🧵 Clues Your “Arthritis” Patient Doesn’t Actually Have RA
Not all swollen joints are rheumatoid arthritis.
Some look identical—but aren’t.
Here’s how to spot RA mimics before the label sticks forever 👇
@IhabFathiSulima @DrAkhilX @SarahSchaferMD @Janetbirdope #MedTwitter #Rheumatology
Not all swollen joints are rheumatoid arthritis.
Some look identical—but aren’t.
Here’s how to spot RA mimics before the label sticks forever 👇
@IhabFathiSulima @DrAkhilX @SarahSchaferMD @Janetbirdope #MedTwitter #Rheumatology

2. The wrong joints are involved
RA = MCP, PIP, wrists.
If DIP joints are involved → think OA, psoriatic arthritis.
If only large joints → think reactive, viral, crystal arthritis.
RA = MCP, PIP, wrists.
If DIP joints are involved → think OA, psoriatic arthritis.
If only large joints → think reactive, viral, crystal arthritis.

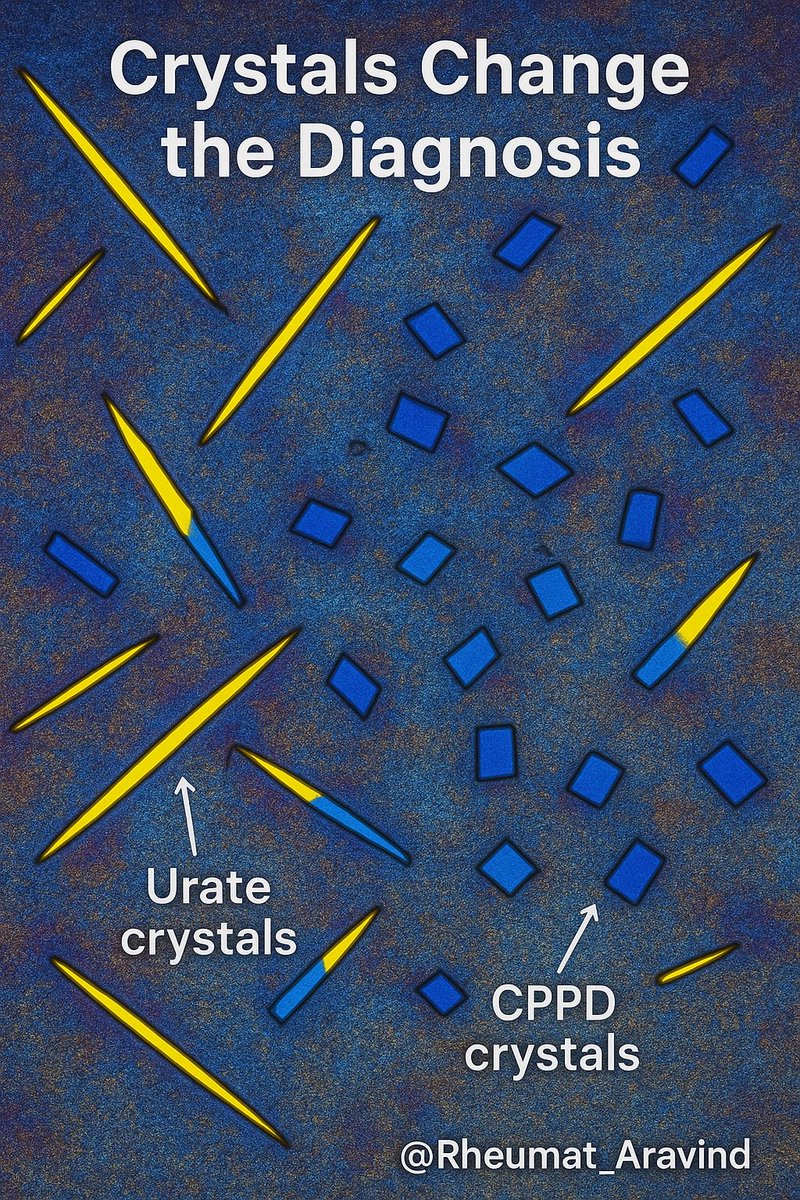
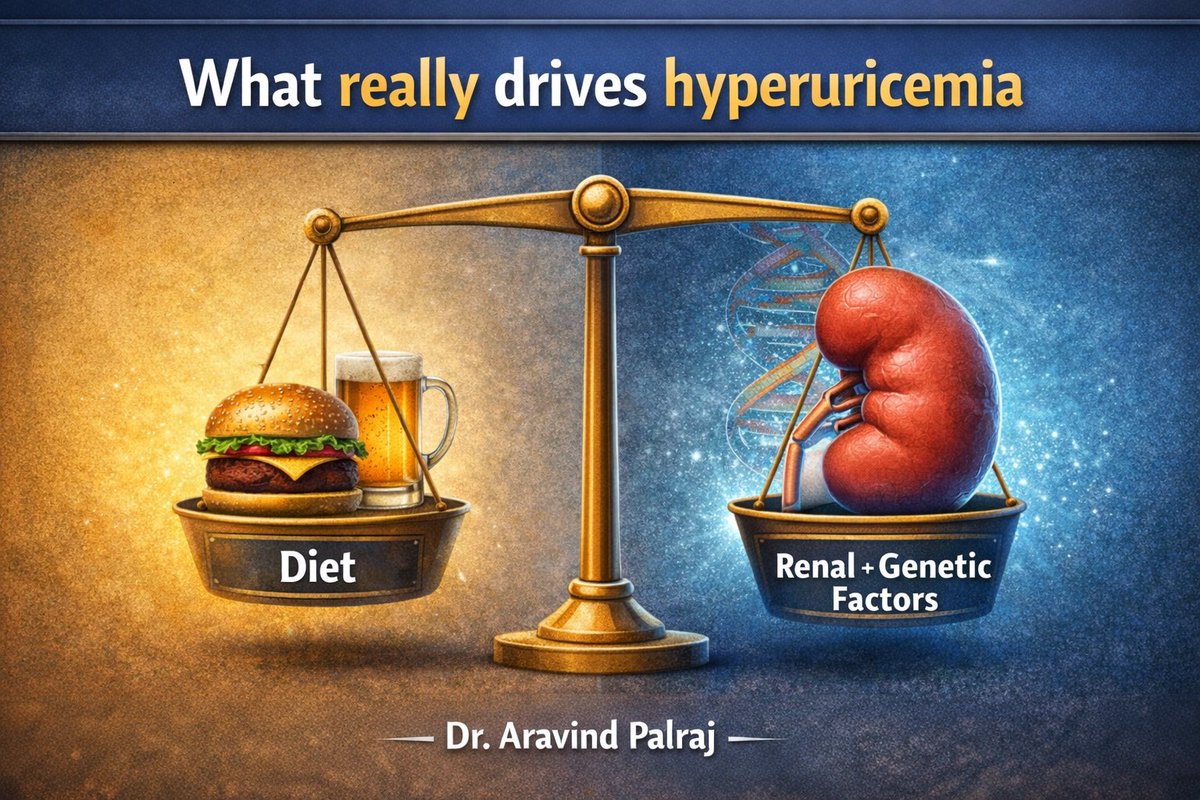
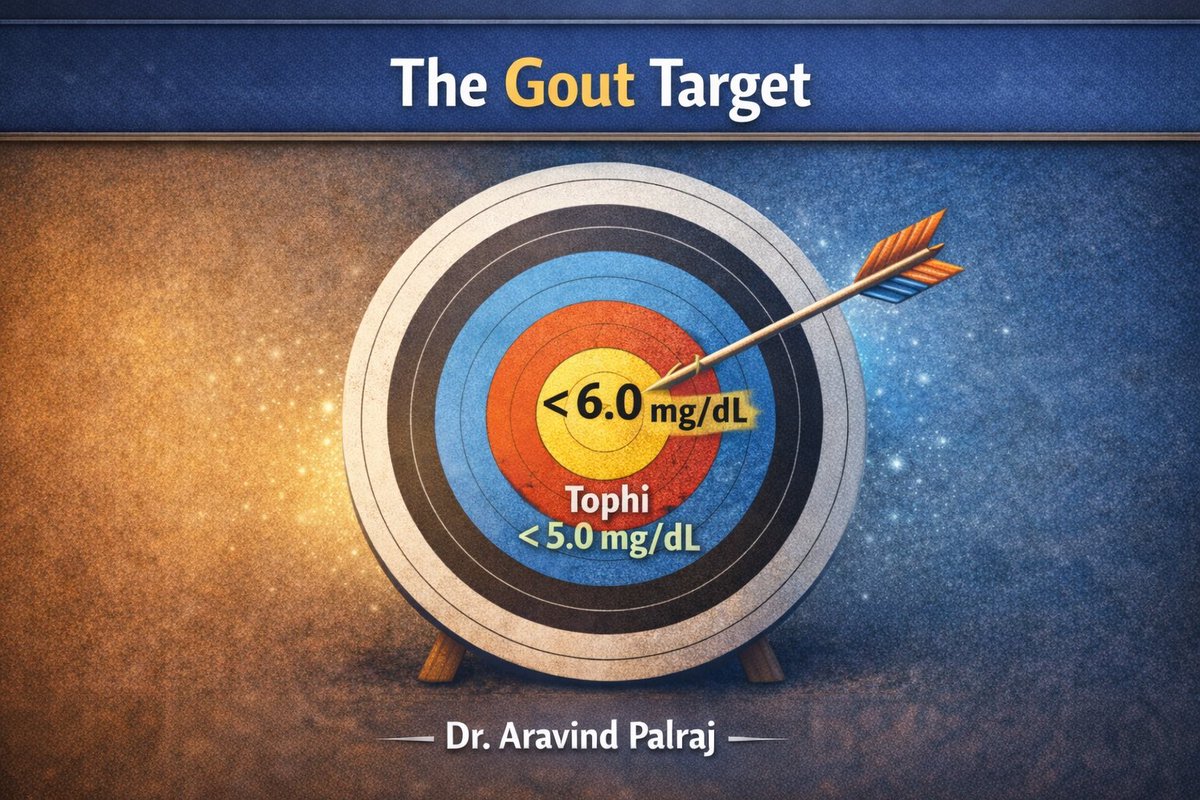
3. Too acute for RA
RA builds over weeks.
