Senior Resident in Rheumatology | Madras Medical College, Chennai | 🛑 Tweets ≠ Medical Advice | https://t.co/jtJ1251so2
7 subscribers
How to get URL link on X (Twitter) App

 Tweet 2 – First Rule
Tweet 2 – First Rule
 Tweet 2 - The Diet Myth
Tweet 2 - The Diet Myth

 First, understand the pre-test probability.
First, understand the pre-test probability.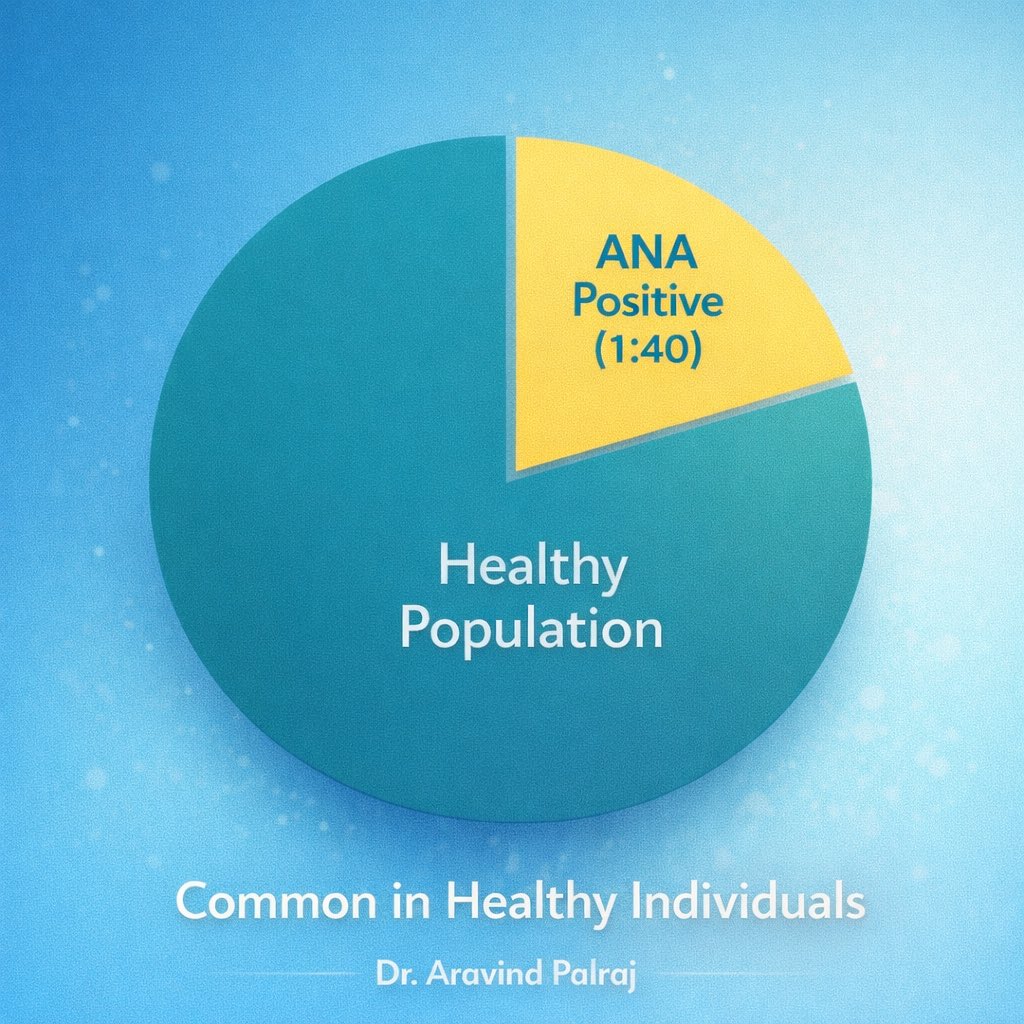
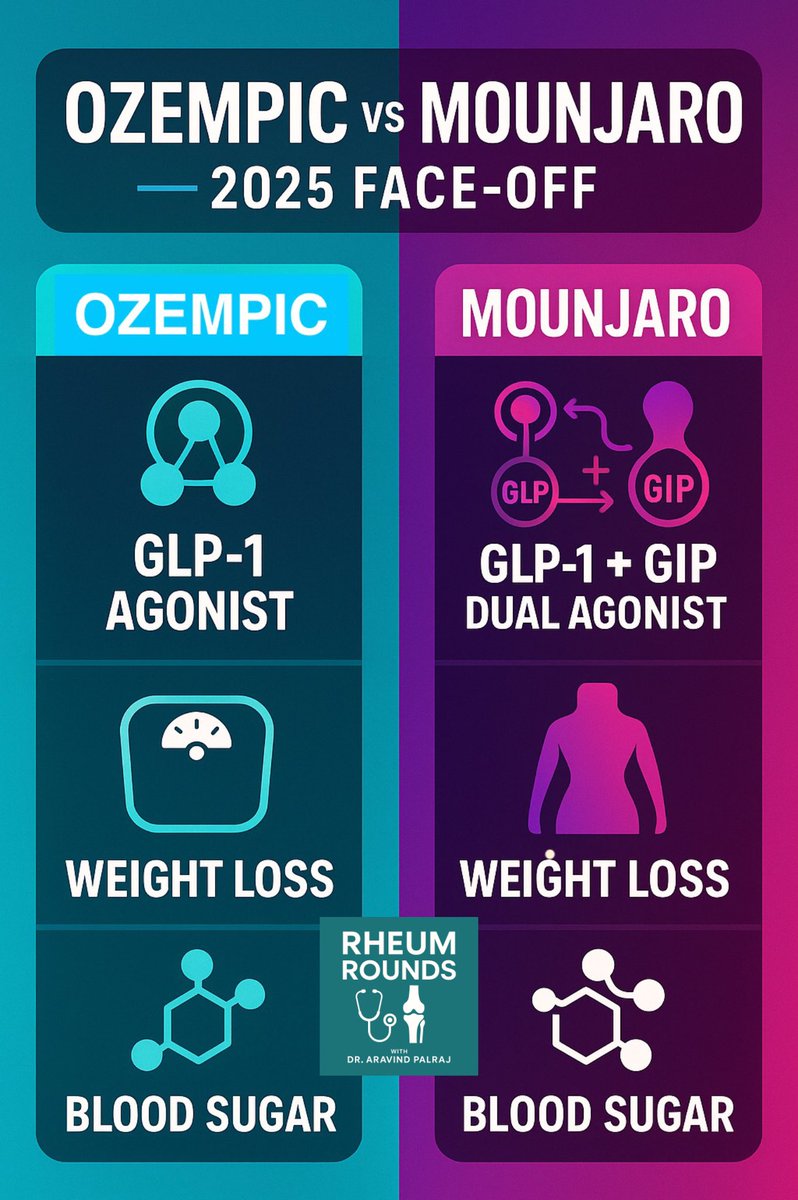
