is why increased permeability or leaky gut, leads to system inflammation (TLR4 is activated and cytokines such as IL-6 and TNF-a are activated after LPS, food antigens or toxins enter circulation for example), contributes to to food sensitivities (IgG-mediated), autoimmune disorder and of course, issues such as pathogen overgrowths, IBS and IBD where for example even up to 80% of people with IBS have increased permeability.
Now TJs are made out of:
1. Transmembrane proteins such as:
-Claudins which is a family of 27 proteins that determine TJ permeability (claudin-1 and -3 for example form tight seals, while claudin-2 increases pore size).
-Occludin that enhances TJ stability and regulates paracellular transport by organising TJ strands and linking them to the actin cytoskeleton via ZO protein for example or by regulating paracellular transport of ions and small molecules.
-JAMs that modulate TJ assembly and immune cell transmigration.
For example, they contribute to the initial formation of TJs by recruiting scaffolding proteins and facilitating cell-cell adhesion.
They also interact with claudins and occludin while also regulating leukocyte and monocyte transmigration across endothelial and epithelial barriers.
-Tricellulin that strengthens junctions at tricellular contacts (where three cells meet).
For example, it forms a barrier to prevent paracellular flux of macromolecules and pathogens at these sites while also binding to LSR (lipolysis-stimulated lipoprotein receptor) to maintain tricellular integrity.
2. Intracellular scaffolding proteins such as:
-Zonula occludens (ZO) proteins are members of the membrane-associated guanylate kinase (MAGUK) family and serve as intracellular scaffolding proteins that place TJ transmembrane proteins (claudins, occludin, JAMs, tricellulin) to the actin cytoskeleton, stabilize TJ structure and mediate signaling.
-Associated (cytoskeletal) proteins actin and myosin filaments in the cytoskeleton dynamically regulate TJ opening/closing via phosphorylation responding to mechanical and biochemical cues.

Now here's how you can improve the function of tight junctions in a nutshell:
Number 1: If you have any inflammatory condition such as MCAS you need to take it into consideration.
Number 2: Eliminate gluten, sugar, alcohol, the overconsumption of high FODMAP foods, NSAIDs, PPIs, heavy metals and glyphosate.
Number 3: Relax.
As stated, cortisol disrupts TJs by dysregulating the HPA axis and it also activates MLCK.
Number 4: Go to sleep and get sun.
Poor sleep and CR disrupt TJ protein expression while sunlight and vitamin D upregulates it.
Number 5: Provide enough zinc (stabilizes TJs), L glutamine (enhances TJ protein expression), retinol and polyphenols.
Number 6: Pick the following probiotic that works best for you:
-Lactobacillus rhamnosus GG.
-Bifidobacterium longum.
-Saccharomyces boulardii.
If these do not work for you or you can't use them, consider:
-Quercetin
-Curcumin NAC can also help in the specific context of people with Chrohn's
-DGL
Number 1: If you have any inflammatory condition such as MCAS you need to take it into consideration.
Number 2: Eliminate gluten, sugar, alcohol, the overconsumption of high FODMAP foods, NSAIDs, PPIs, heavy metals and glyphosate.
Number 3: Relax.
As stated, cortisol disrupts TJs by dysregulating the HPA axis and it also activates MLCK.
Number 4: Go to sleep and get sun.
Poor sleep and CR disrupt TJ protein expression while sunlight and vitamin D upregulates it.
Number 5: Provide enough zinc (stabilizes TJs), L glutamine (enhances TJ protein expression), retinol and polyphenols.
Number 6: Pick the following probiotic that works best for you:
-Lactobacillus rhamnosus GG.
-Bifidobacterium longum.
-Saccharomyces boulardii.
