1/Talk about bad blood!
Do you know when a hematoma is going to expand?
Read on for month’s @theAJNR SCANtastic on all you need to know about imaging intracranial hemorrhage!
ajnr.org/content/46/7/1…
Do you know when a hematoma is going to expand?
Read on for month’s @theAJNR SCANtastic on all you need to know about imaging intracranial hemorrhage!
ajnr.org/content/46/7/1…
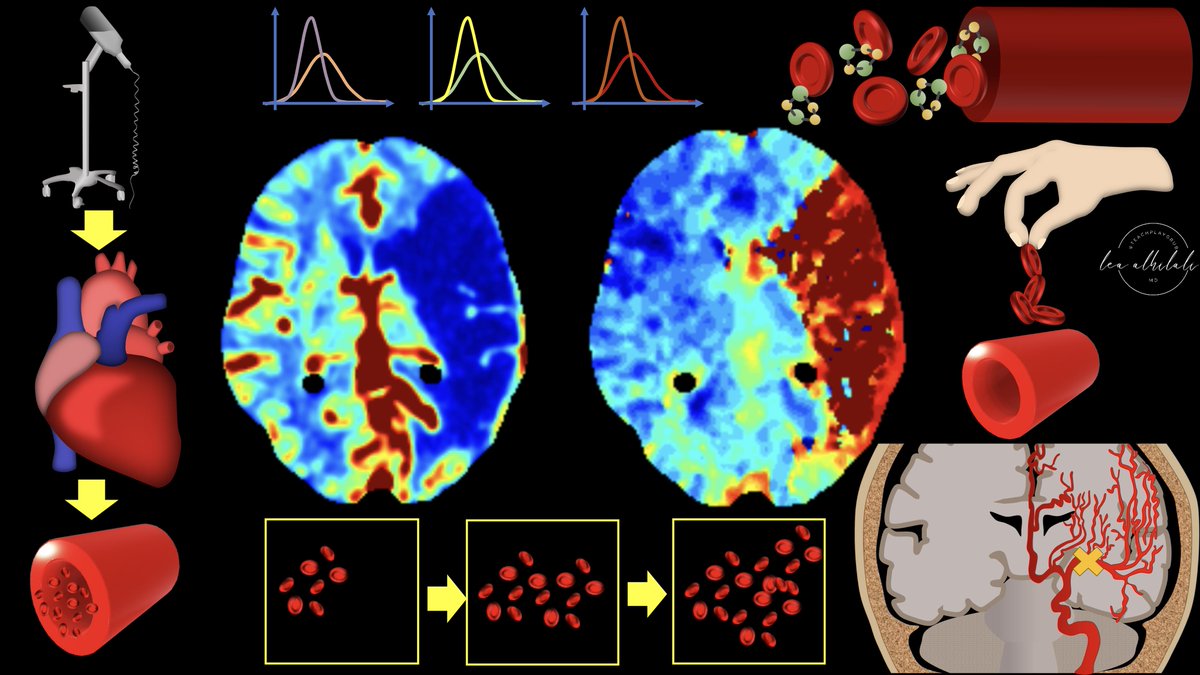
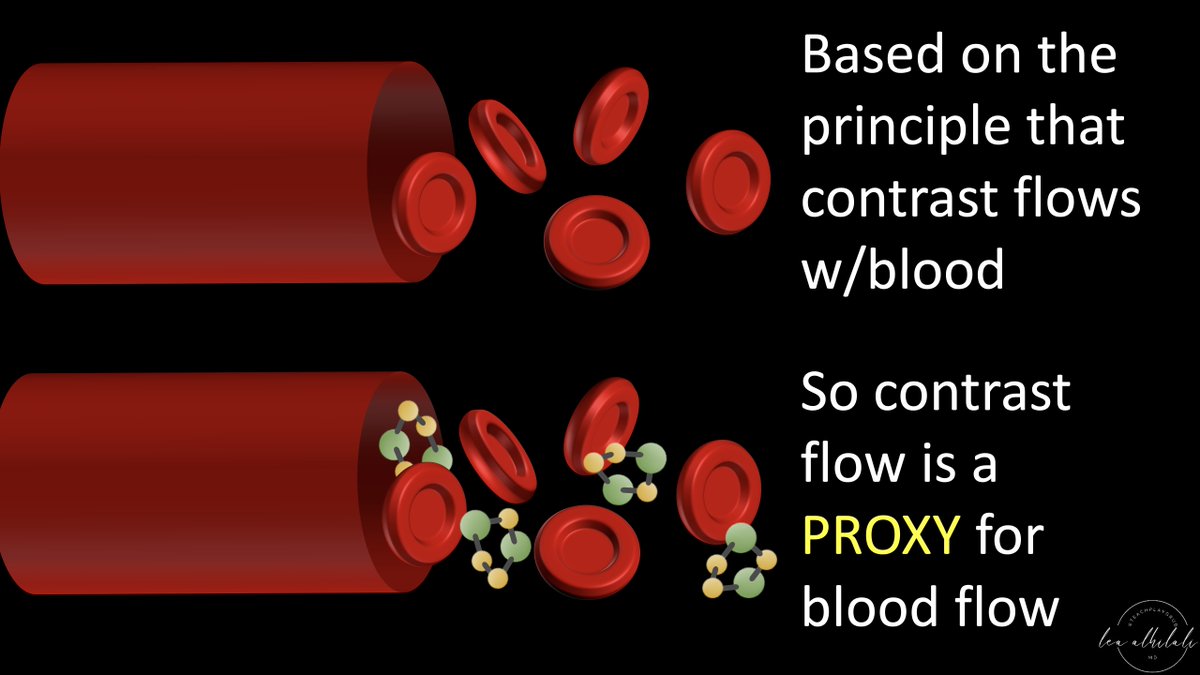
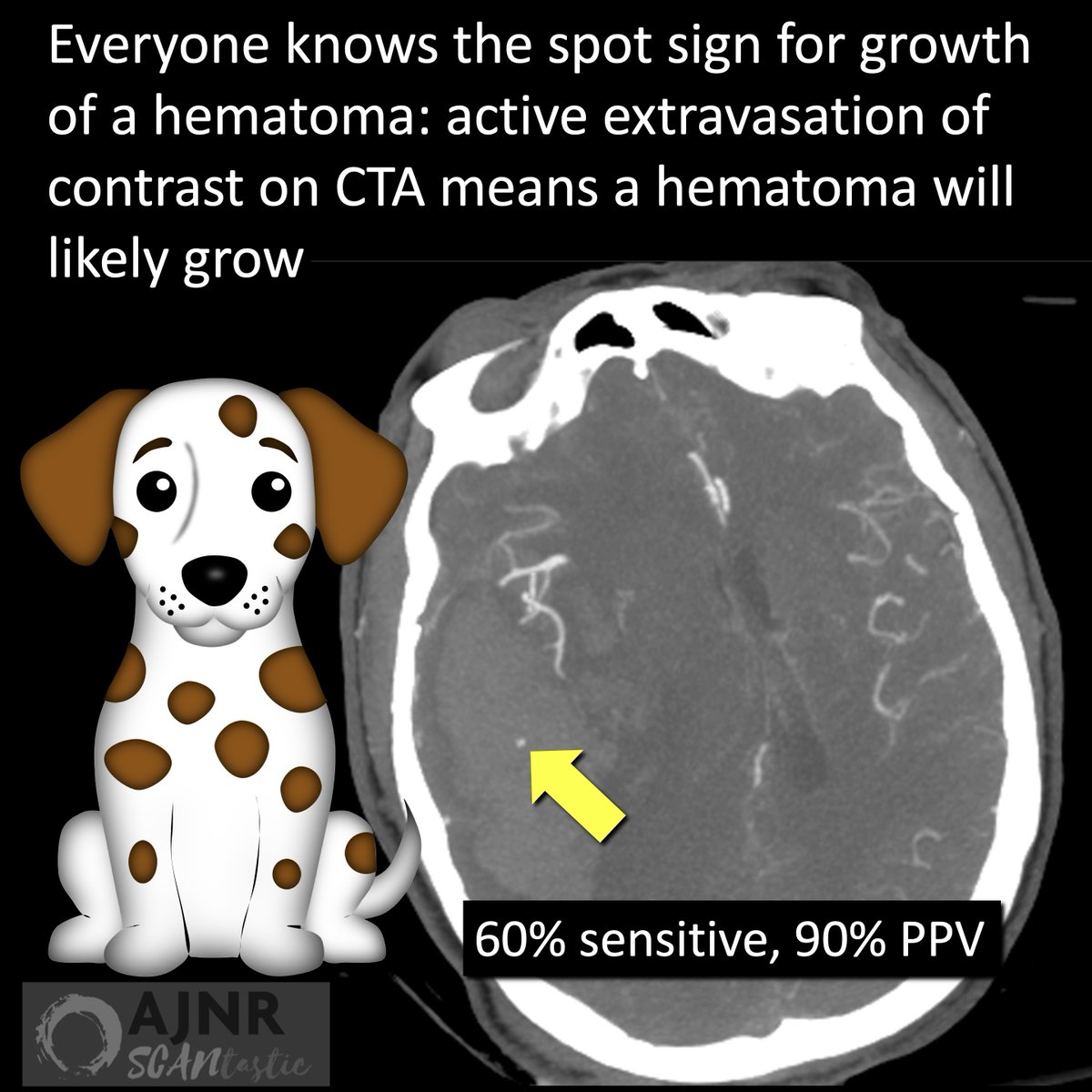
@TheAJNR 2/Everyone knows about the spot sign for intracranial hemorrhage