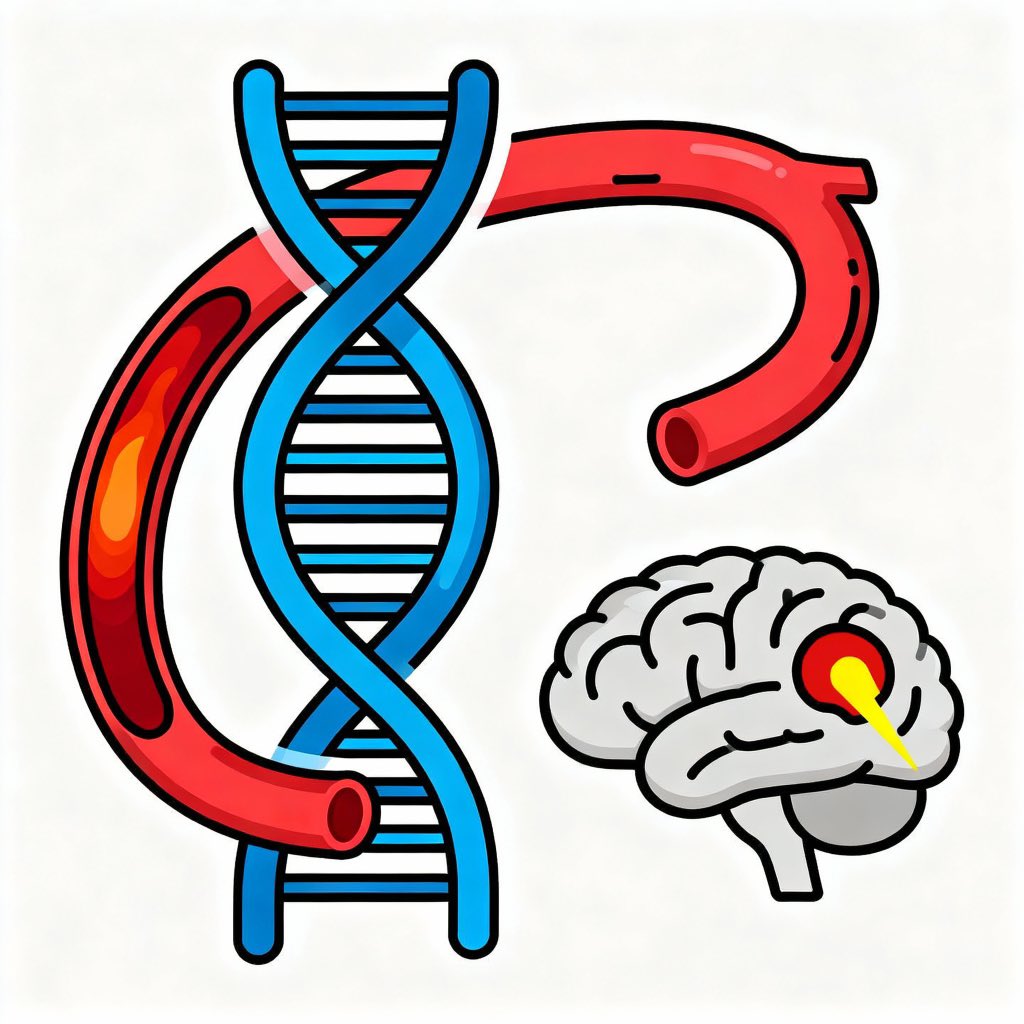
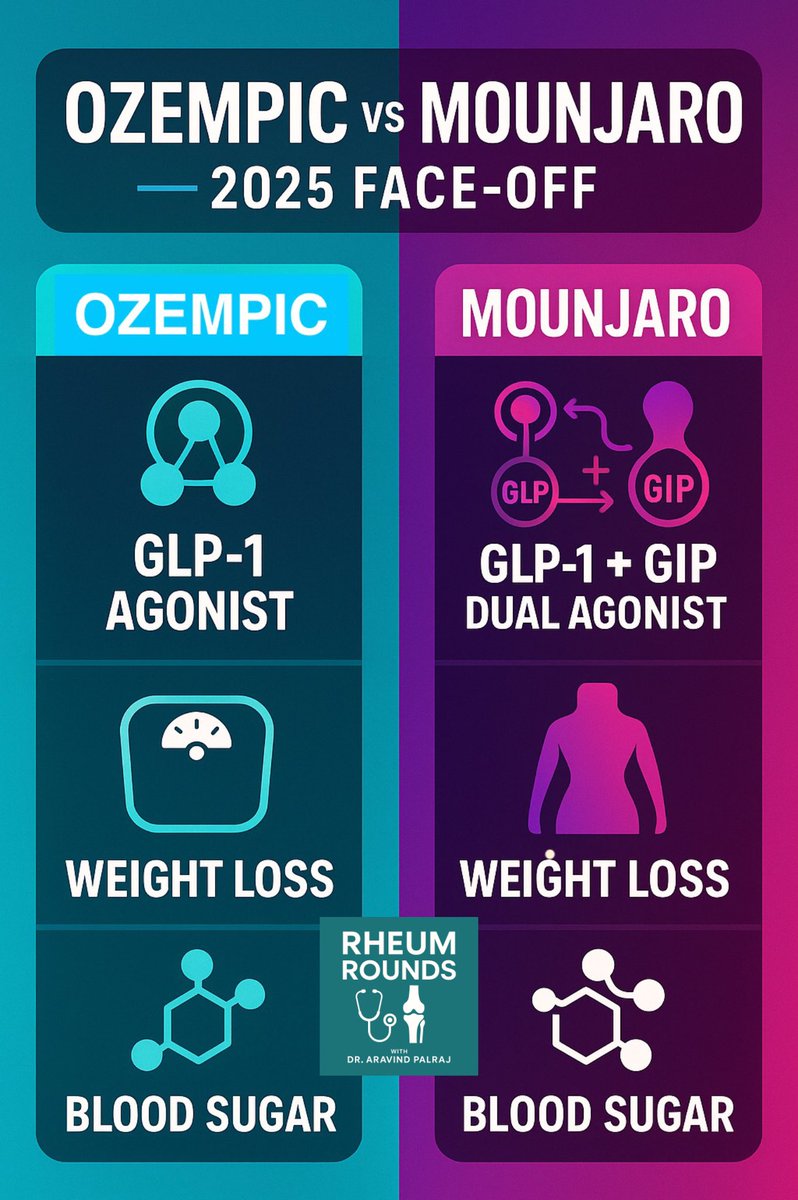 1️⃣ Mechanism
1️⃣ Mechanism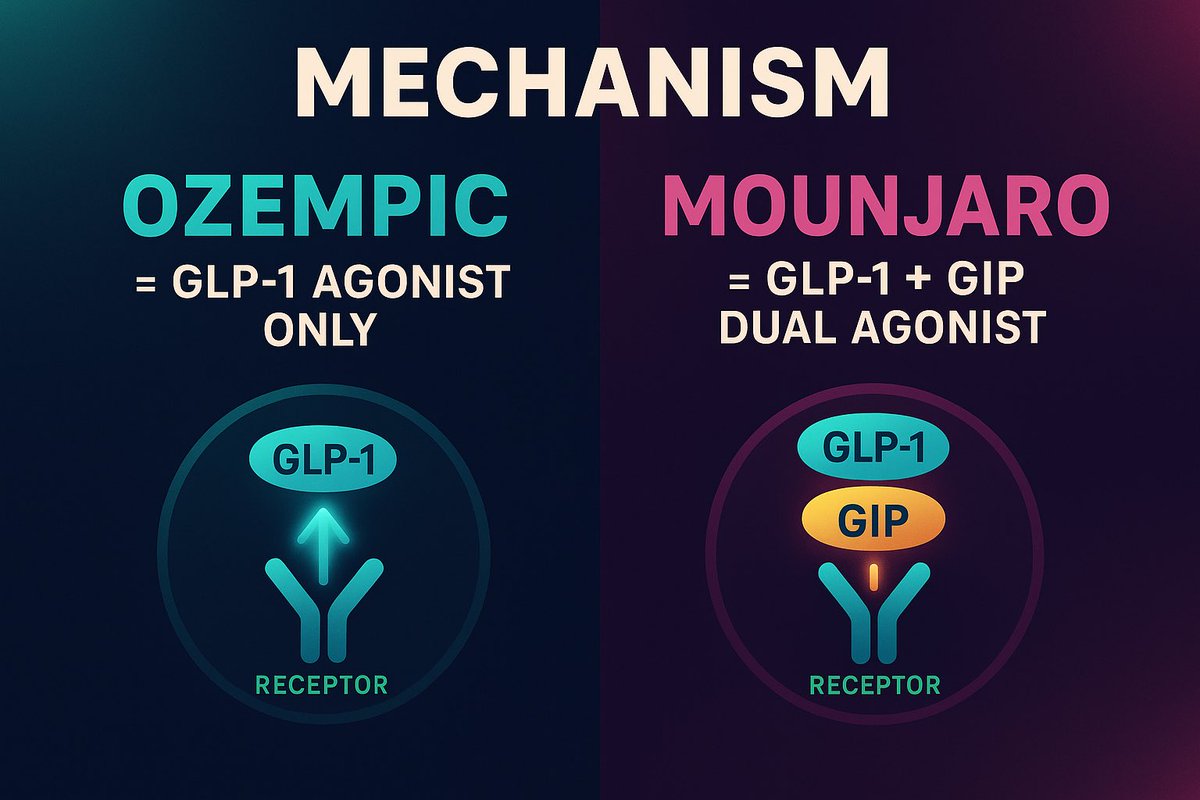

 1️⃣ “ANA is negative, so it’s not lupus.”
1️⃣ “ANA is negative, so it’s not lupus.”