If swelling peaks in 24–48 hrs → think gout, pseudogout, septic arthritis, viral arthritis.
RA builds over weeks.
If swelling peaks in 24–48 hrs → think gout, pseudogout, septic arthritis, viral arthritis.
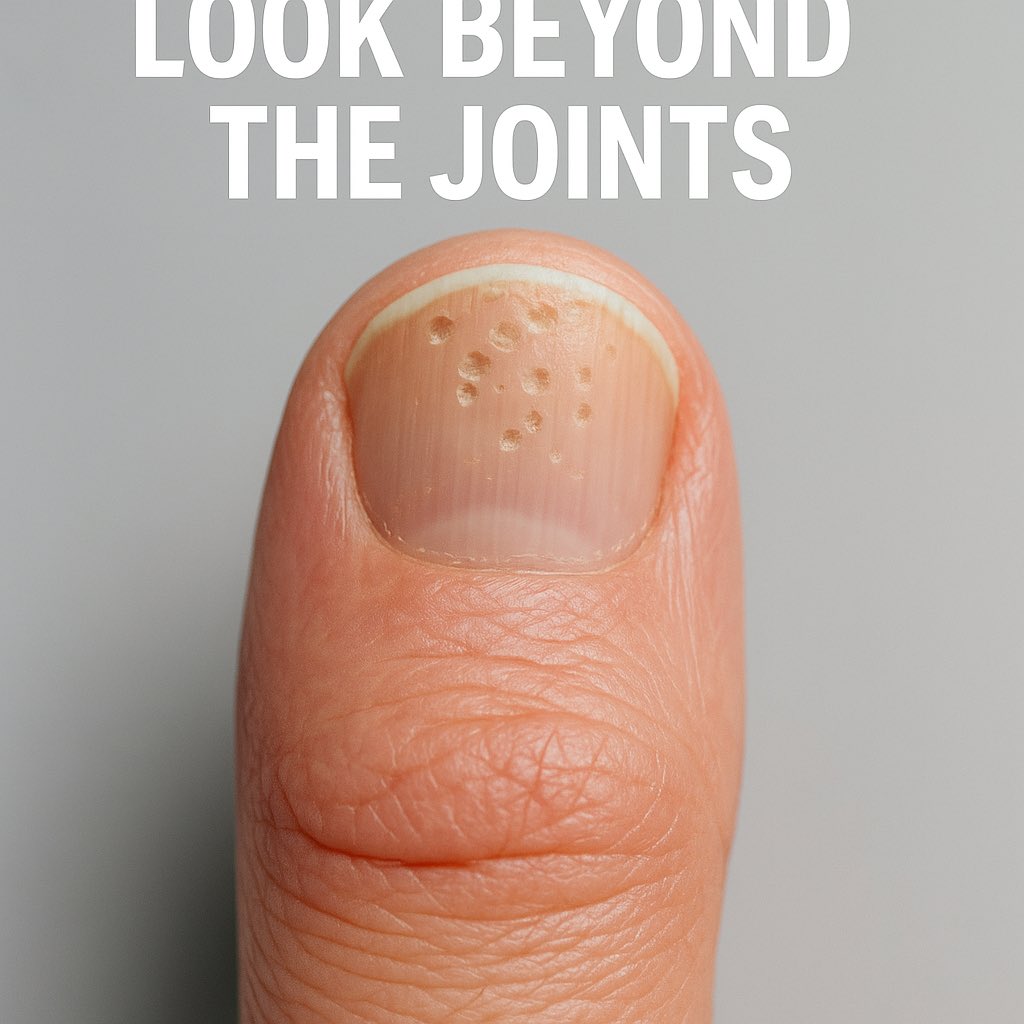
5. Psoriasis changes the game
Skin rash? Nail pitting?
Psoriatic arthritis can look just like RA—until you check the skin.
