1/Time to go with the flow!
Hoping no one notices you don’t know the anatomy of internal carotid (ICA)?
Do you say “carotid siphon” & hope no one asks for more detail?
Here’s a thread to help you siphon off some information about ICA anatomy!
Hoping no one notices you don’t know the anatomy of internal carotid (ICA)?
Do you say “carotid siphon” & hope no one asks for more detail?
Here’s a thread to help you siphon off some information about ICA anatomy!

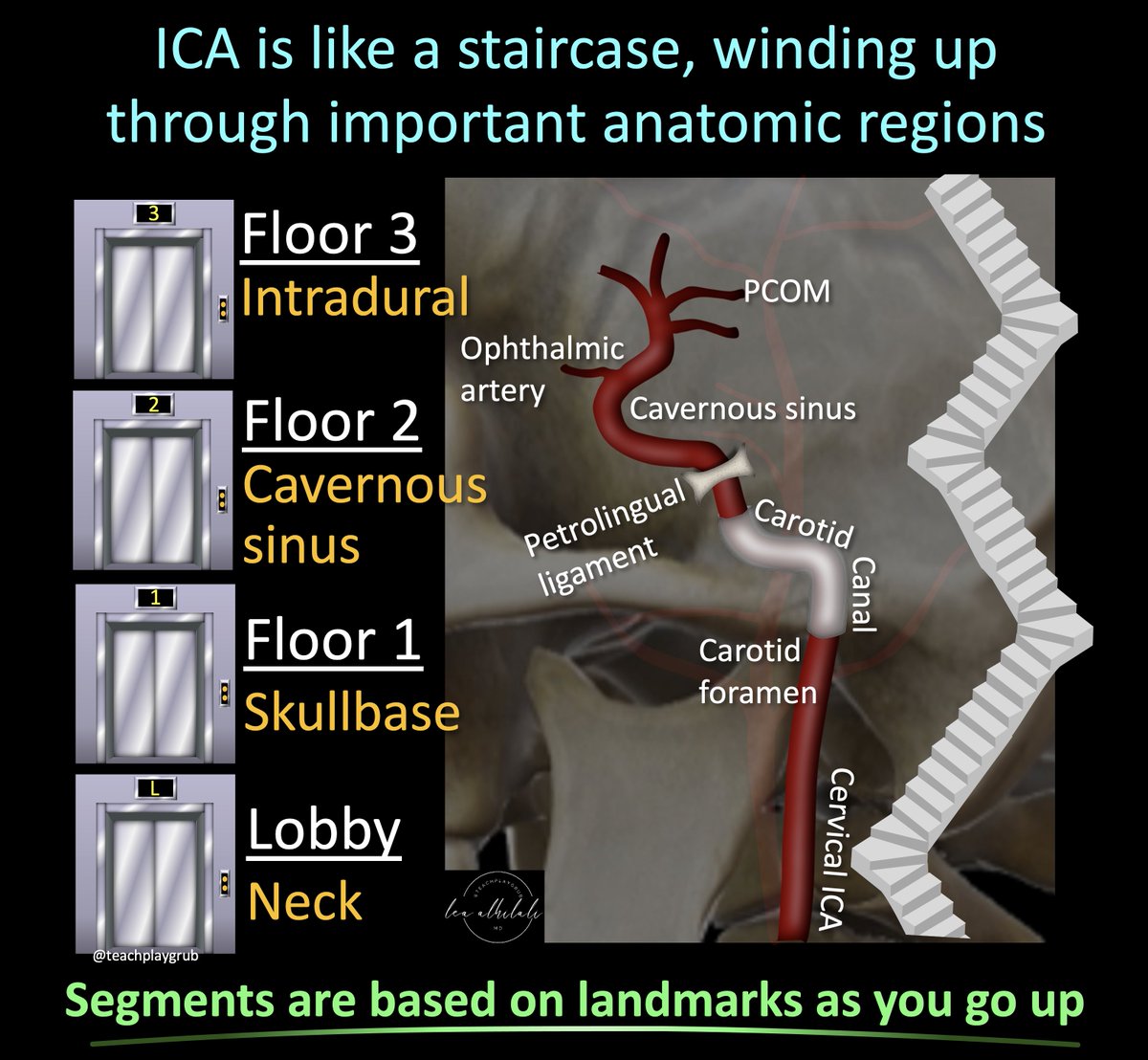
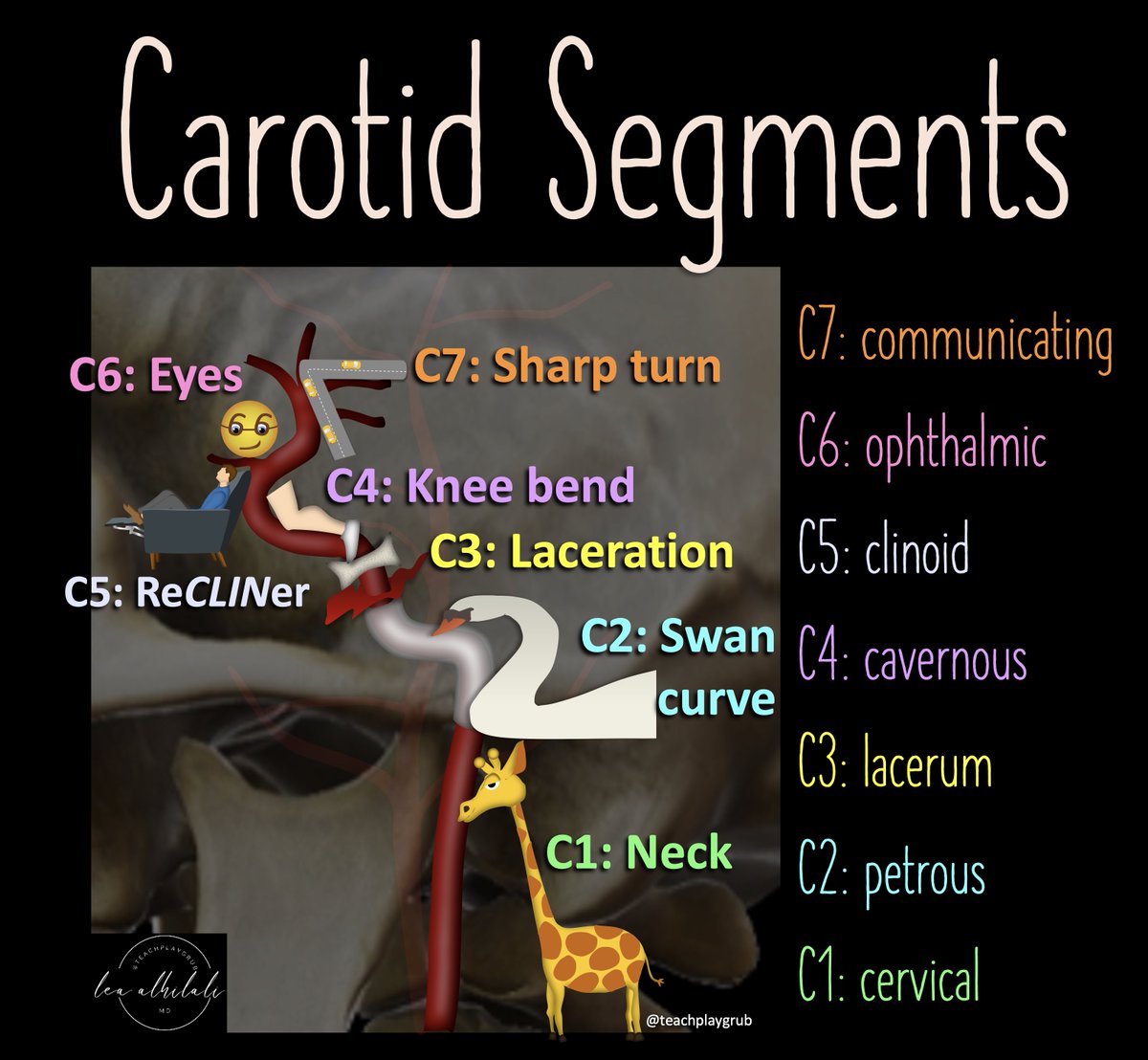
2/ICA is like a staircase—winding up through important anatomic regions like a staircase winding up to each floor Lobby is the neck.
First floor is skullbase/carotid canal. Next it stops at the cavernous sinus, before finally reaching the rooftop balcony of the intradural space.
First floor is skullbase/carotid canal. Next it stops at the cavernous sinus, before finally reaching the rooftop balcony of the intradural space.
3/ICA is divided into numbered segments based on landmarks that denote transitions on its way up the floors.