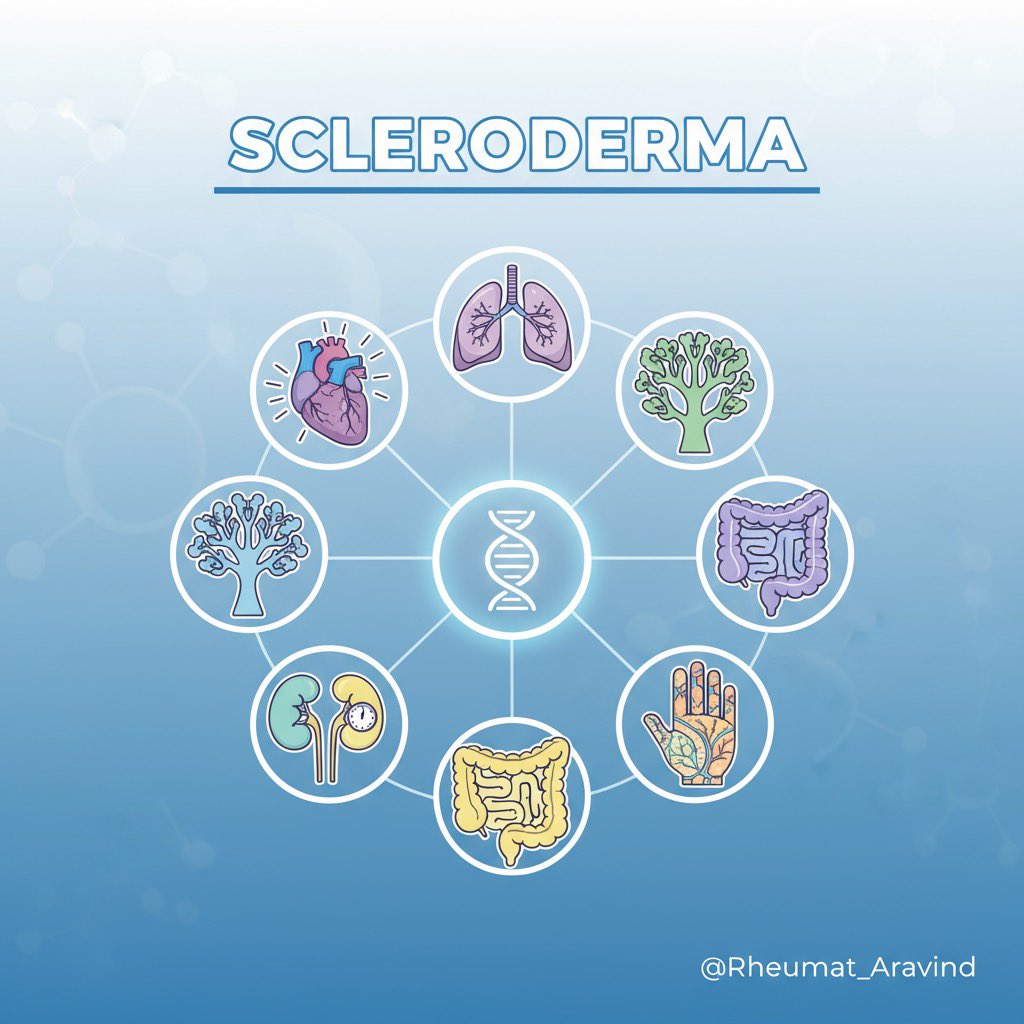
 General and Systemic Signs
General and Systemic Signs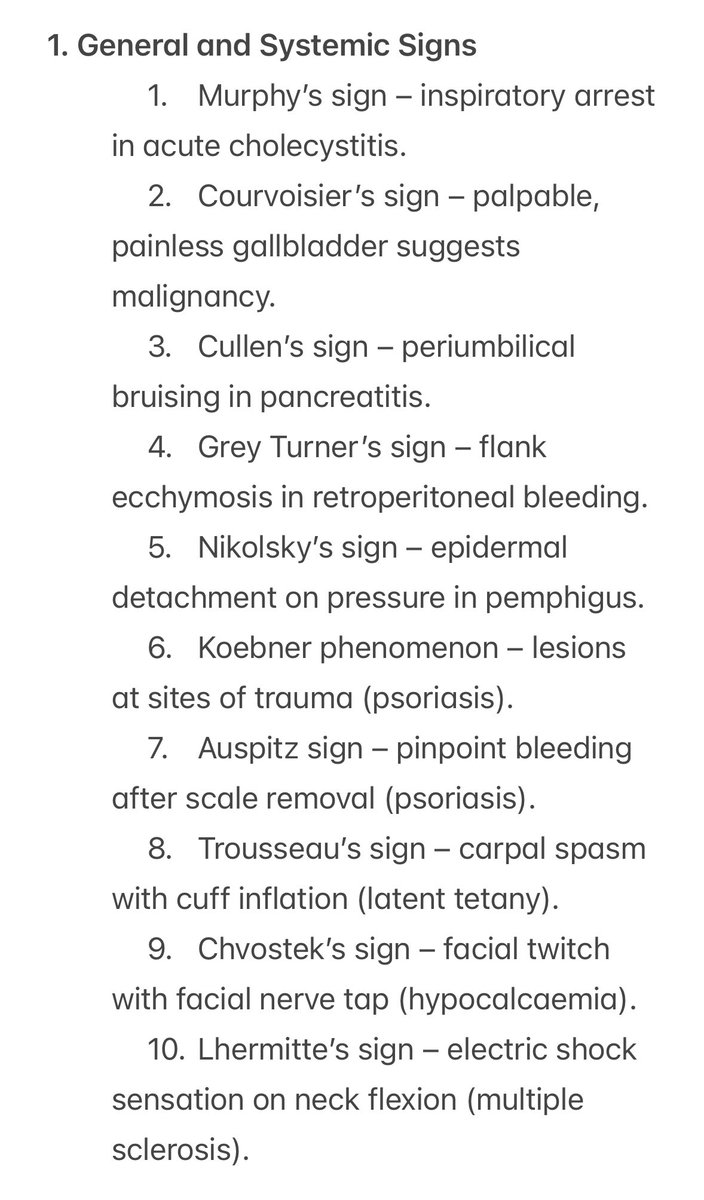
 💬 Tweet 1 – General Principles
💬 Tweet 1 – General Principles