Skin rash? Nail pitting?
Psoriatic arthritis can look just like RA—until you check the skin.
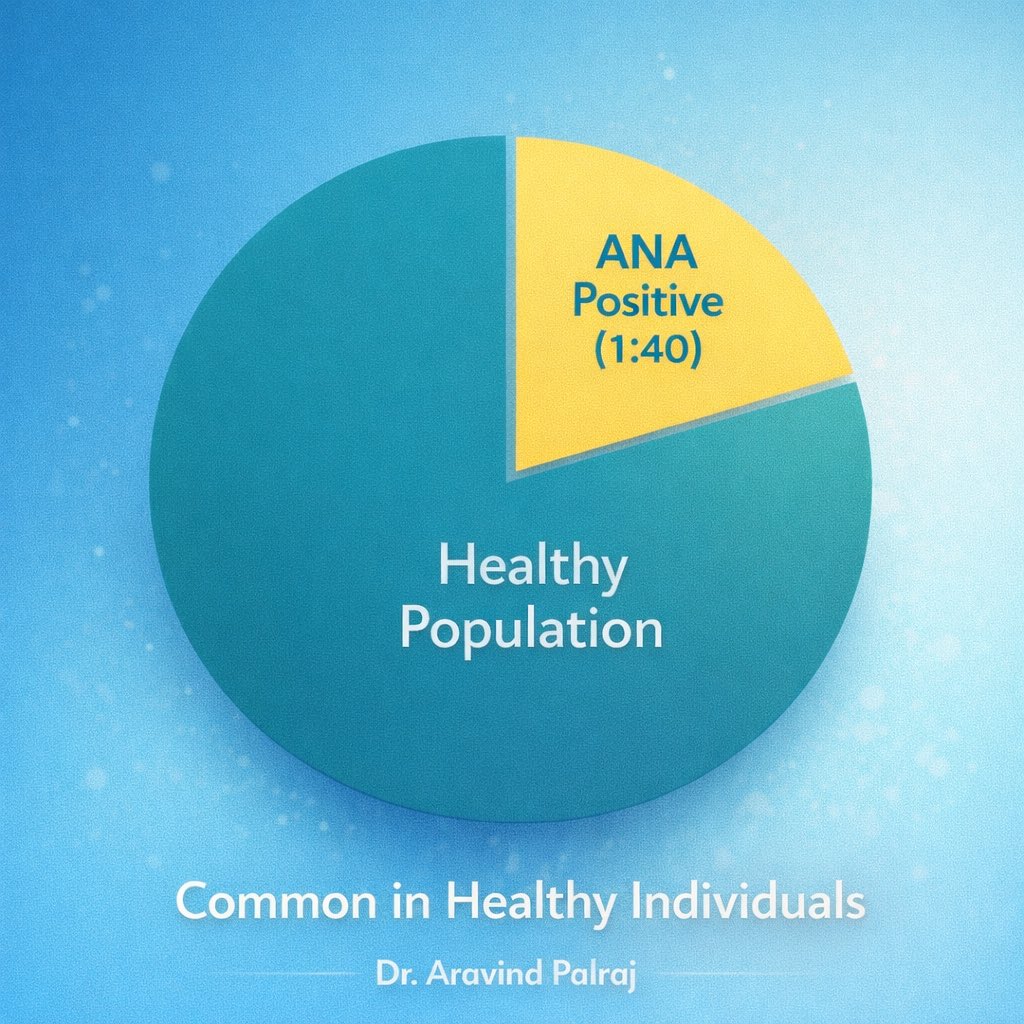
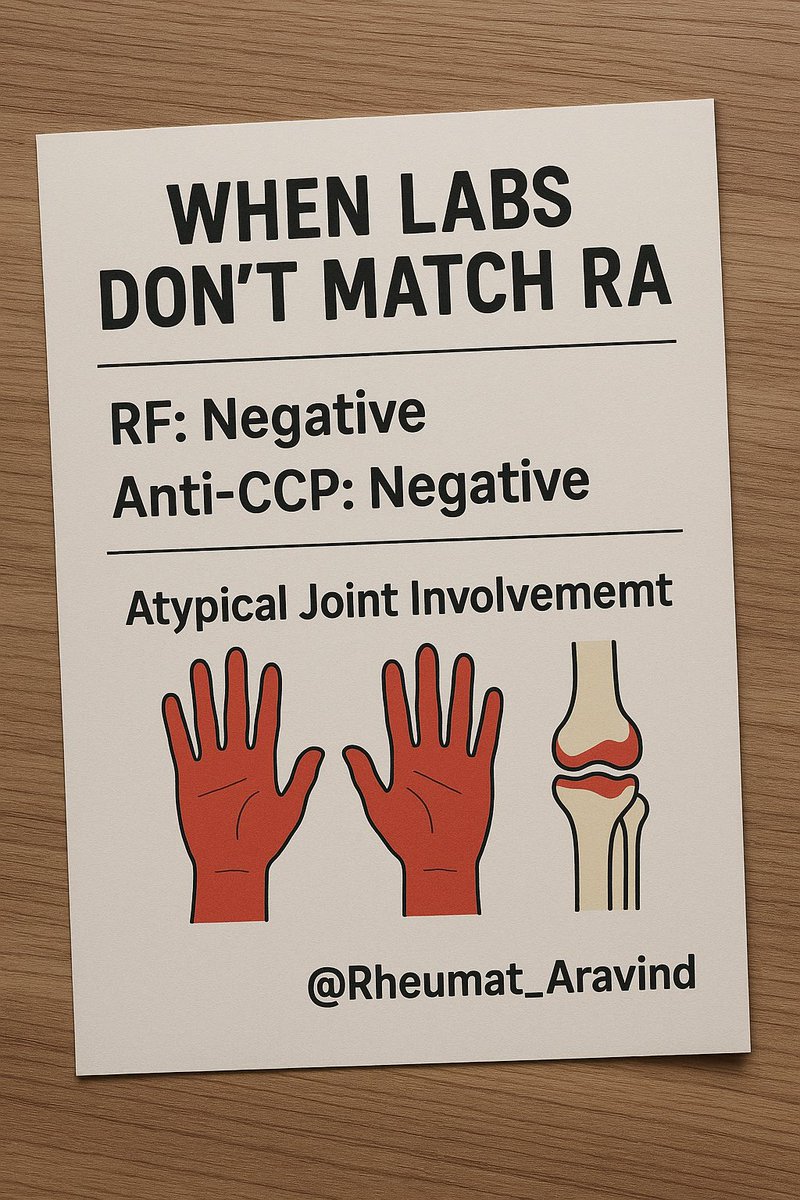
6. Negative RF & anti-CCP + weird features
If both are negative, especially with atypical joint pattern → think seronegative spondyloarthritis, lupus, viral arthritis.