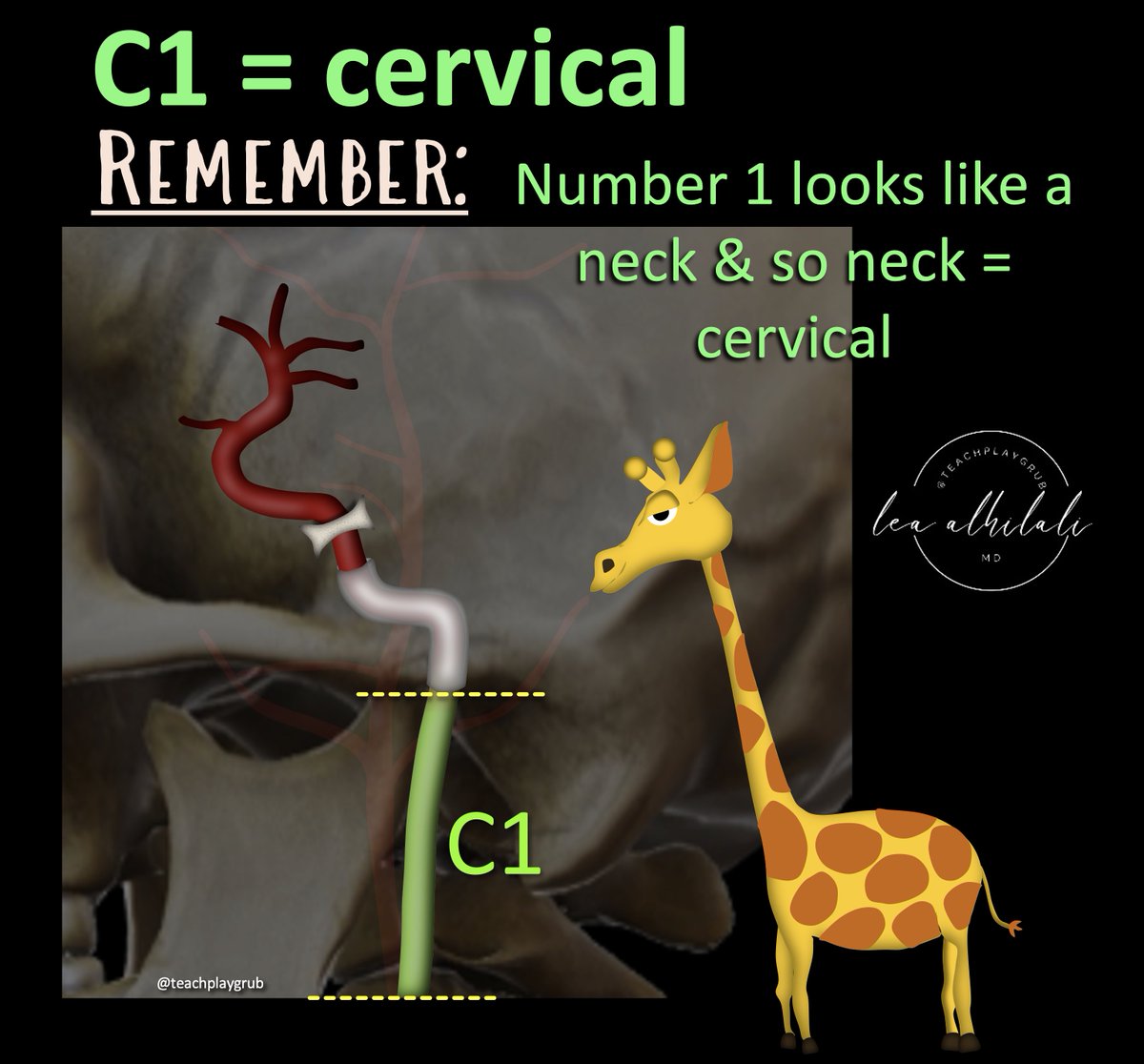
C1 is in the lobby or neck.
You can remember this b/c the number 1 looks elongated & straight like a neck.
C1 is in the lobby or neck.
You can remember this b/c the number 1 looks elongated & straight like a neck.