 The Art of Beginning
The Art of Beginning
 General Principles
General Principles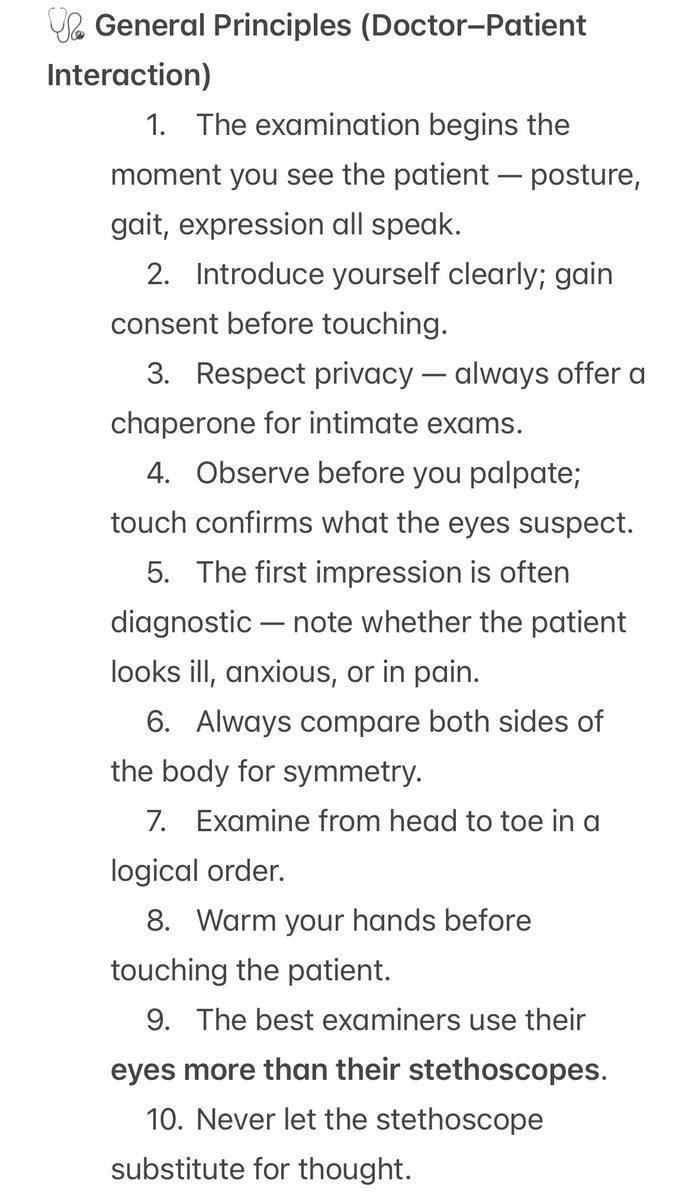
 2/
2/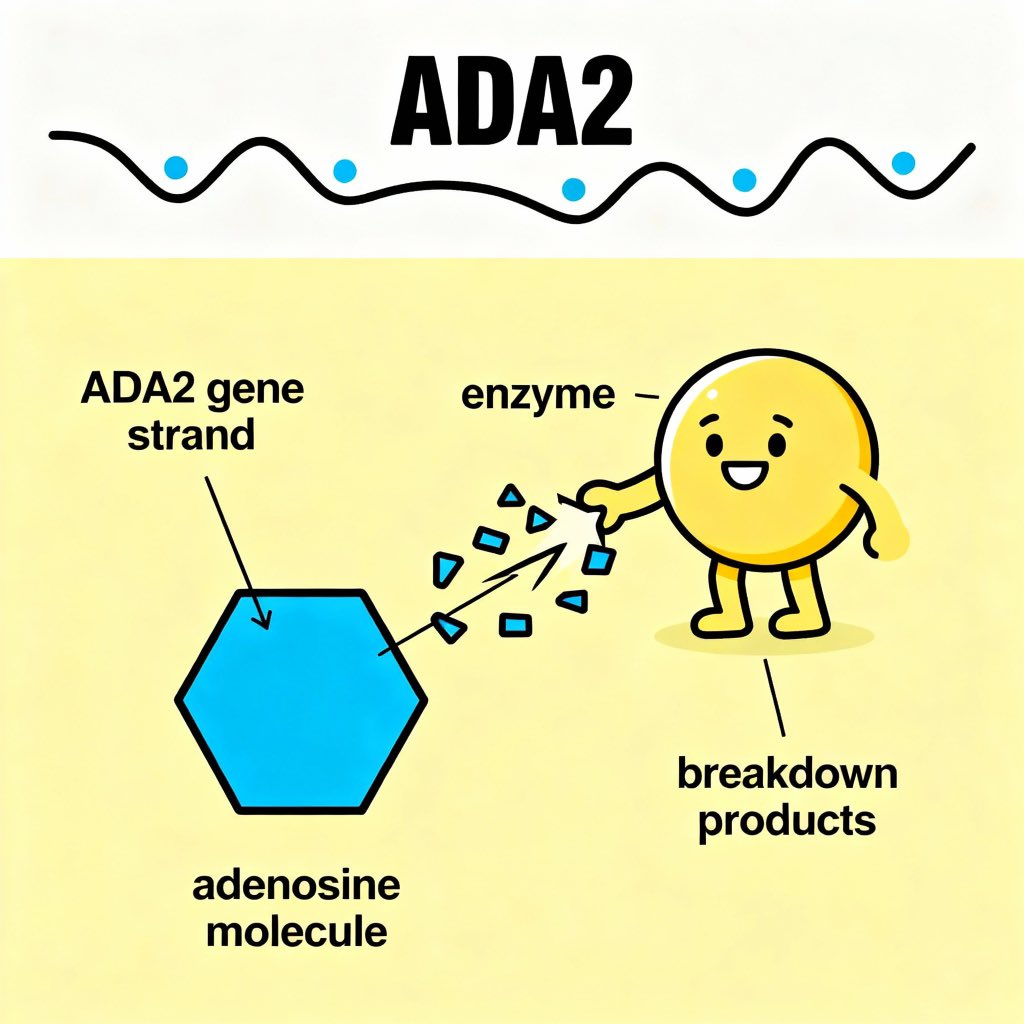
 2/
2/
 Tweet 2:
Tweet 2: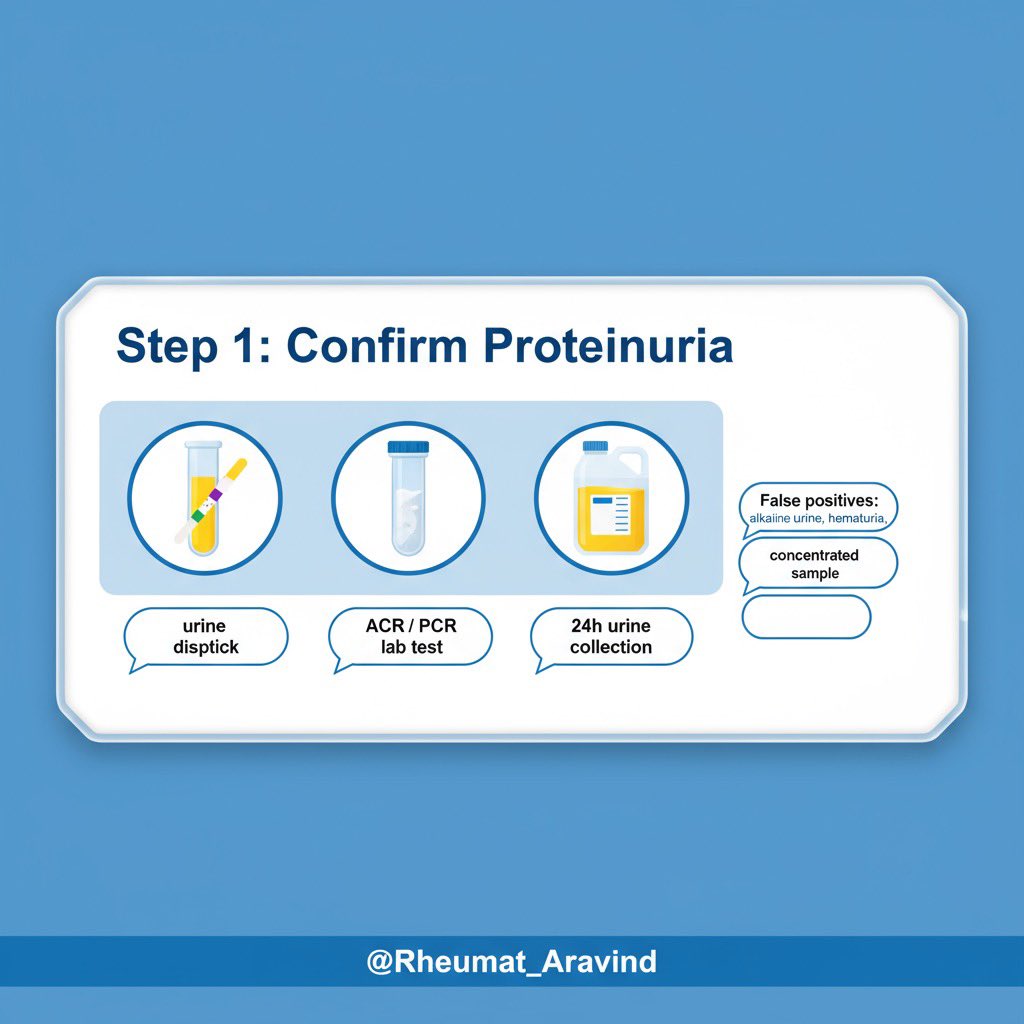