If these do not work for you or you can't use them, consider:
-Quercetin
-Curcumin NAC can also help in the specific context of people with Chrohn's
-DGL
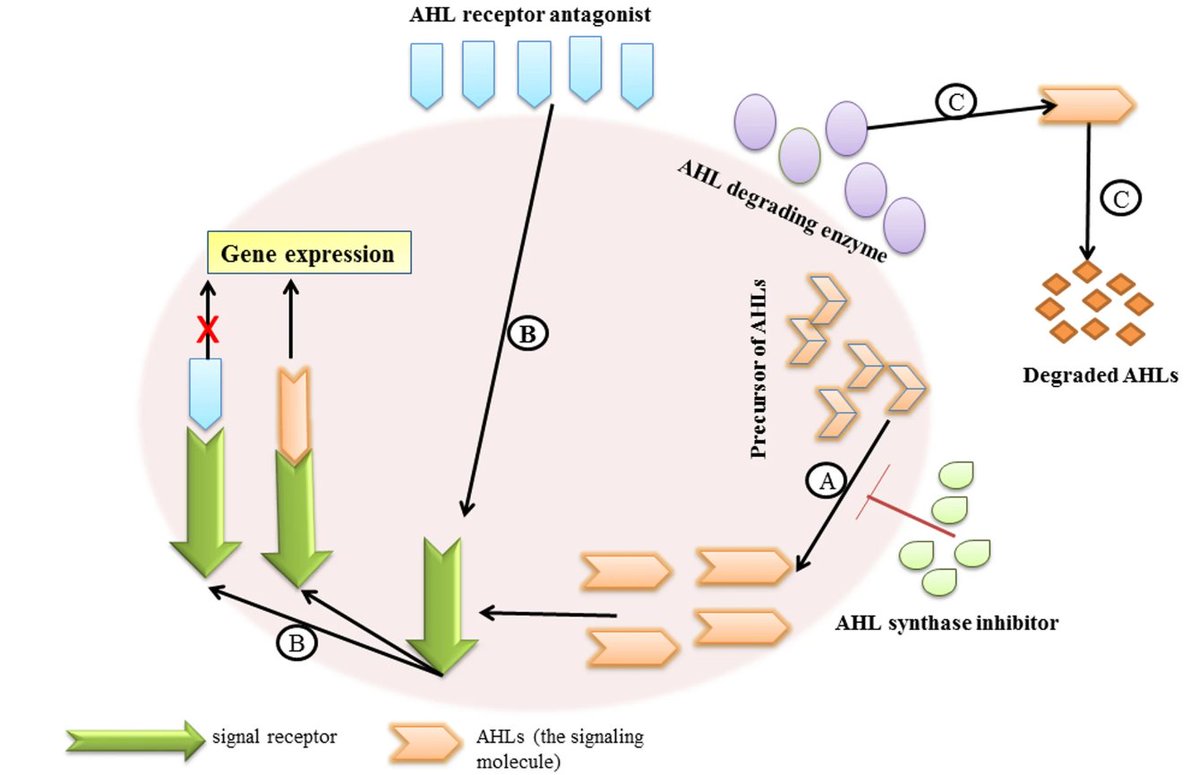
Then start working on biofilms.
Biofilms are organized “groups” of microorganisms such as bacteria, fungi, archaea, or protozoa commonly formed in the gut, oral cavity and sinuses.
They are embedded in a self-produced extracellular matrix composed of polysaccharides, proteins, and extracellular DNA (eDNA) that acts as a physical barrier and makes them highly resistant to antibiotics and antifungals.
Biofilm formation starts with planktonic microbes adhering to a surface through something called van der Waals forces or specific adhesins, then microbes start producing matrix components. T
hen the maturation process begins where cell division and matrix expansion form microcolonies starts and finally three-dimensional structures develop, with channels for nutrient flow.
This process is regulated by quorum sensing which is a cell-to-cell communication system using signaling molecules to coordinate gene expression, enhancing virulence and resistance.
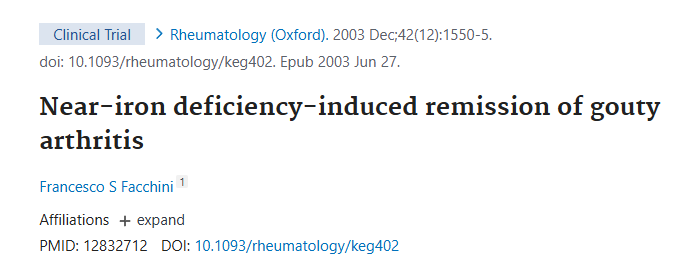
The three biofilm disruptors with the least chances of backfiring include:
1. Apolactoferrin
Lactoferrin comes in two forms:
-Native lactoferrin
-Apolactoferrin
Both can be quite valuable but the first one is iron bound and the second one is not which allows it to deprive pathogens of iron and thus helping us actually starve iron-dependent pathogens like candida albicans.