It’s when arterial contrast is seen within a hematoma on CTA, indicating active
extravasation of contrast into the hematoma.
But what if you want to know before the CTA?
It’s when arterial contrast is seen within a hematoma on CTA, indicating active
extravasation of contrast into the hematoma.
But what if you want to know before the CTA?
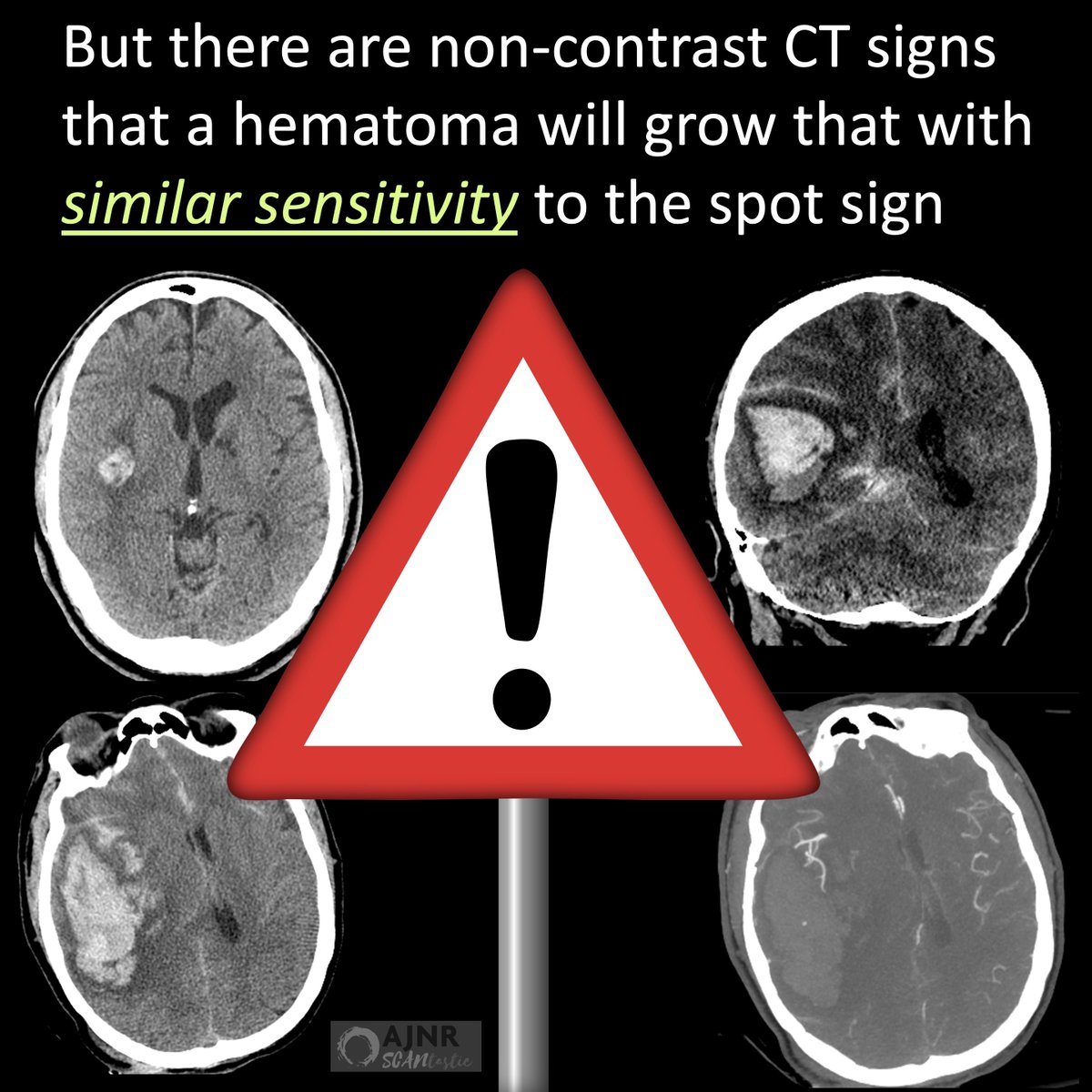
@TheAJNR 3/Turns out there are non-contrast head CT signs that a hematoma may expand that perform similarly to the spot sign—and together can be very accurate.
