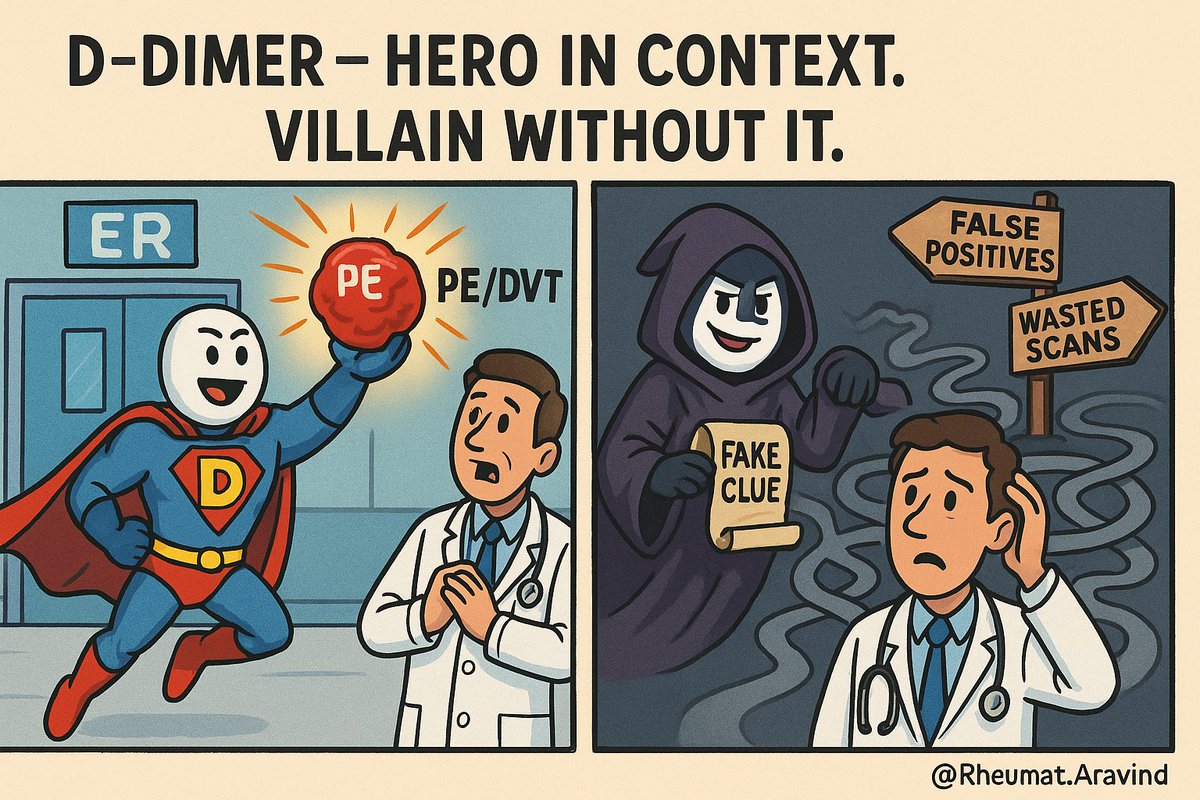
🧵D-Dimer – Diagnostic Hero or Misleading Villain?
We’ve all ordered D-Dimer.
But do we really understand what it’s telling us?
Let’s break down when D-Dimer helps—and when it just adds confusion👇
@IhabFathiSulima @DrAkhilX @drkeithsiau @CelestinoGutirr @Janetbirdope @nirmalregency @Lupusreference #MedTwitter #NEETPG
We’ve all ordered D-Dimer.
But do we really understand what it’s telling us?