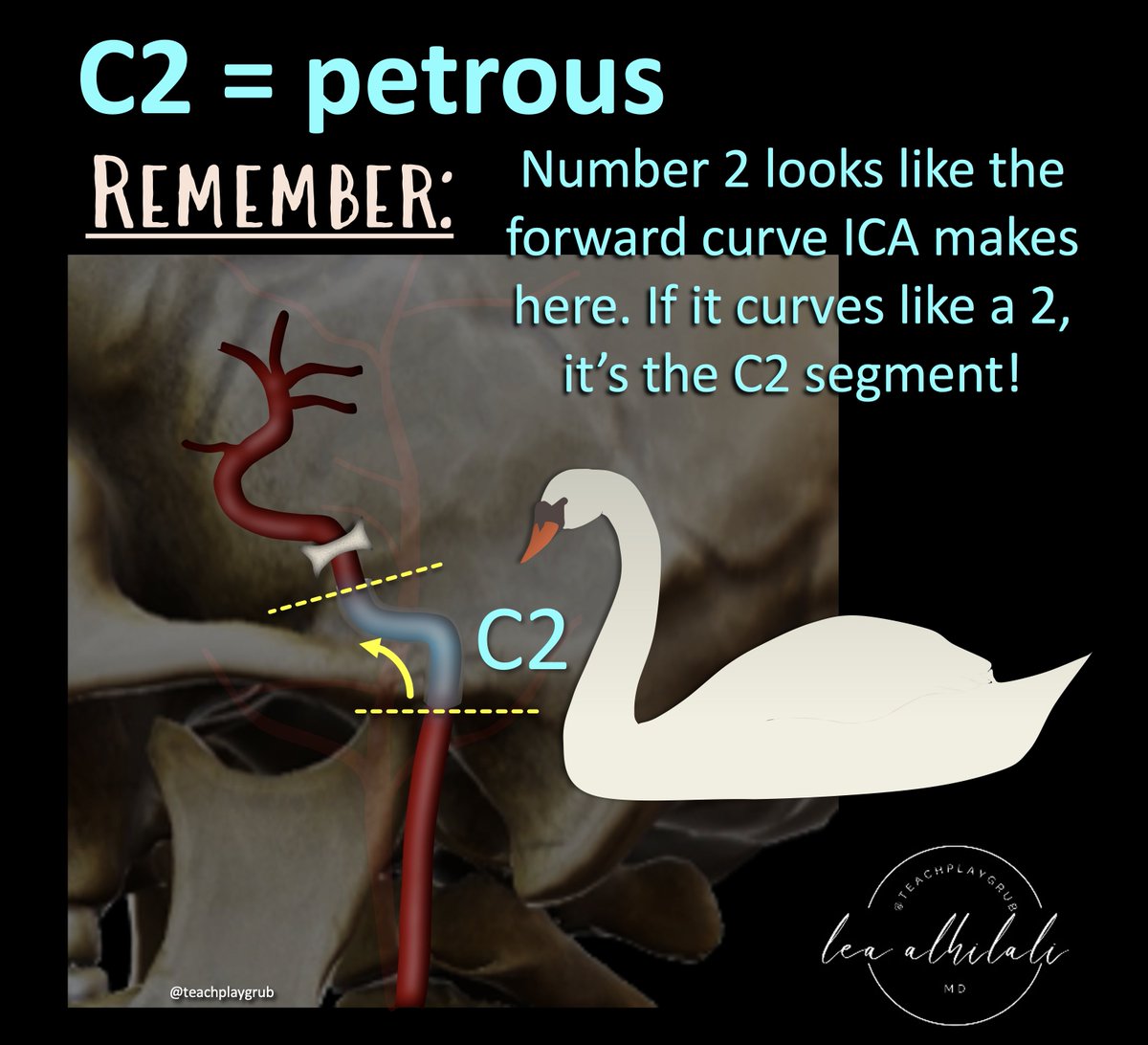
4/C2 is the petrous or horizontal segment. This is where the ICA gets to the next floor, the skullbase.
I remember this b/c the ICA makes a curve forward here, like a swan’s neck--and number 2 has a forward, swan like curve that looks just like the curve of the petrous segment.
I remember this b/c the ICA makes a curve forward here, like a swan’s neck--and number 2 has a forward, swan like curve that looks just like the curve of the petrous segment.