How can you remember what they are?
How can you remember what they are?
@TheAJNR 4/If you are wondering if a hematoma will expand, look for the same features as the
most expansive thing in the universe: a black hole.
There are many signs, but 3 best are also seen w/black holes
most expansive thing in the universe: a black hole.
There are many signs, but 3 best are also seen w/black holes
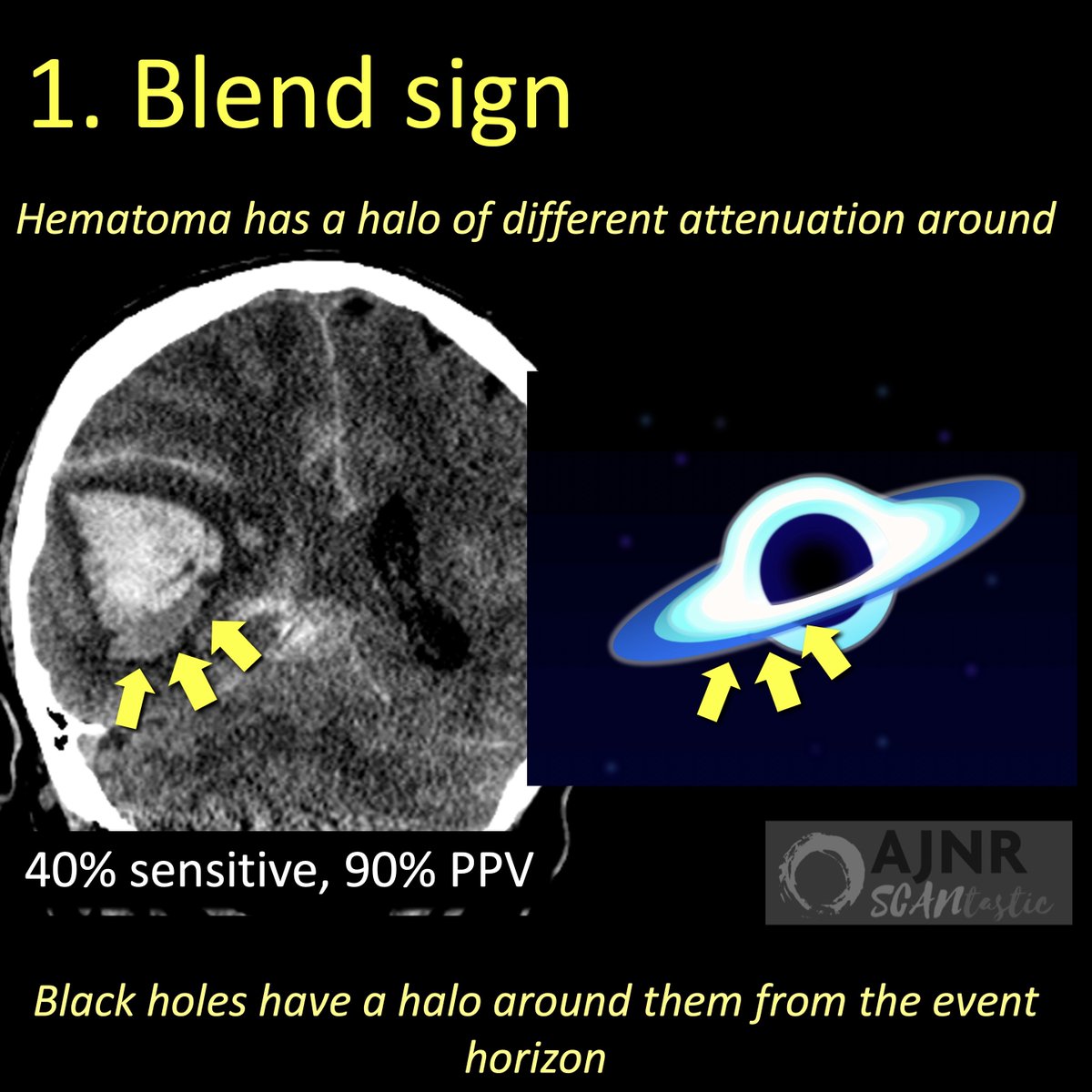
@TheAJNR 5/First is the blend sign
Here, part of the hematoma has a different attenuation, meaning different age blood & thus active bleeding
It looks like a halo & black holes have halos in the event horizon!
Here, part of the hematoma has a different attenuation, meaning different age blood & thus active bleeding
It looks like a halo & black holes have halos in the event horizon!
@TheAJNR 6/Next is the black hole sign
Here, regions have very low density, indicating unclotted blood similar to water density.
If blood is still flowing like water, then hematoma may expand
Black holes obviously have black holes too!
Here, regions have very low density, indicating unclotted blood similar to water density.
If blood is still flowing like water, then hematoma may expand
Black holes obviously have black holes too!

@TheAJNR 7/Finally is the island sign
Here, there are satellite hematomas, indicating multiple regions of bleeding, increasing risk of expansion
Black holes usually have satellites orbiting around them from their gravitational pull!
Here, there are satellite hematomas, indicating multiple regions of bleeding, increasing risk of expansion
Black holes usually have satellites orbiting around them from their gravitational pull!