Let’s break down when D-Dimer helps—and when it just adds confusion👇
@IhabFathiSulima @DrAkhilX @drkeithsiau @CelestinoGutirr @Janetbirdope @nirmalregency @Lupusreference #MedTwitter #NEETPG
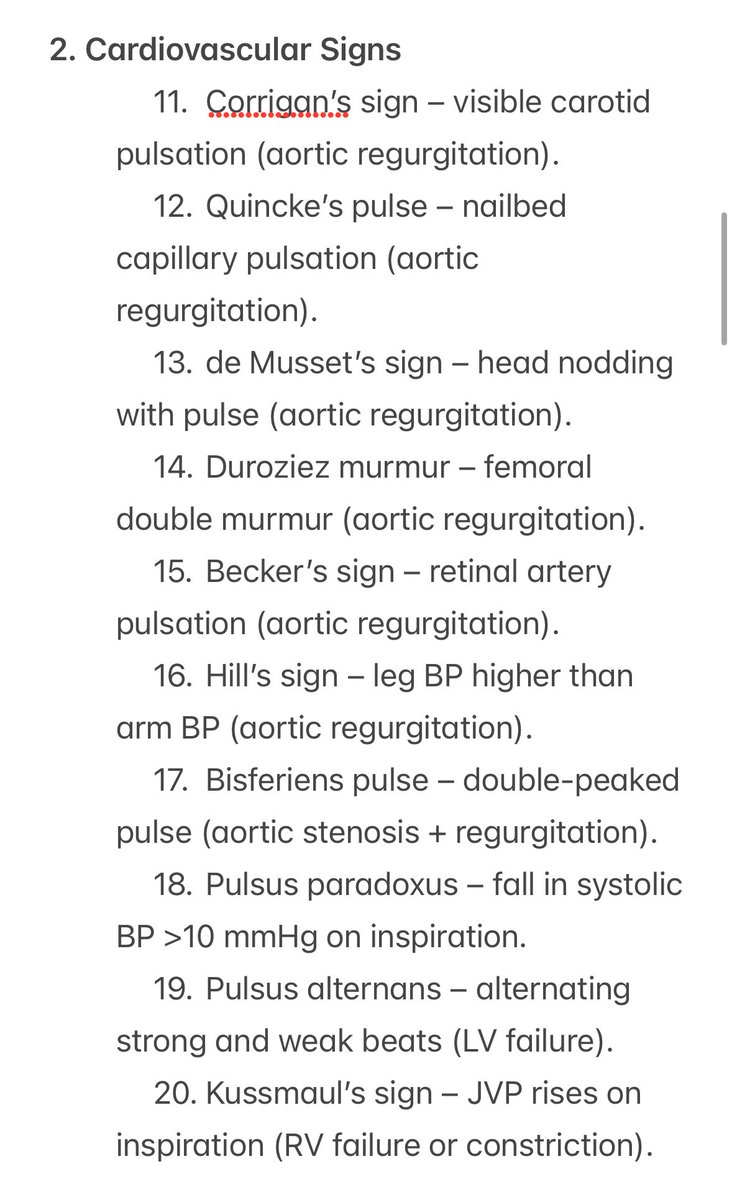
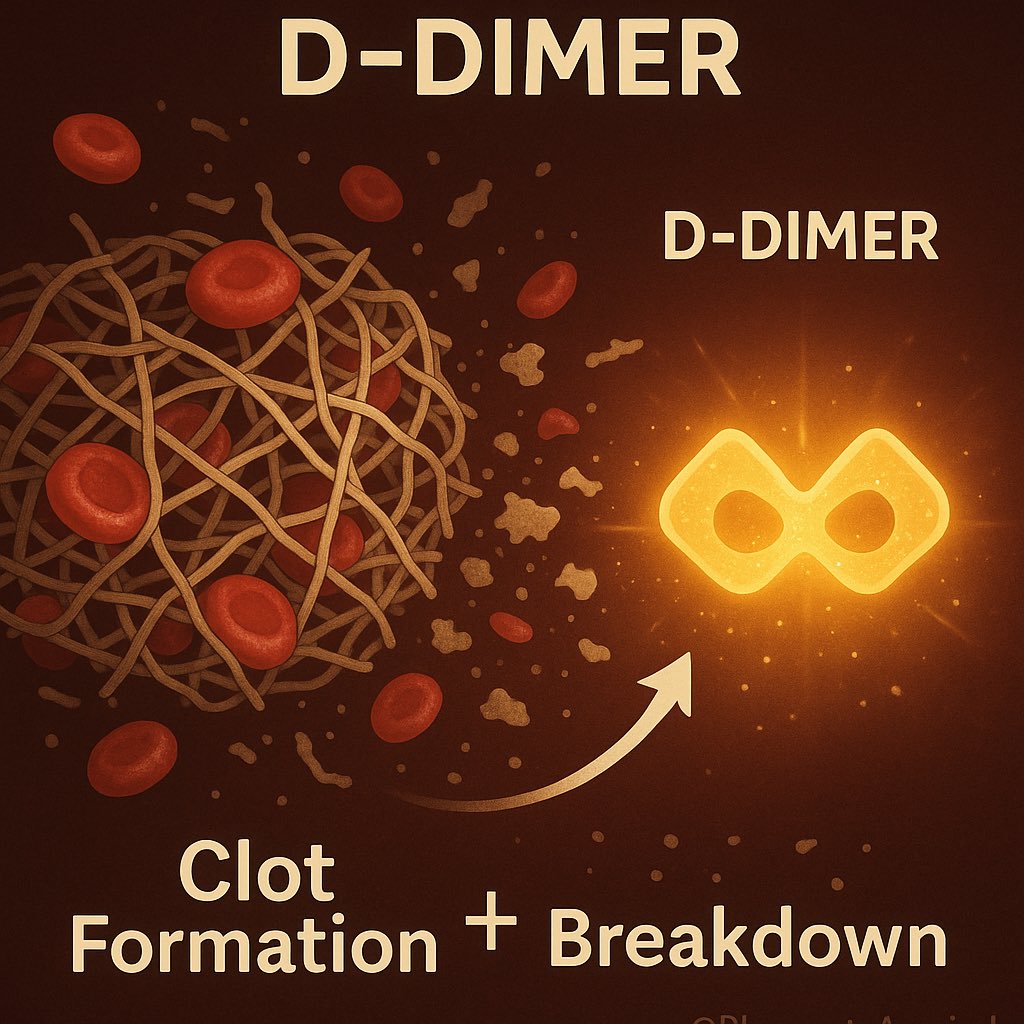
1. What is D-Dimer, really?
🧬 It’s a fibrin degradation product.
If you see it, it means the body formed and broke down a clot.
But: That doesn’t always mean pathology.
🧬 It’s a fibrin degradation product.
If you see it, it means the body formed and broke down a clot.
But: That doesn’t always mean pathology.