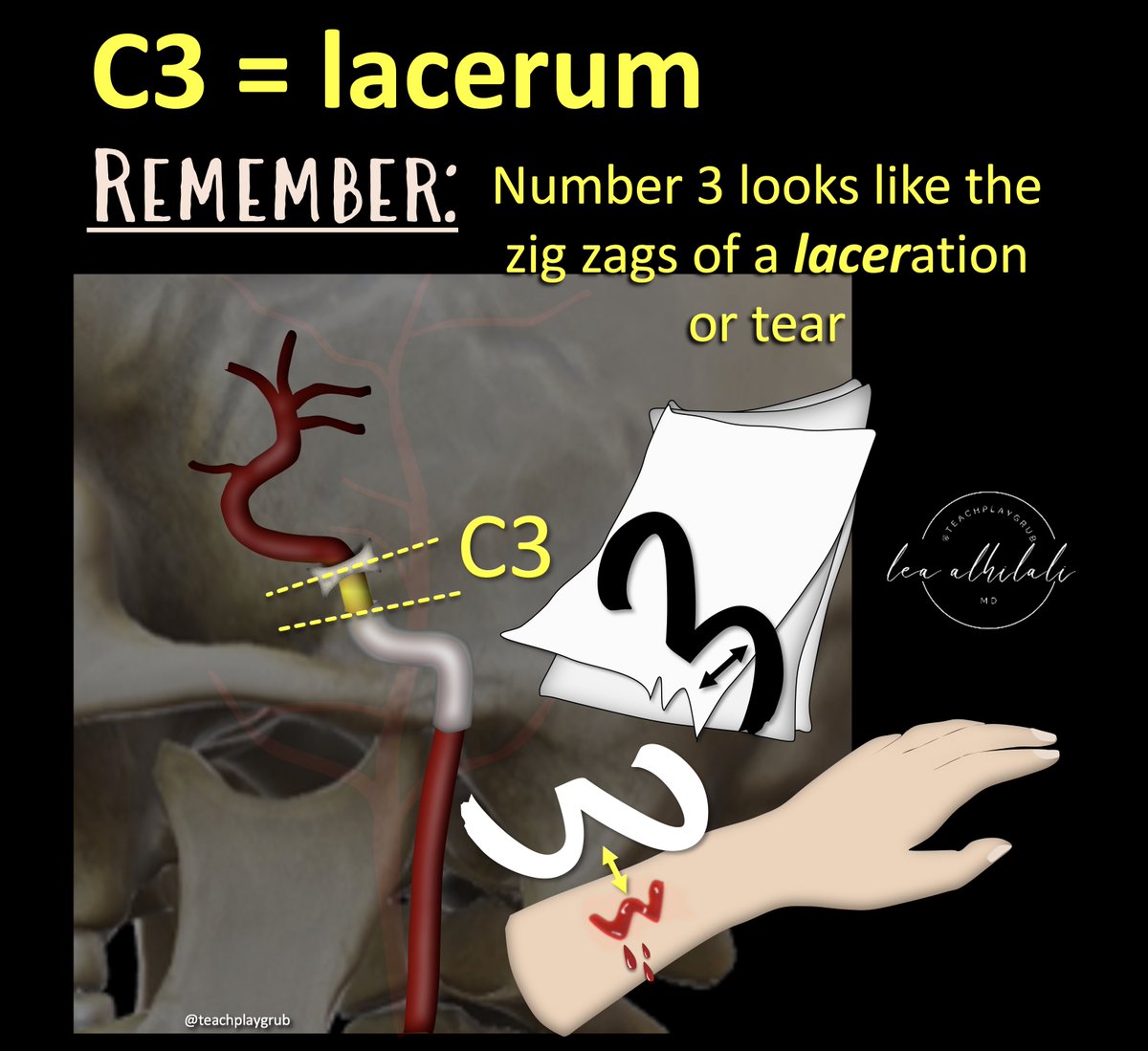
5/C3 is the lacerum segment—from above foramen lacerum to petrolingual ligament.