It also prevents pathogens from adhering to surfaces by interfering with adhesins and inhibits quorum sensing.
It also seems to be better tolerated from people who experience discomfort from things such as NAC and bromelain.
And it can of course help people who have hereditary hemochromatosis and find that even though flavonoids help their markers and some symptoms, they lower their libido too much.
2. L. reuteri DSM 17938, ATCC PTA 5289.
These are suggested since they produce reuterin that has broad-spectrum antimicrobial properties that can also disrupt EPS, competes for adhesion sites and inhibits quorum-sensing pathways.
3. Curcumin.
This one inhibits quorum sensing and disrupts bacterial cell membranes as well.
Other ones that can help include: NAC, berberine, garlic extract, bromelain and serrapeptase
Biofilms are organized “groups” of microorganisms such as bacteria, fungi, archaea, or protozoa commonly formed in the gut, oral cavity and sinuses.
They are embedded in a self-produced extracellular matrix composed of polysaccharides, proteins, and extracellular DNA (eDNA) that acts as a physical barrier and makes them highly resistant to antibiotics and antifungals.
Biofilm formation starts with planktonic microbes adhering to a surface through something called van der Waals forces or specific adhesins, then microbes start producing matrix components. T
hen the maturation process begins where cell division and matrix expansion form microcolonies starts and finally three-dimensional structures develop, with channels for nutrient flow.
This process is regulated by quorum sensing which is a cell-to-cell communication system using signaling molecules to coordinate gene expression, enhancing virulence and resistance.
The three biofilm disruptors with the least chances of backfiring include:
1. Apolactoferrin
Lactoferrin comes in two forms:
-Native lactoferrin
-Apolactoferrin
Both can be quite valuable but the first one is iron bound and the second one is not which allows it to deprive pathogens of iron and thus helping us actually starve iron-dependent pathogens like candida albicans.
It also prevents pathogens from adhering to surfaces by interfering with adhesins and inhibits quorum sensing.
It also seems to be better tolerated from people who experience discomfort from things such as NAC and bromelain.
And it can of course help people who have hereditary hemochromatosis and find that even though flavonoids help their markers and some symptoms, they lower their libido too much.
2. L. reuteri DSM 17938, ATCC PTA 5289.
These are suggested since they produce reuterin that has broad-spectrum antimicrobial properties that can also disrupt EPS, competes for adhesion sites and inhibits quorum-sensing pathways.
3. Curcumin.
This one inhibits quorum sensing and disrupts bacterial cell membranes as well.
Other ones that can help include: NAC, berberine, garlic extract, bromelain and serrapeptase
After some weeks, nuke, bind and manage die offs.
This is where antifungals such as carplilic acid, sodium caprylate, molybdenum, berberine, ceylon cinnamon, blackseed oil paired with prokinetics such as ginger and binder such as activated charcoal come into play.
Disclaimer: If you do everything else right, you really should feel die off with small amounts of these.
If not (and i've seen this happen) the tips that were addressed so far might actually have already taken care of the overgrowth so consider taking the tests again.
This is where antifungals such as carplilic acid, sodium caprylate, molybdenum, berberine, ceylon cinnamon, blackseed oil paired with prokinetics such as ginger and binder such as activated charcoal come into play.
Disclaimer: If you do everything else right, you really should feel die off with small amounts of these.
If not (and i've seen this happen) the tips that were addressed so far might actually have already taken care of the overgrowth so consider taking the tests again.