If both are negative, especially with atypical joint pattern → think seronegative spondyloarthritis, lupus, viral arthritis.
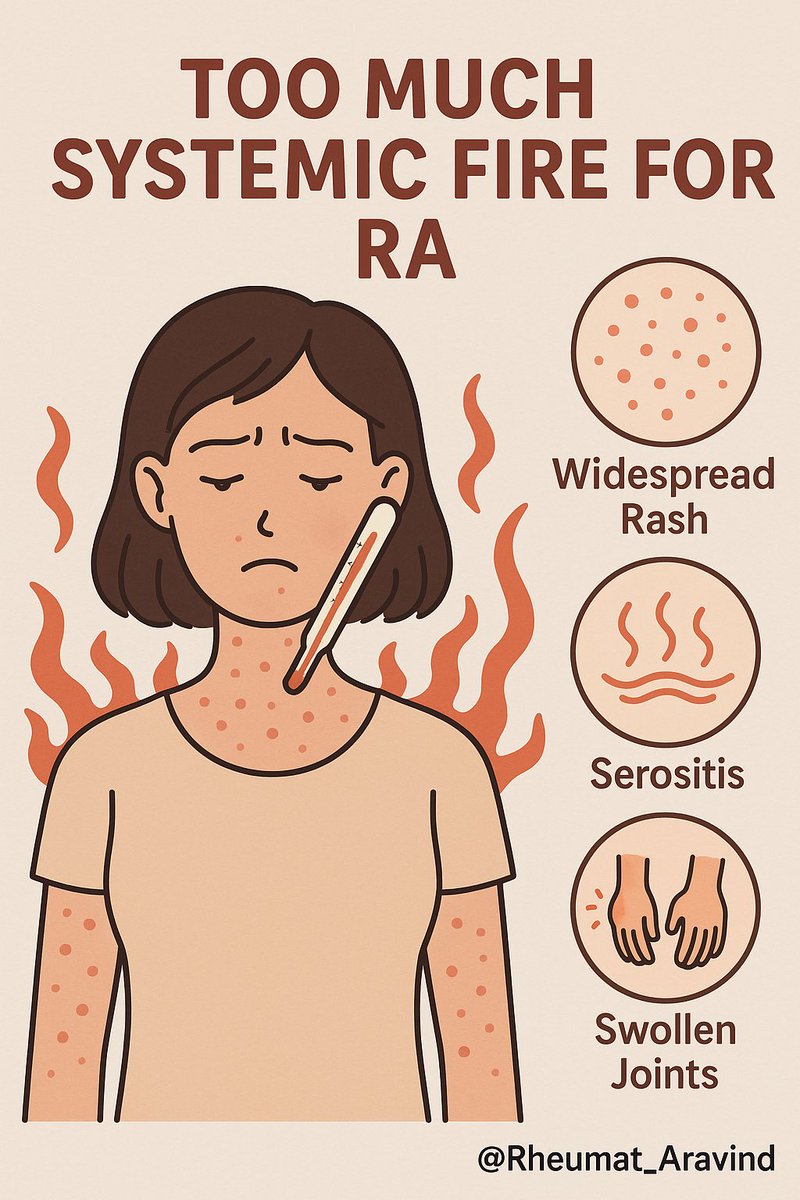
7. Systemic features out of proportion
High fever, rash, serositis, cytopenias → maybe Still’s disease, lupus, vasculitis.
High fever, rash, serositis, cytopenias → maybe Still’s disease, lupus, vasculitis.
• • •
Missing some Tweet in this thread? You can try to
force a refresh