It’s easy to remember b/c lacerum comes from the Latin word for torn (b/c foramen lacerum is irregular like a tear or laceration)
Number 3 zig zags like a laceration or torn edge, so C3 = lacerum
It’s easy to remember b/c lacerum comes from the Latin word for torn (b/c foramen lacerum is irregular like a tear or laceration)
Number 3 zig zags like a laceration or torn edge, so C3 = lacerum
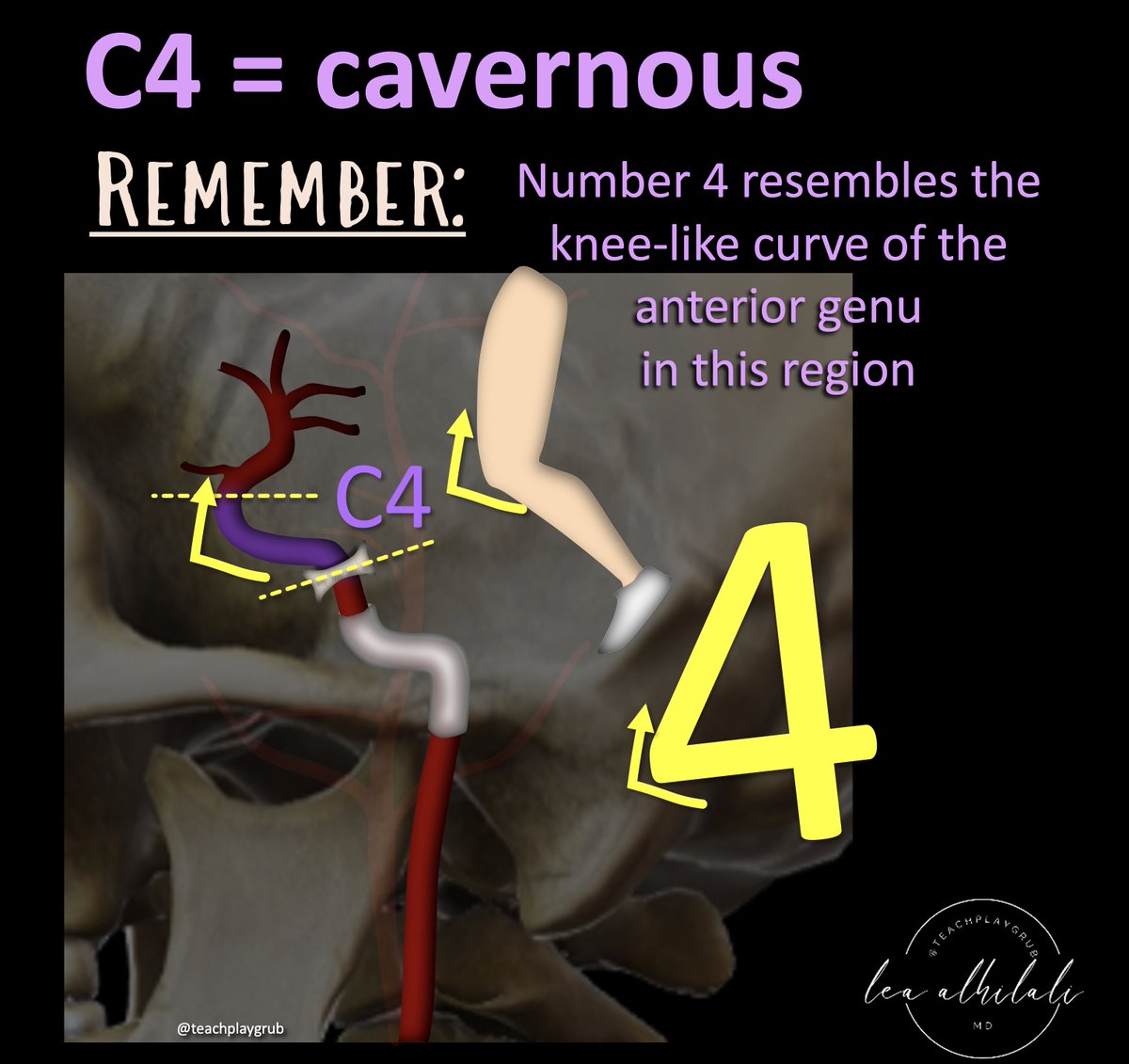
6/C4 is the cavernous segment
Cavernous segment has the anterior genu. Here, the ICA makes a curve back, so it looks like a knee (genu is Latin for knee)
You can remember C4 is cavernous b/c the number 4 has a curve back like the anterior genu of the cavernous ICA, like a knee.
Cavernous segment has the anterior genu. Here, the ICA makes a curve back, so it looks like a knee (genu is Latin for knee)
You can remember C4 is cavernous b/c the number 4 has a curve back like the anterior genu of the cavernous ICA, like a knee.
