🧵 💡 “Sjögren’s Syndrome: Why Do So Many Trials Fail?”
From hydroxychloroquine to rituximab to belimumab — let’s walk through the key trials that shaped (and shook) pSS treatment.👇
#Sjögrens #RheumTwitter #MedTwitter @DurgaPrasannaM1 @IhabFathiSulima @NeuroSjogrens @SjogrensOrg @SjogrensCa @SarahSchaferMD @elisa_comer @SjogrensForum
From hydroxychloroquine to rituximab to belimumab — let’s walk through the key trials that shaped (and shook) pSS treatment.👇
#Sjögrens #RheumTwitter #MedTwitter @DurgaPrasannaM1 @IhabFathiSulima @NeuroSjogrens @SjogrensOrg @SjogrensCa @SarahSchaferMD @elisa_comer @SjogrensForum

1️⃣ JOQUER Trial – The HCQ Wake-Up Call
💊 Hydroxychloroquine — once used for fatigue, arthralgia, dryness.
🧪 JOQUER (NEJM 2014) showed:
❌ No significant benefit over placebo.
✅ Some trends for low-inflammatory patients.
Lesson? HCQ ≠ miracle drug in pSS.
💊 Hydroxychloroquine — once used for fatigue, arthralgia, dryness.
🧪 JOQUER (NEJM 2014) showed:
❌ No significant benefit over placebo.
✅ Some trends for low-inflammatory patients.
Lesson? HCQ ≠ miracle drug in pSS.
2️⃣ TEARS Trial – The Rituximab Reality Check
🧬 B-cell targeting made sense.
💉 Rituximab = logical next step.
👨🔬 TEARS trial (2013):
❌ No big win on fatigue or dryness
🟡 But systemic benefit signals emerged
Lesson? Choose patients wisely.
🧬 B-cell targeting made sense.
💉 Rituximab = logical next step.
👨🔬 TEARS trial (2013):
❌ No big win on fatigue or dryness
🟡 But systemic benefit signals emerged
Lesson? Choose patients wisely.
3️⃣ TRACTISS Trial – Double Down on RTX
🇬🇧 UK-based TRACTISS (2017) repeated the test.
💉 Again, no major relief for dryness
✅ Trends toward benefit in systemic features.
👀 Takeaway: RTX may help outside the glands.
🇬🇧 UK-based TRACTISS (2017) repeated the test.
💉 Again, no major relief for dryness
✅ Trends toward benefit in systemic features.
👀 Takeaway: RTX may help outside the glands.

4️⃣ BELISS Trial – Enter Belimumab
🔵 Belimumab (anti-BAFF) — aimed at B-cell overdrive.
💡 BELISS (2015):
🟢 Promising systemic activity (↓ ESSDAI)
⚠️ Open-label, small sample
Verdict? Hopeful, but not ready for prime time.
🔵 Belimumab (anti-BAFF) — aimed at B-cell overdrive.
💡 BELISS (2015):
🟢 Promising systemic activity (↓ ESSDAI)
⚠️ Open-label, small sample
Verdict? Hopeful, but not ready for prime time.

5️⃣ NECESSITY Project – Fixing the Real Problem
🤯 Why do trials keep ‘failing’?
💡 Because endpoints are fuzzy!
🎯 NECESSITY is building a validated composite outcome for pSS trials.
Future trials may finally make sense.
🤯 Why do trials keep ‘failing’?
💡 Because endpoints are fuzzy!
🎯 NECESSITY is building a validated composite outcome for pSS trials.
Future trials may finally make sense.
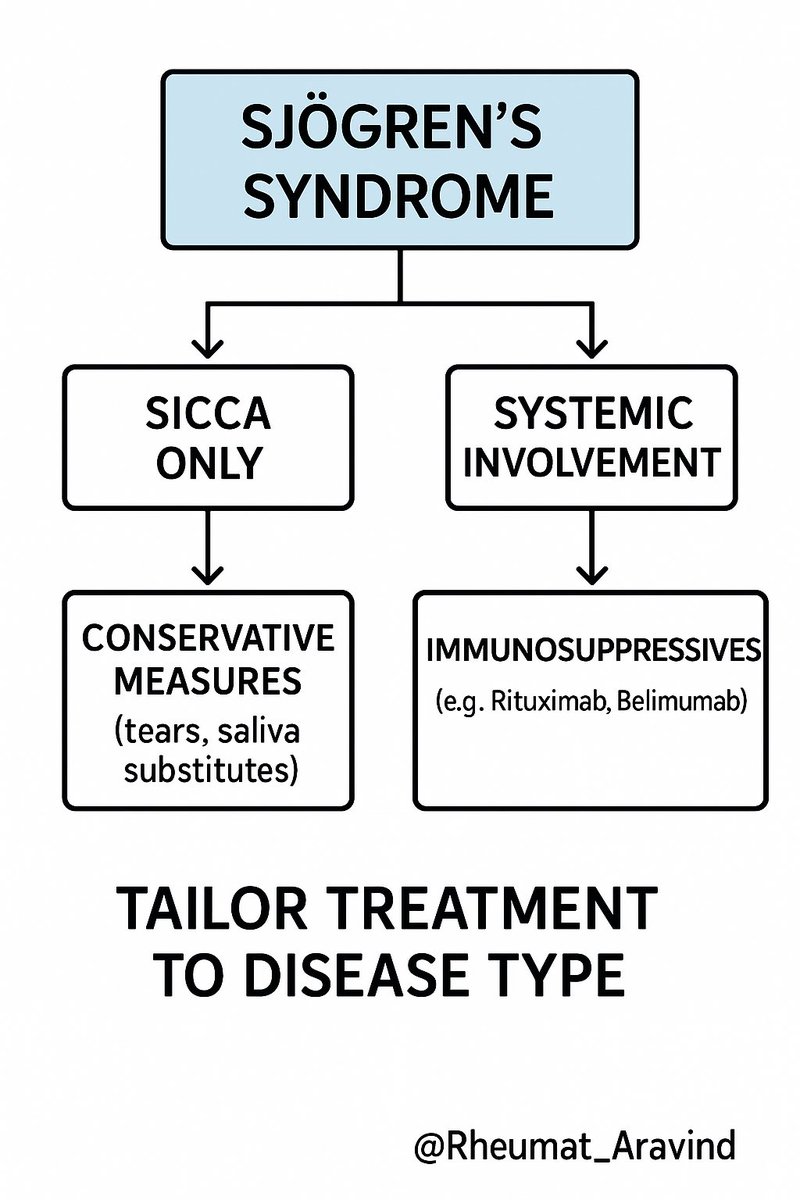
🔚 Final Tweet – Key Takeaways:
📌 HCQ: ↓ enthusiasm
📌 RTX: works for systemic, not sicca
📌 Belimumab: promising, not proven
📌 NECESSITY: might change everything
💬 Until then, treat based on phenotype — not just antibodies.
#Sjögrens #RheumEd
📌 HCQ: ↓ enthusiasm
📌 RTX: works for systemic, not sicca
📌 Belimumab: promising, not proven
📌 NECESSITY: might change everything
💬 Until then, treat based on phenotype — not just antibodies.
#Sjögrens #RheumEd
• • •
Missing some Tweet in this thread? You can try to
force a refresh