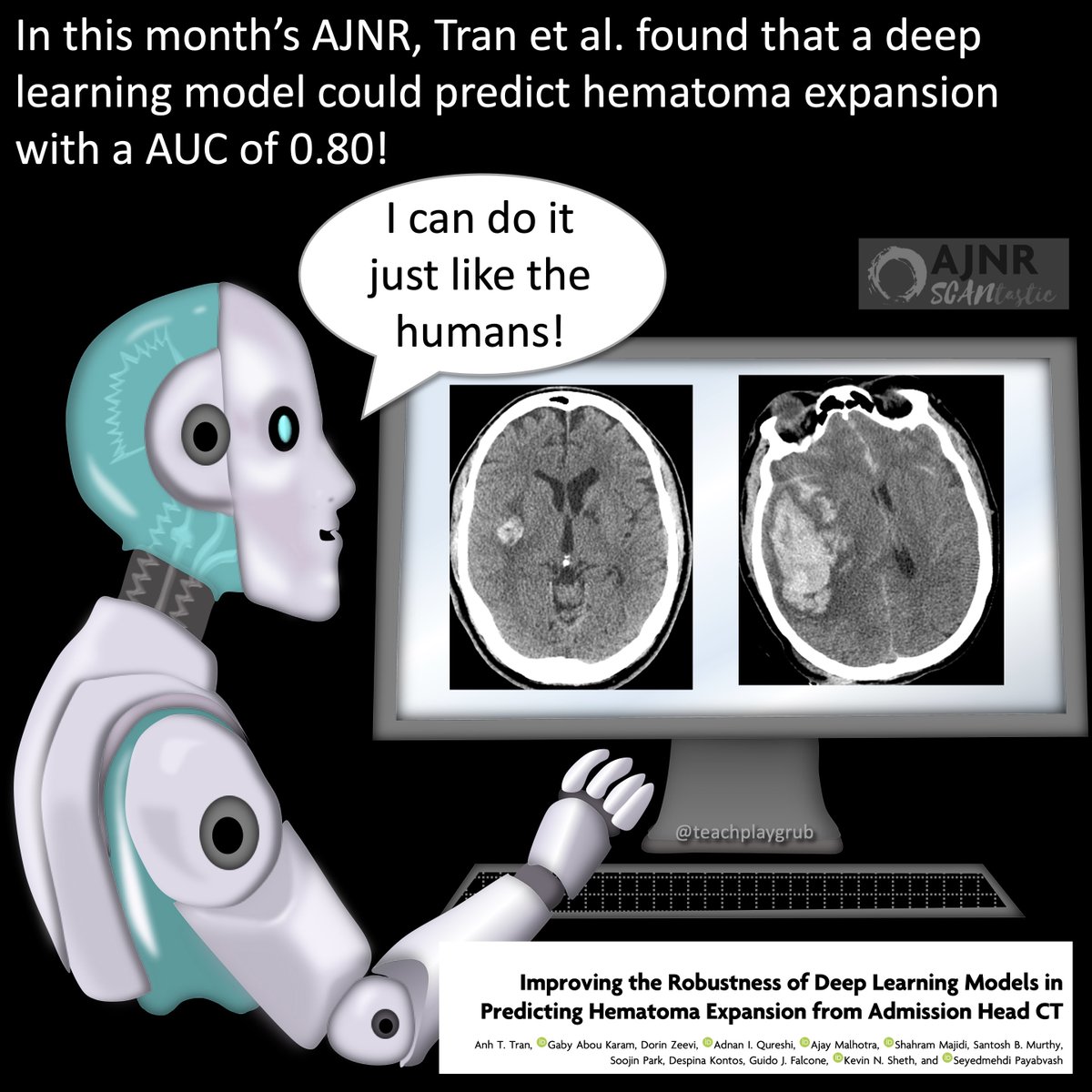
@TheAJNR 8/In this month’s @theAJNR Tran et al. worked to optimize a deep learning model that could predict hematoma expansion with an AUC of 0.8!
In the future, AI may make all these signs obsolete!!
In the future, AI may make all these signs obsolete!!
@TheAJNR 9/Now you know the imaging signs for hematoma expansion—until deep learning can assess it for you!
Hopefully, now you will know which clot is hot!
ajnr.org/content/46/7/1…
Hopefully, now you will know which clot is hot!
ajnr.org/content/46/7/1…

• • •
Missing some Tweet in this thread? You can try to
force a refresh