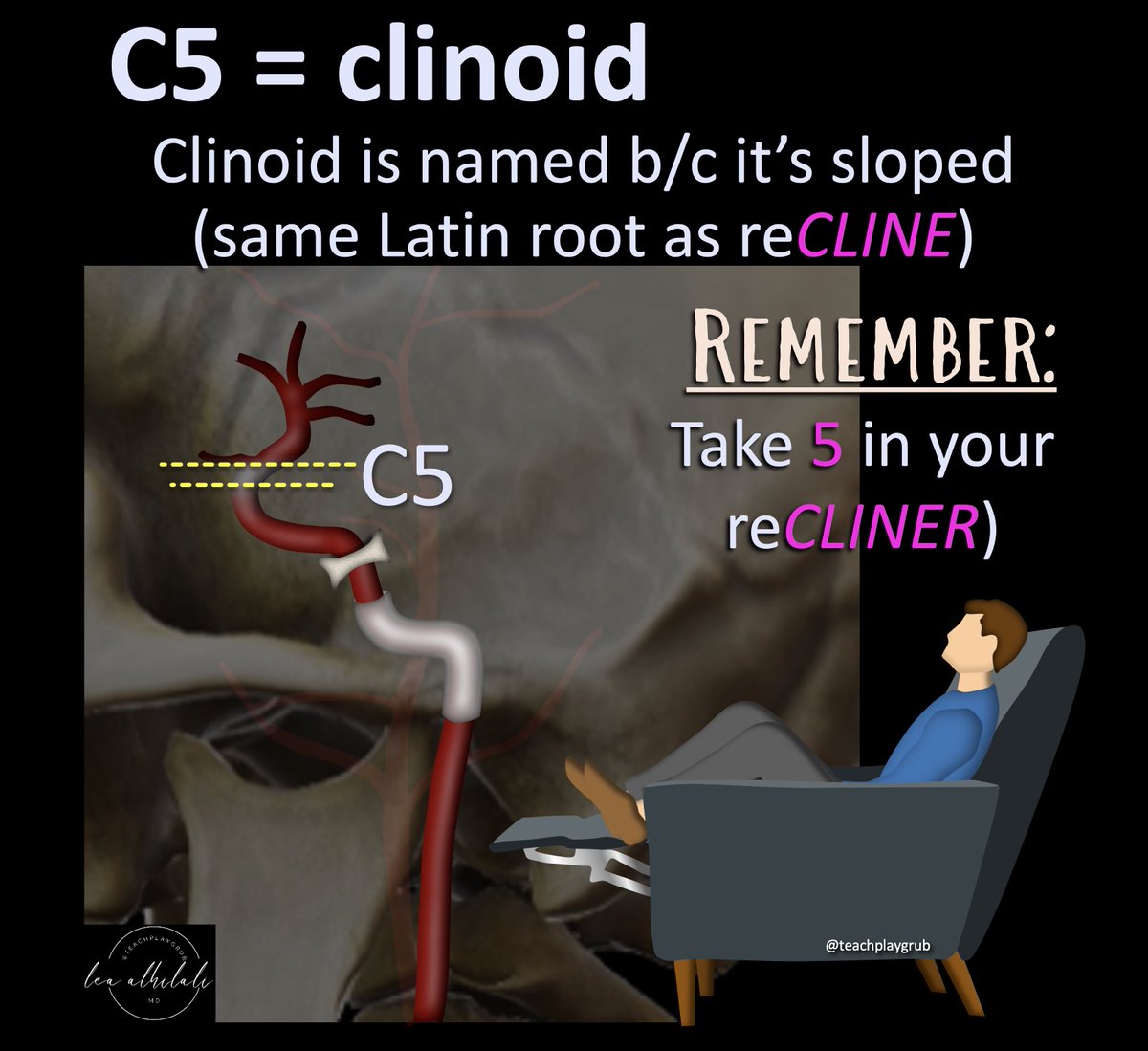
7/C5 is the clinoid segment—at the ant. clinoid process
Clinoid process gets its name from its sloped shape. It’s from the same Latin root as recline (CLIN)
And we all take a break (take five some might say😉) by sitting back or reclining.
Take FIVE & reCLINE. C5 is CLINoid.
Clinoid process gets its name from its sloped shape. It’s from the same Latin root as recline (CLIN)
And we all take a break (take five some might say😉) by sitting back or reclining.
Take FIVE & reCLINE. C5 is CLINoid.