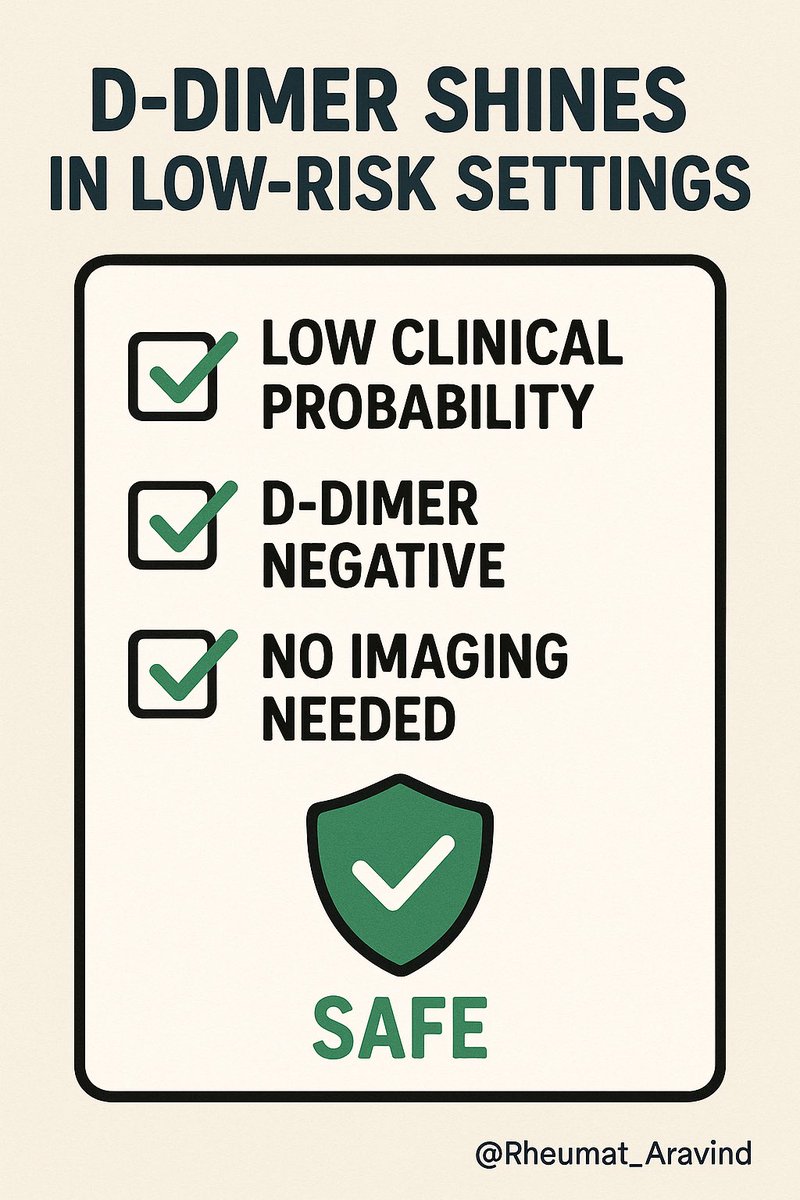
2. When is it actually useful?
✅ Low to moderate suspicion of DVT/PE
🧠 It’s a rule-out tool
Normal D-Dimer? Great.
Abnormal? Don’t panic yet.
✅ Low to moderate suspicion of DVT/PE
🧠 It’s a rule-out tool
Normal D-Dimer? Great.
Abnormal? Don’t panic yet.
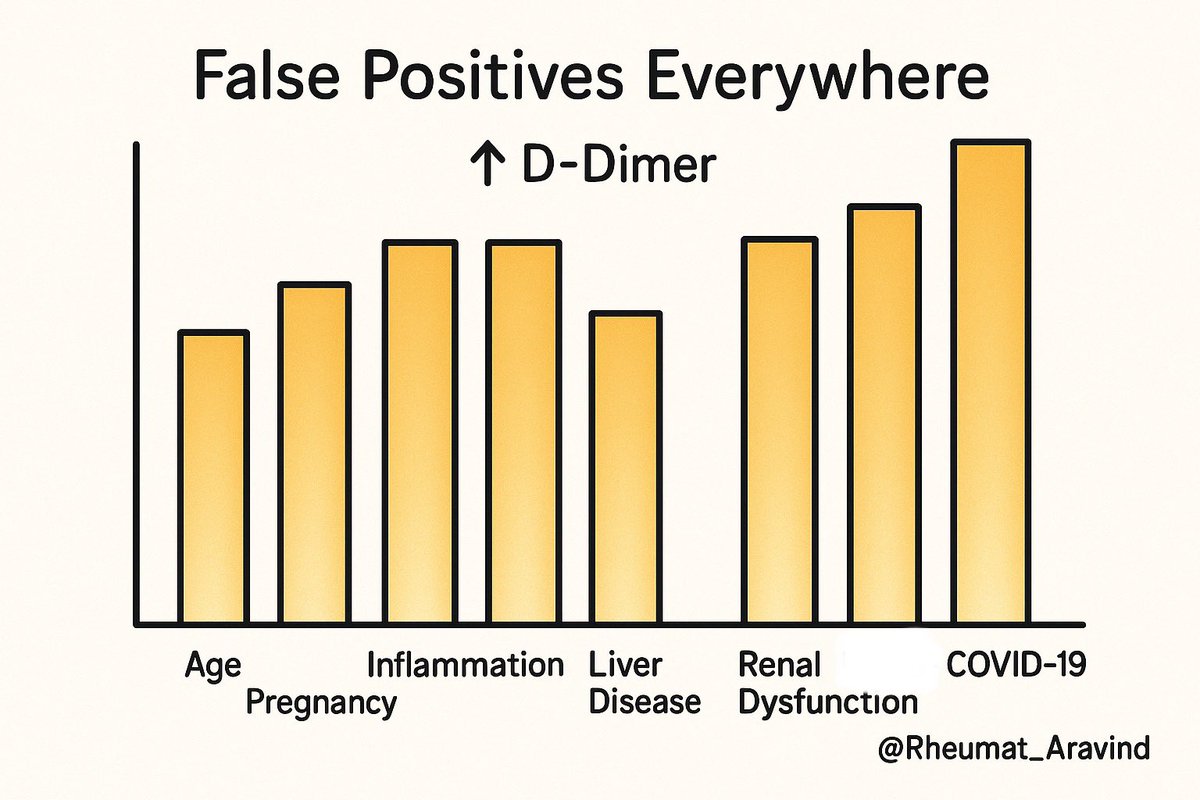
3. D-Dimer can go up for tons of reasons:
– Age > 50
– Surgery, trauma
– Infections, cancer
– Pregnancy
– SLE, vasculitis
– COVID-19
– Hospital admission itself!