 Tweet 2:
Tweet 2:
 Tweet 2:
Tweet 2:
 Tweet 2 (Pearl 1 – MAS in sJIA):
Tweet 2 (Pearl 1 – MAS in sJIA):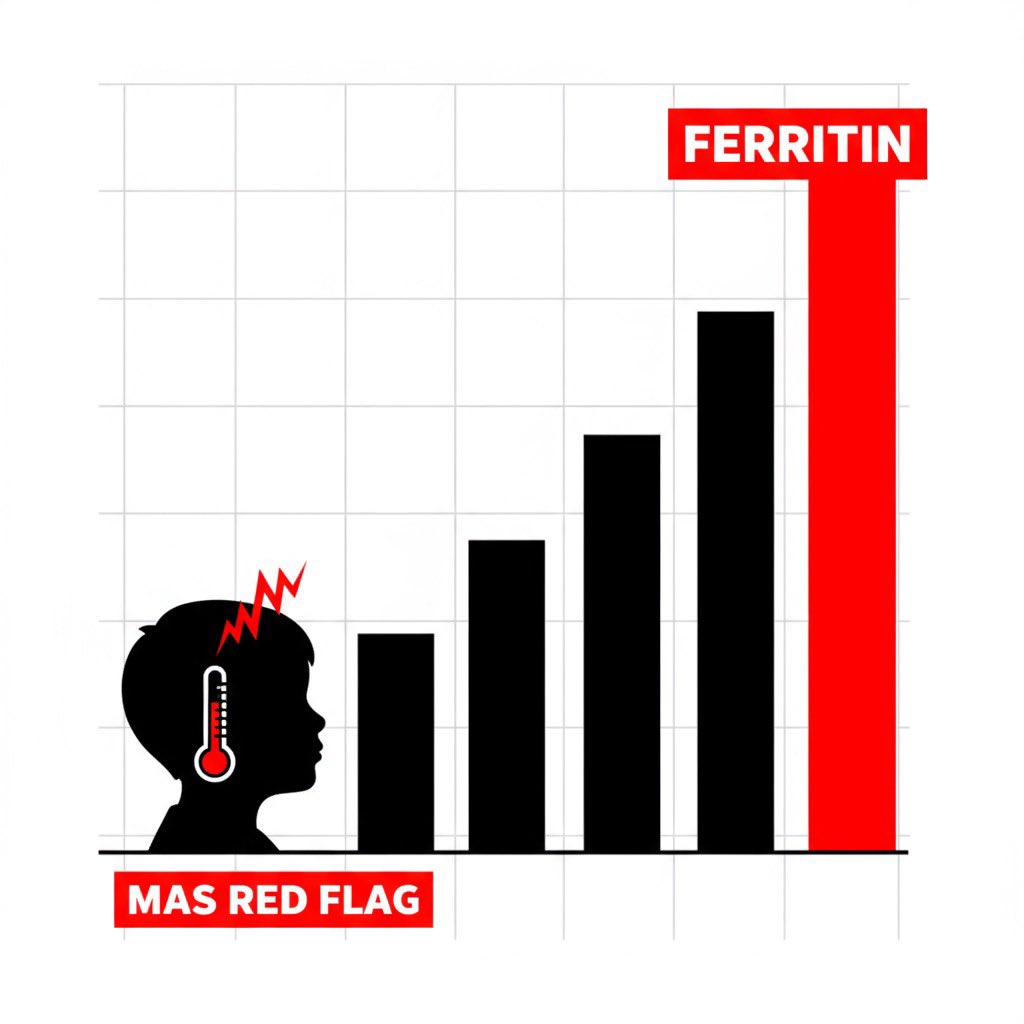
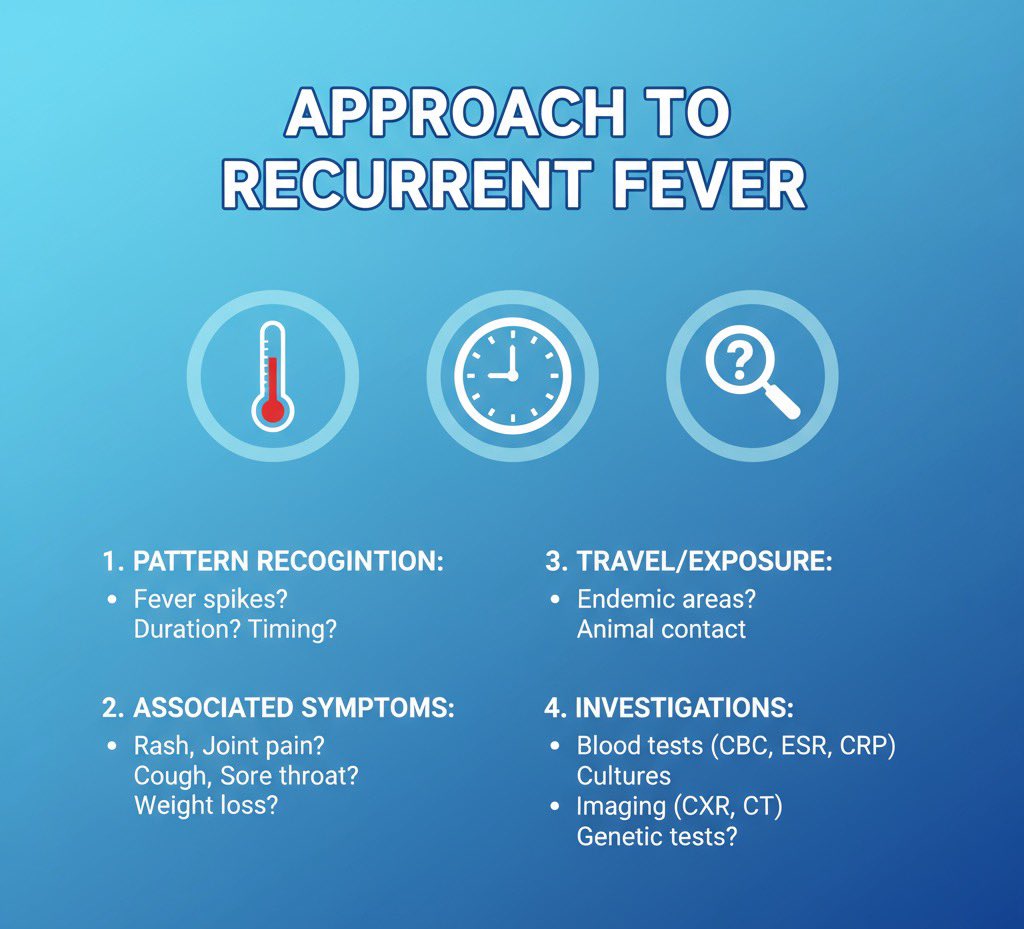
 1. Definition 📌