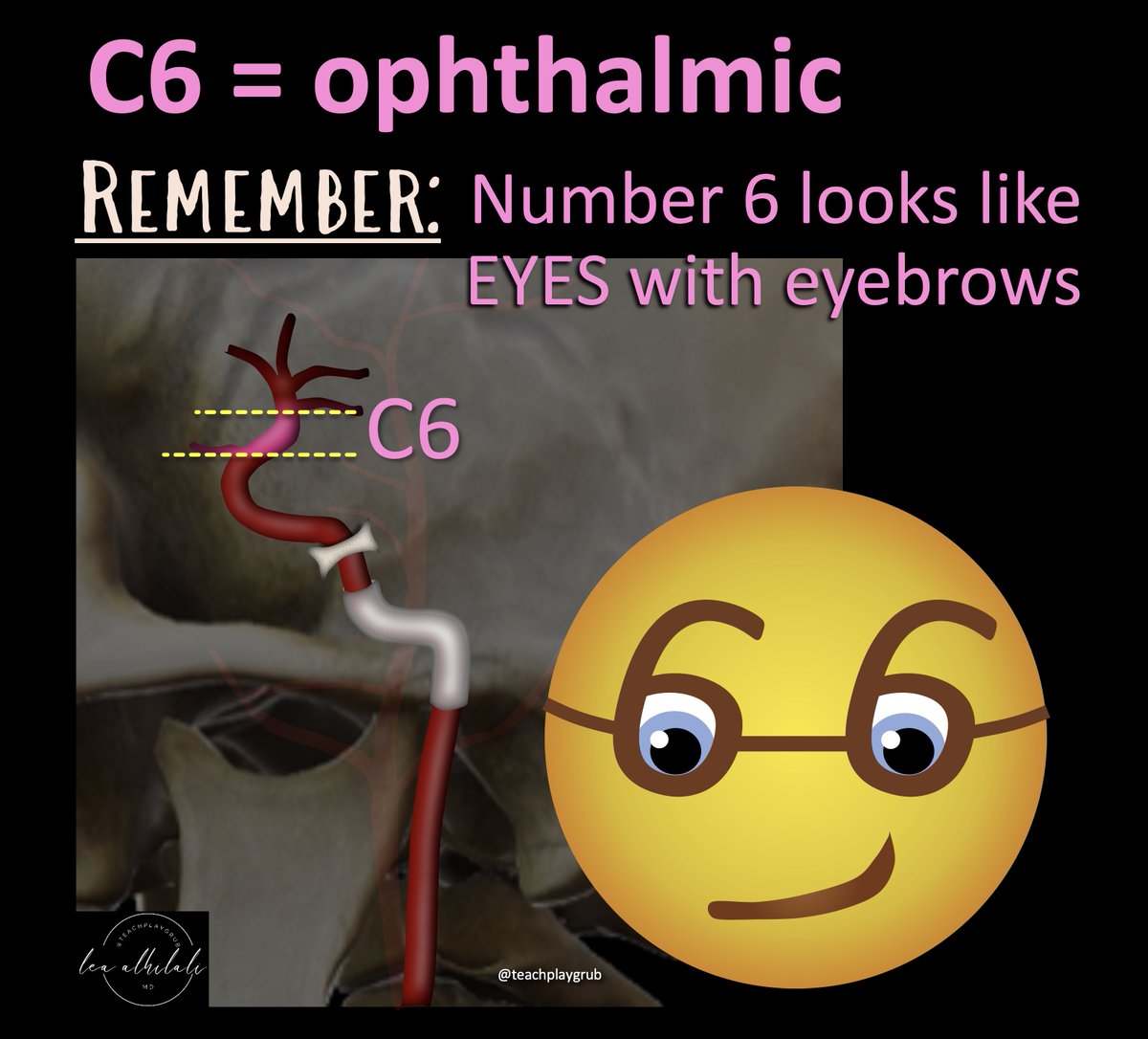
8/C6 is the ophthalmic segment.
I remember this b/c the circle of the number 6 looks like eyes and its curve looks like eyebrows.
So, 6 is an eye = ophthalmic
I remember this b/c the circle of the number 6 looks like eyes and its curve looks like eyebrows.
So, 6 is an eye = ophthalmic
9/C7 is the communicating or terminal segment.
You can remember this bc the number 7 looks like the ICA ending & giving off the PCOMM.
The number 7 has the shape of a turn off right before the road ends—& the ICA gives off the PCOMM in its C7 segment right before terminating.
You can remember this bc the number 7 looks like the ICA ending & giving off the PCOMM.
The number 7 has the shape of a turn off right before the road ends—& the ICA gives off the PCOMM in its C7 segment right before terminating.

10/Now you can remember all the segments of the ICA!
Hopefully this will help you to be precise in your localization and siphon away the term “carotid siphon”!!
Hopefully this will help you to be precise in your localization and siphon away the term “carotid siphon”!!
• • •
Missing some Tweet in this thread? You can try to
force a refresh






