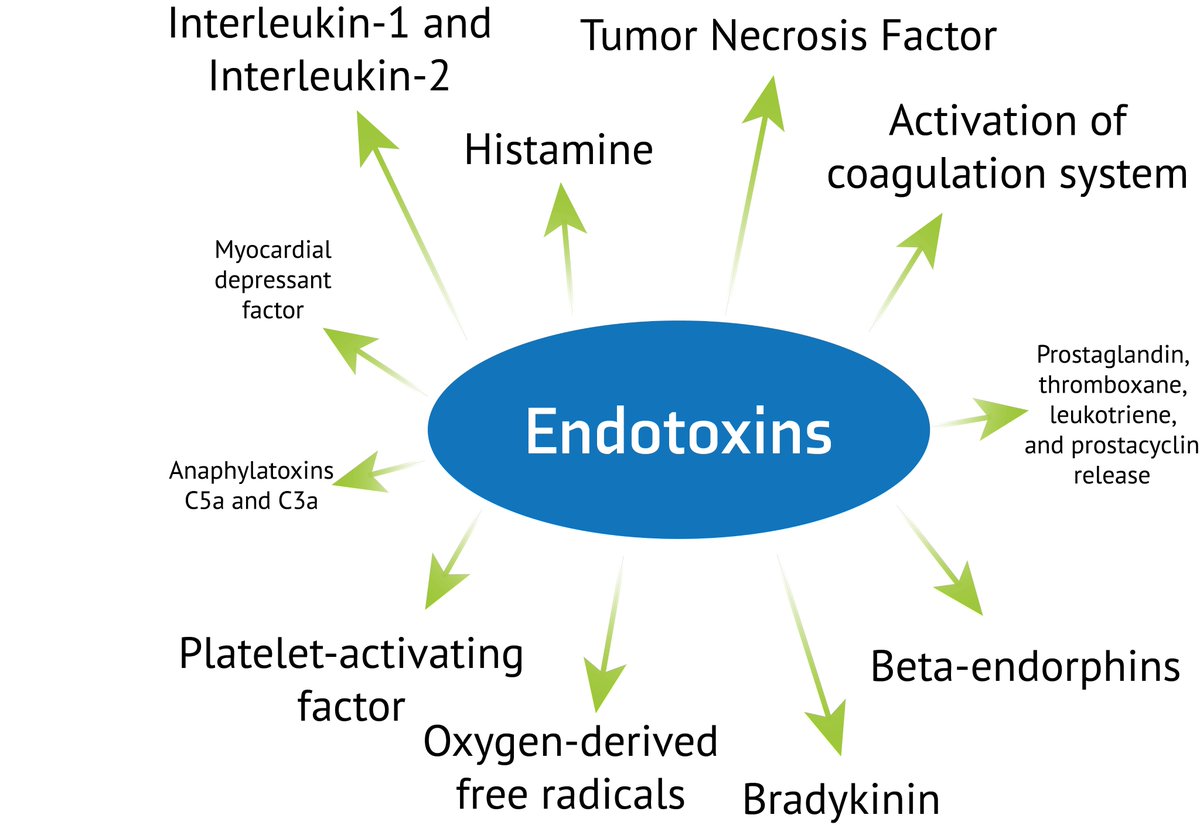
When it comes to die offs, antimicrobial or antifungal therapies can often trigger a Jarisch-Herxheimer reaction or "die-off" with symptoms that can range from nausea, headaches, slight fevers, fatigue, rashes, feelings of histamine intolerance and so on.
This reaction occurs during rapid pathogen death and includes the release of microbial components such as:
-Lipopolysaccharides (LPS).
Endotoxins from gram-negative bacteria activate the toll-like receptor 4 on immune cells, triggering nuclear factor-kappa B (NF-κB) signaling and the release of pro-inflammatory cytokines such as interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α) and interleukin-1β (IL-1β).
-β-Glucans and Mannoproteins.
Fungal cell wall components from Candida species stimulate dectin-1 receptors on macrophages, further activating NF-κB and cytokine release.
-Acetaldehyde and ethanol.
These are metabolic byproducts of Candida and certain bacteria that cause oxidative stress and neurotoxicity.
-Nucleic acids and proteins.
These are released during microbial lysis, these act as damage-associated molecular patterns (DAMPs), perpetuating immune activation through pattern recognition receptors (PRRs).
Now the intensity of die-off is influences by the:
Microbial loads (severe SIBO with >10^5 CFU/mL will release more toxins than a minor case for example)
The person’s detoxification capacity.
Impaired phase I (cytochrome P450) and phase II (conjugation) liver detoxification pathways will obviously harm the person’s ability to detox these products.
The states of his immune system.
Overactive Th1/Th17 responses or mast cell activation syndrome (MCAS) amplify inflammatory responses for example.
His gut barrier integrity.
A leaky gut, allows greater translocation of toxins into systemic circulation.
So it’s vital to follow every process that’s presented in this thread step by step and taking your time with hit especially considering that some die offs can last days.
This reaction occurs during rapid pathogen death and includes the release of microbial components such as:
-Lipopolysaccharides (LPS).