– Age > 50
– Surgery, trauma
– Infections, cancer
– Pregnancy
– SLE, vasculitis
– COVID-19
– Hospital admission itself!
4. Rheumatology trap: Flare or clot?
SLE patient with leg pain + raised D-Dimer?
🔍 Check pretest probability
🔄 If low → duplex or imaging
💡 Don’t anchor on D-Dimer alone
SLE patient with leg pain + raised D-Dimer?
🔍 Check pretest probability
🔄 If low → duplex or imaging
💡 Don’t anchor on D-Dimer alone
5. What’s an age-adjusted D-Dimer?
🧓 After age 50, D-Dimer naturally rises.
So we adjust:
Age × 10 ng/mL (FEU) = cutoff
E.g. Age 72 → cutoff is 720
🧓 After age 50, D-Dimer naturally rises.
So we adjust:
Age × 10 ng/mL (FEU) = cutoff
E.g. Age 72 → cutoff is 720

6. How NOT to use D-Dimer:
🚫 High suspicion? Go straight to imaging.
🚫 As a standalone test.
🚫 To monitor clot burden.
🚫 In inflammatory diseases to predict thrombosis without clinical context.
🚫 High suspicion? Go straight to imaging.
🚫 As a standalone test.
🚫 To monitor clot burden.
🚫 In inflammatory diseases to predict thrombosis without clinical context.

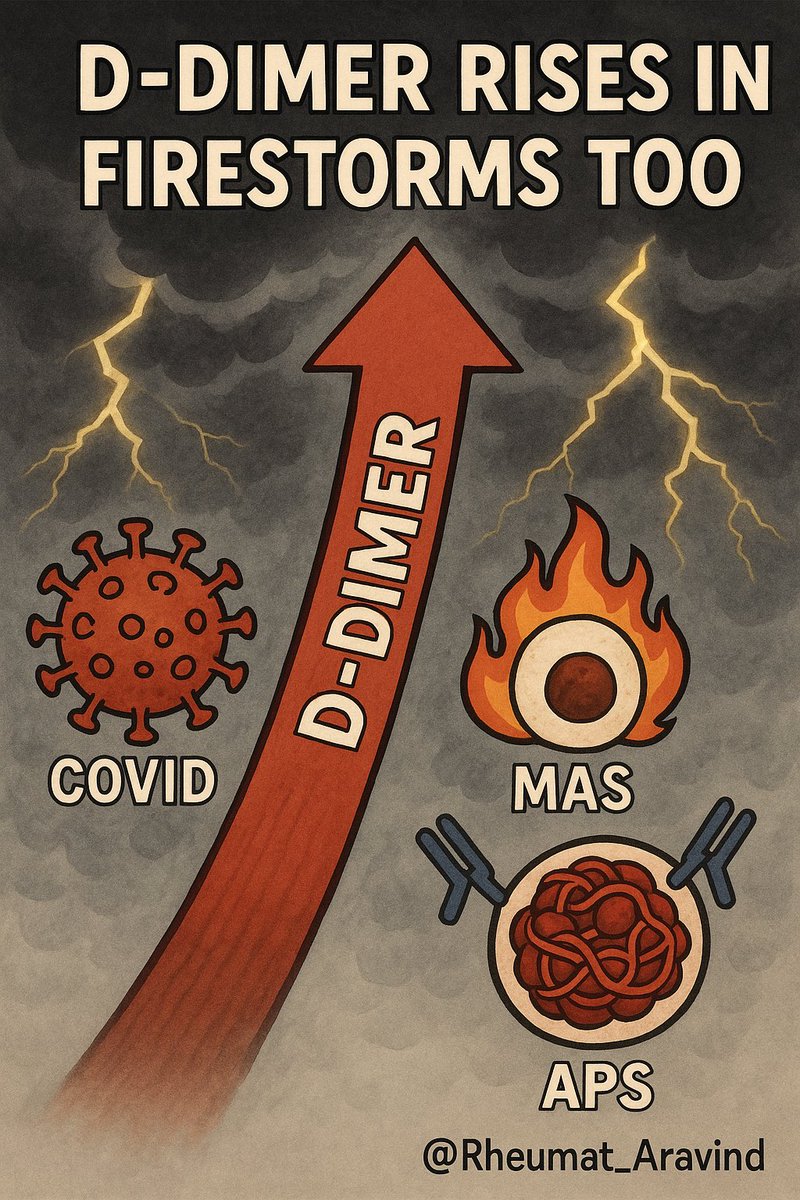
7. D-Dimer in COVID, APS, MAS?
🔴 High D-Dimer = clot risk, cytokine storm, endothelial damage
BUT: Use clinical correlation.