1. Definition 📌
 2. Categories of FUO 📂
2. Categories of FUO 📂
 2/
2/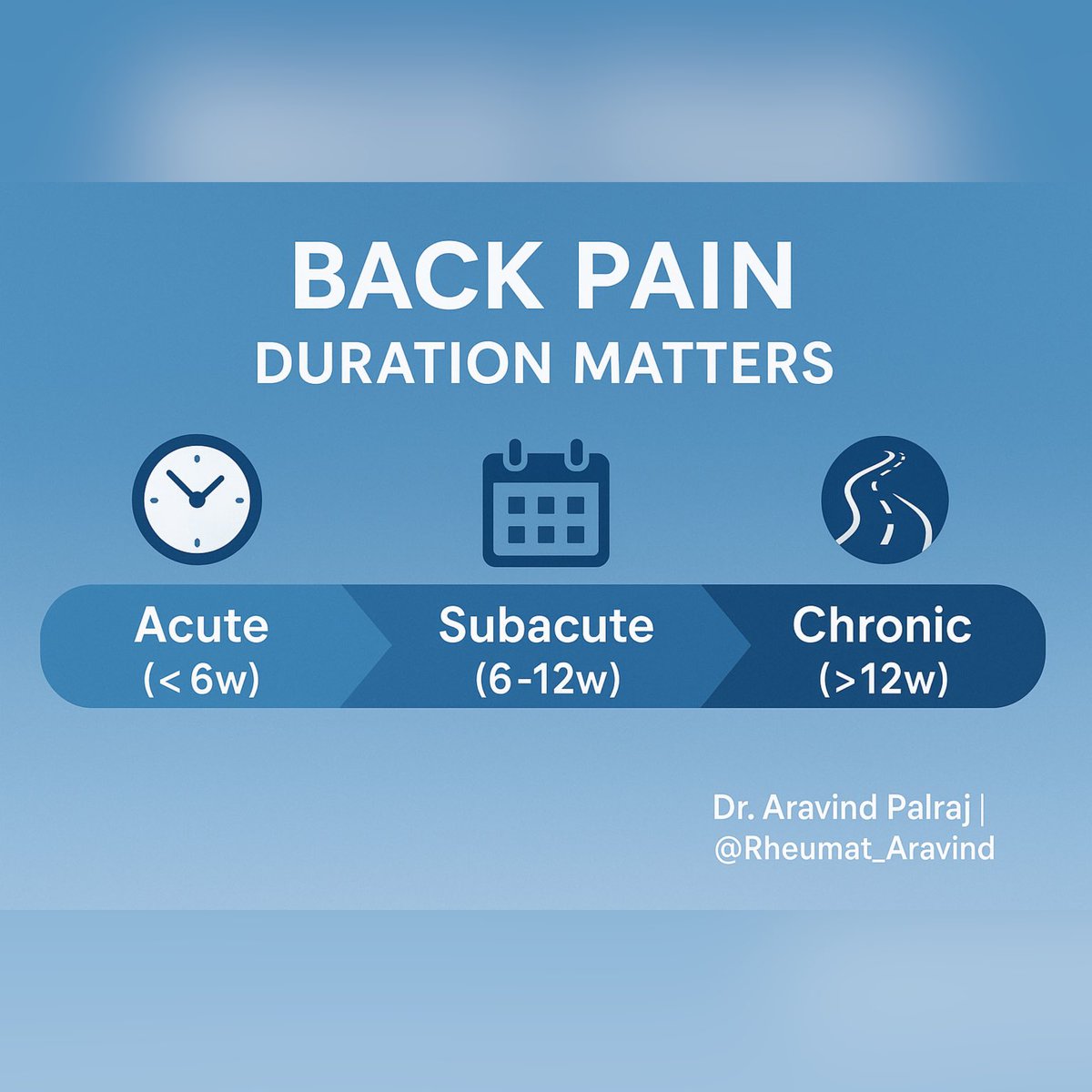
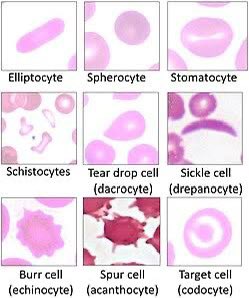
 1. Normal Smear
1. Normal Smear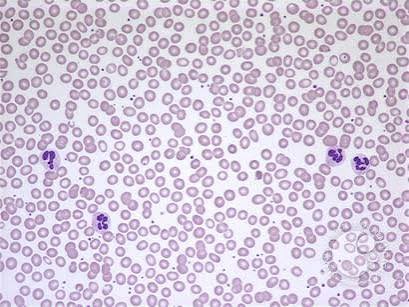