Endotoxins from gram-negative bacteria activate the toll-like receptor 4 on immune cells, triggering nuclear factor-kappa B (NF-κB) signaling and the release of pro-inflammatory cytokines such as interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α) and interleukin-1β (IL-1β).
-β-Glucans and Mannoproteins.
Fungal cell wall components from Candida species stimulate dectin-1 receptors on macrophages, further activating NF-κB and cytokine release.
-Acetaldehyde and ethanol.
These are metabolic byproducts of Candida and certain bacteria that cause oxidative stress and neurotoxicity.
-Nucleic acids and proteins.
These are released during microbial lysis, these act as damage-associated molecular patterns (DAMPs), perpetuating immune activation through pattern recognition receptors (PRRs).
Now the intensity of die-off is influences by the:
Microbial loads (severe SIBO with >10^5 CFU/mL will release more toxins than a minor case for example)
The person’s detoxification capacity.
Impaired phase I (cytochrome P450) and phase II (conjugation) liver detoxification pathways will obviously harm the person’s ability to detox these products.
The states of his immune system.
Overactive Th1/Th17 responses or mast cell activation syndrome (MCAS) amplify inflammatory responses for example.
His gut barrier integrity.
A leaky gut, allows greater translocation of toxins into systemic circulation.
So it’s vital to follow every process that’s presented in this thread step by step and taking your time with hit especially considering that some die offs can last days.

Supplements that can help you mitigate die-off symptoms by reducing inflammation, binding toxins and enhancing detoxification include:
-Activated charcoal (start with just 500mg 2 hours before or after your meals and medications).
This one absorbs LPS, acetaldehyde and mycotoxins due to its porous structure.
-Bentonite clay (start with just ½ a teaspoon on an empty stomach).
This one binds cationic toxins.
-N-Acetylcysteine (NAC) (start with just 300mg twice a day).
This one increases GSH synthesis and conjugates acetaldehyde while also inhibiting NF-κB.
-Milk thistle (Silymarin).
This one upregulates Nrf2.
-Quercetin.
This one inhibits mast cell degranulation and downregulates NF-κB.
-Pantethine.
This serves a s precursor to coenzyme A, supporting acetyl-CoA formation from acetate (it basically enhances phase II detoxification).
-Provide enough B3 (or NAD+ precursors such as NMN), molybdenum, magnesium and zinc to support ALDH/AOX activity.
-Thiamine (B1) can aso help by supporting pyruvate dehydrogenase and preventing acetaldehyde formation from pyruvate.
And finally after all these, remember to restore the balance.
This one will require testing in order to see if the overgrowth is at bay and tools such as glutamine, PEA, quercetin, tributyrin, colostrum, zinc, B2 and B1 can be used.
-Activated charcoal (start with just 500mg 2 hours before or after your meals and medications).
This one absorbs LPS, acetaldehyde and mycotoxins due to its porous structure.
-Bentonite clay (start with just ½ a teaspoon on an empty stomach).
This one binds cationic toxins.
-N-Acetylcysteine (NAC) (start with just 300mg twice a day).
This one increases GSH synthesis and conjugates acetaldehyde while also inhibiting NF-κB.
-Milk thistle (Silymarin).
This one upregulates Nrf2.
-Quercetin.
This one inhibits mast cell degranulation and downregulates NF-κB.
-Pantethine.
This serves a s precursor to coenzyme A, supporting acetyl-CoA formation from acetate (it basically enhances phase II detoxification).
-Provide enough B3 (or NAD+ precursors such as NMN), molybdenum, magnesium and zinc to support ALDH/AOX activity.
-Thiamine (B1) can aso help by supporting pyruvate dehydrogenase and preventing acetaldehyde formation from pyruvate.
And finally after all these, remember to restore the balance.
This one will require testing in order to see if the overgrowth is at bay and tools such as glutamine, PEA, quercetin, tributyrin, colostrum, zinc, B2 and B1 can be used.
That's all.
I hope that you found something useful in this thread, if you did, make sure to leave a like/RT.
I hope that you found something useful in this thread, if you did, make sure to leave a like/RT.
https://x.com/Helios_Movement/status/1938157311576408439
And if you want more details when it comes to gut issues, detailed meal plans and so on, you can go here:
fitandball.gumroad.com/l/uftii/gut45
fitandball.gumroad.com/l/uftii/gut45
• • •
Missing some Tweet in this thread? You can try to
force a refresh