Don’t treat numbers in isolation.
🔴 High D-Dimer = clot risk, cytokine storm, endothelial damage
BUT: Use clinical correlation.
Don’t treat numbers in isolation.
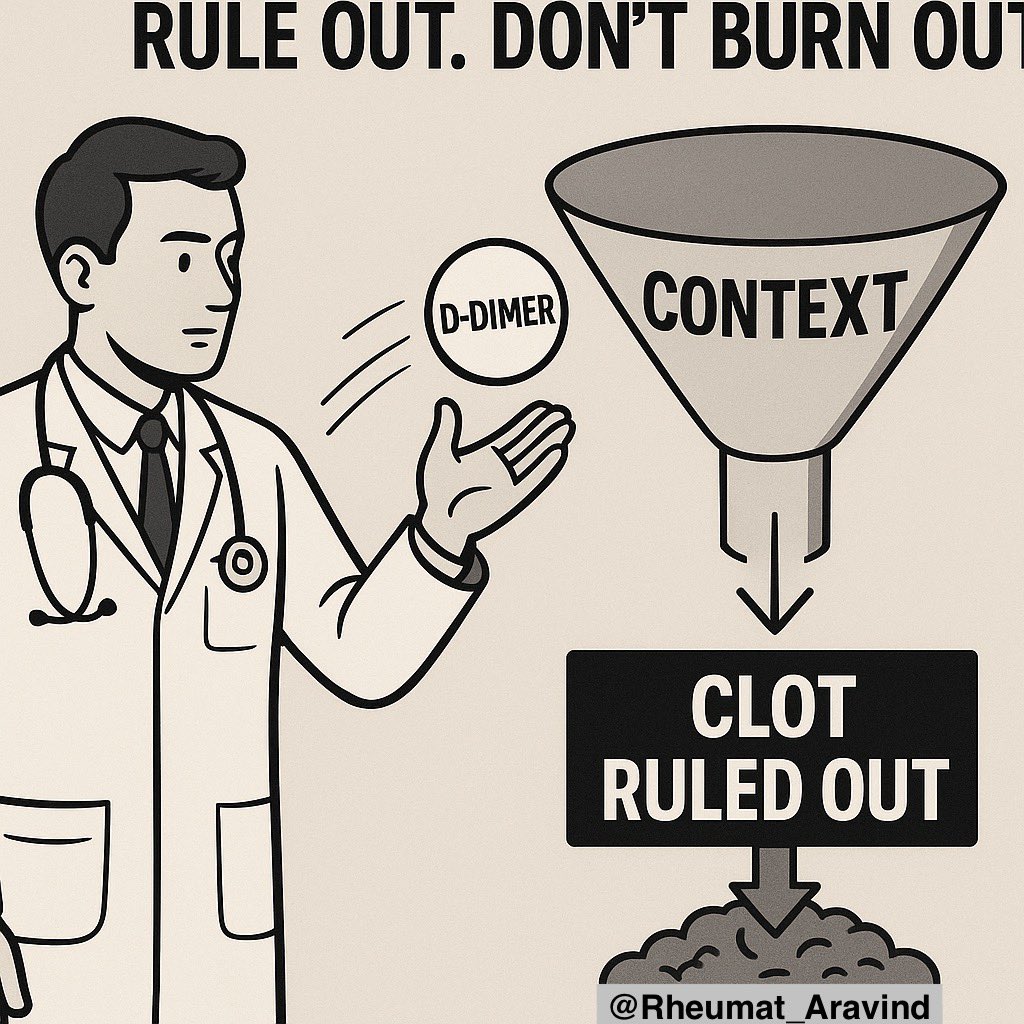
📌 Takeaway
D-Dimer is powerful in the right clinical context.
Don’t let it become a diagnostic distraction.
Use it to rule out, not stress out.
D-Dimer is powerful in the right clinical context.
Don’t let it become a diagnostic distraction.
Use it to rule out, not stress out.
• • •
Missing some Tweet in this thread? You can try to
force a refresh