 2️⃣ Enthesitis
2️⃣ Enthesitis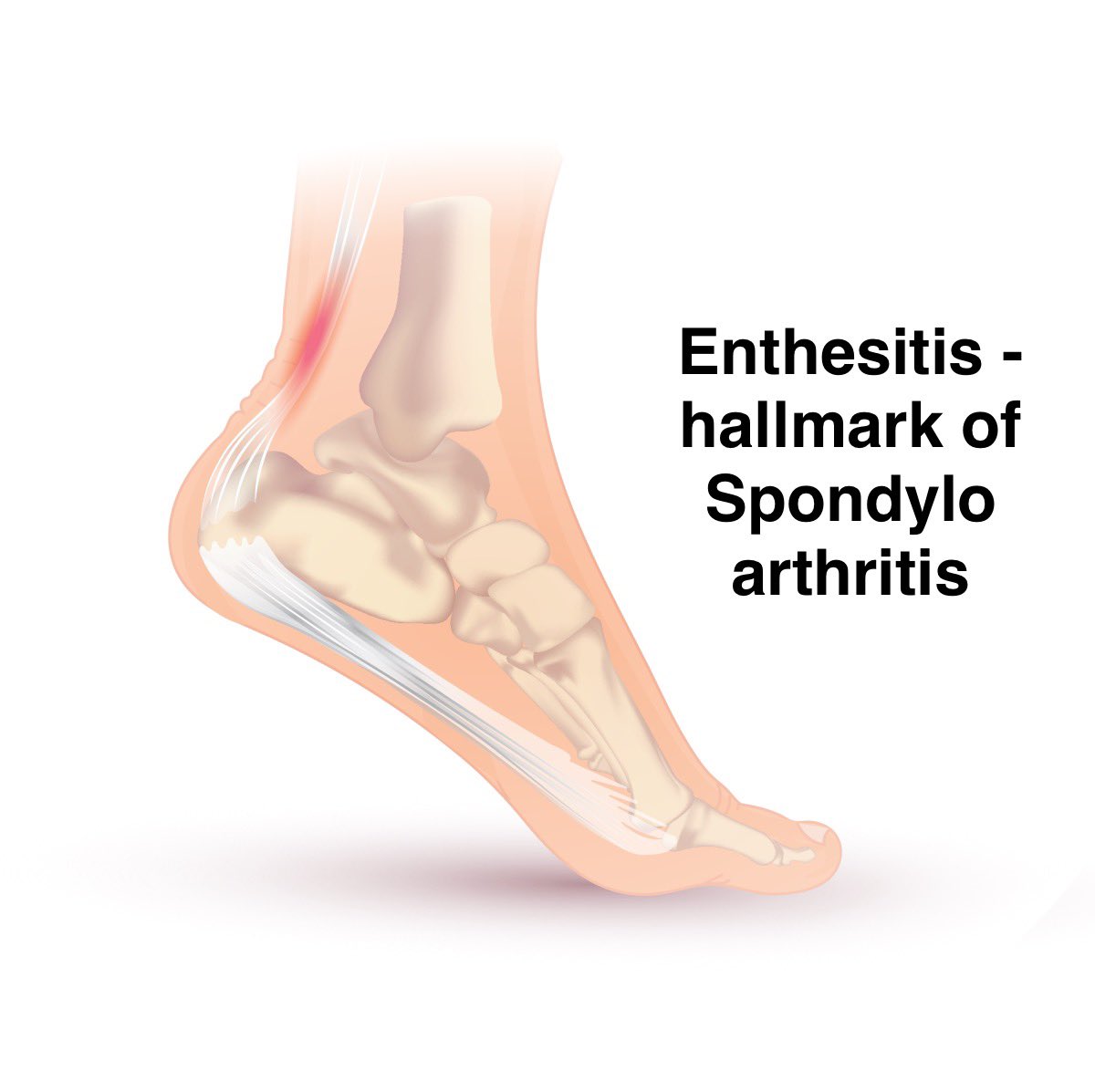
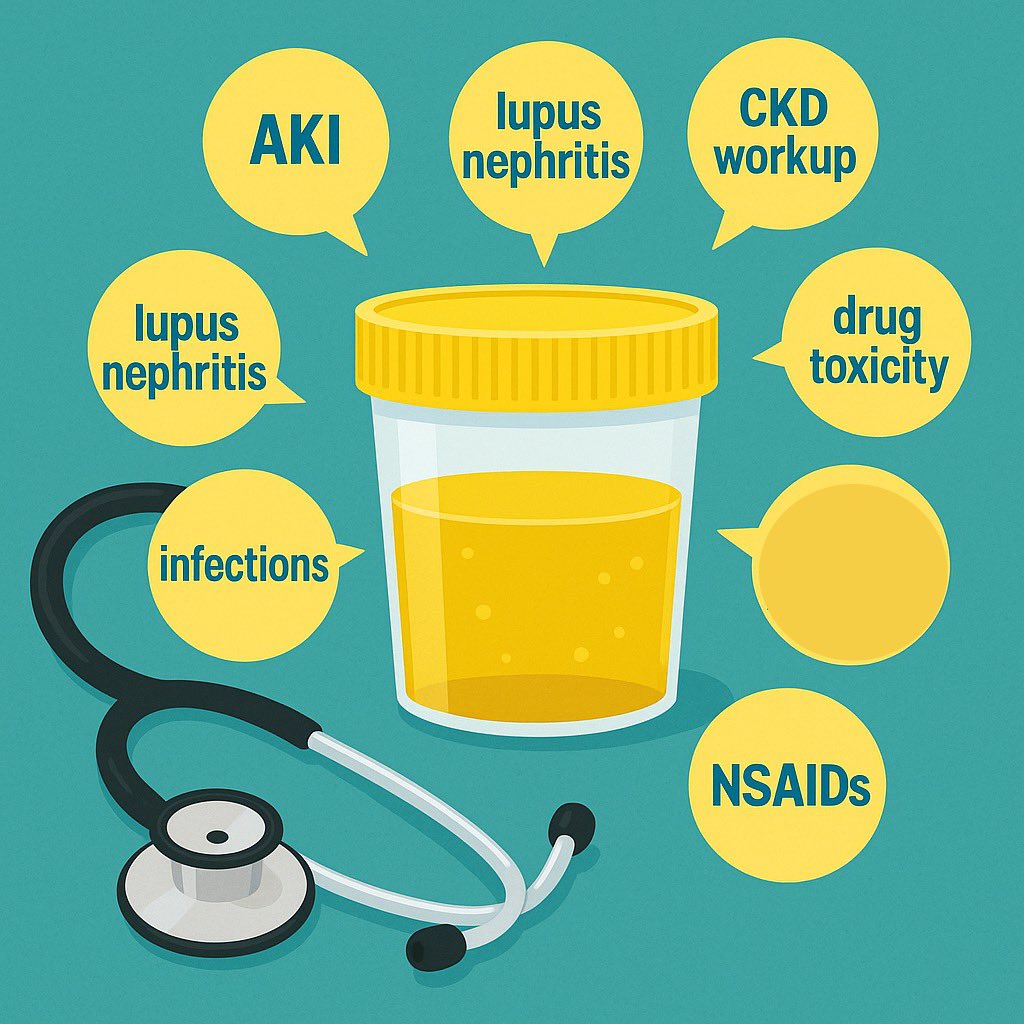
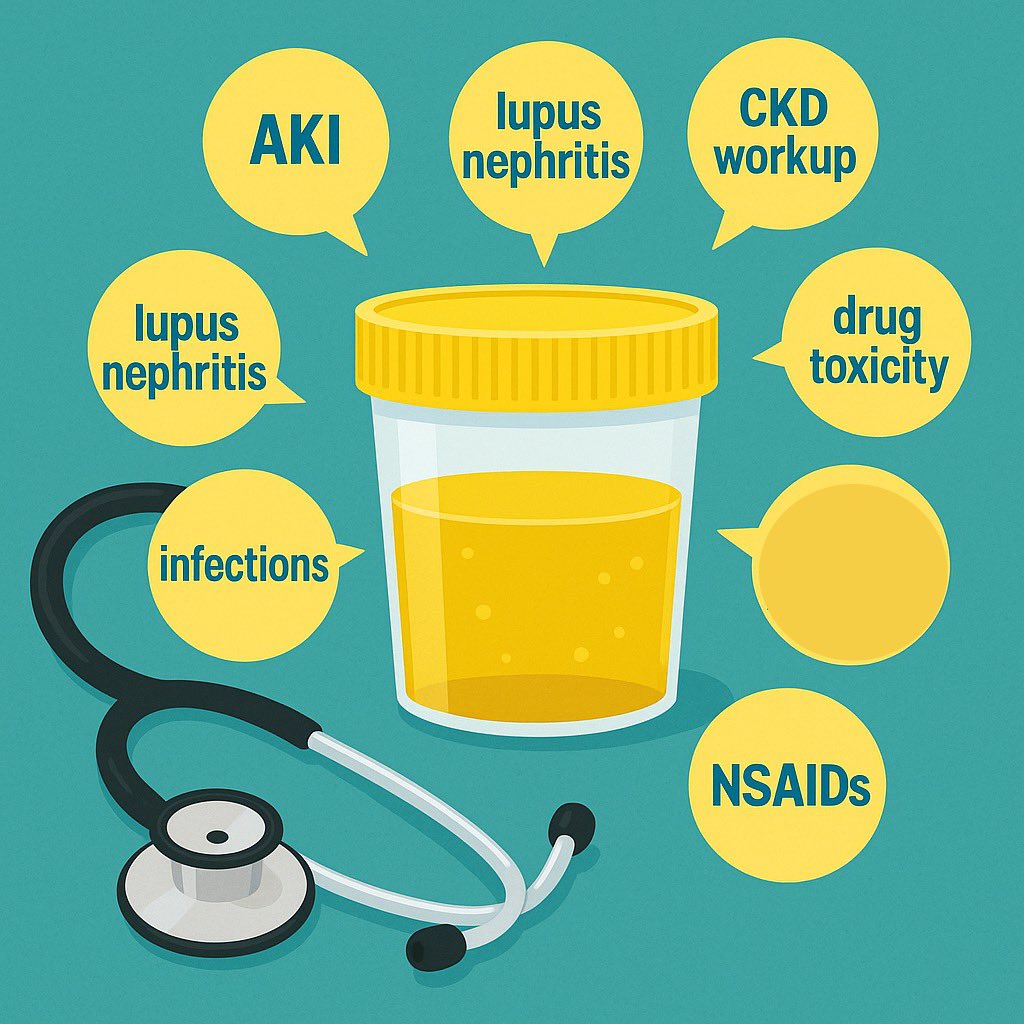 2️⃣ Components of urinalysis
2️⃣ Components of urinalysis