🧵 CK Can Lie — Catching Myositis When Creatine Kinase Is Normal
Myalgia + weakness.
CK is normal.
Everyone relaxes.
That’s how dangerous myositis gets missed. Let’s fix it. 👇
@IhabFathiSulima @DrAkhilX @CelestinoGutirr #MedTwitter
Myalgia + weakness.
CK is normal.
Everyone relaxes.
That’s how dangerous myositis gets missed. Let’s fix it. 👇
@IhabFathiSulima @DrAkhilX @CelestinoGutirr #MedTwitter

1) First principle
Normal CK ≠ no muscle disease. CK reflects muscle necrosis, not strength. Patchy disease, low muscle mass, or perimysial-predominant injury can keep CK normal.
Normal CK ≠ no muscle disease. CK reflects muscle necrosis, not strength. Patchy disease, low muscle mass, or perimysial-predominant injury can keep CK normal.

2) When CK is often normal (or only mildly ↑)
•Dermatomyositis (esp. MDA5 phenotype)
•Steroid myopathy (treatment complication, not inflammation)
•Inclusion body myositis (>50 yrs; finger flexors/quads)
•Early/patchy disease, chronic burnt-out myositis
•Dermatomyositis (esp. MDA5 phenotype)
•Steroid myopathy (treatment complication, not inflammation)
•Inclusion body myositis (>50 yrs; finger flexors/quads)
•Early/patchy disease, chronic burnt-out myositis

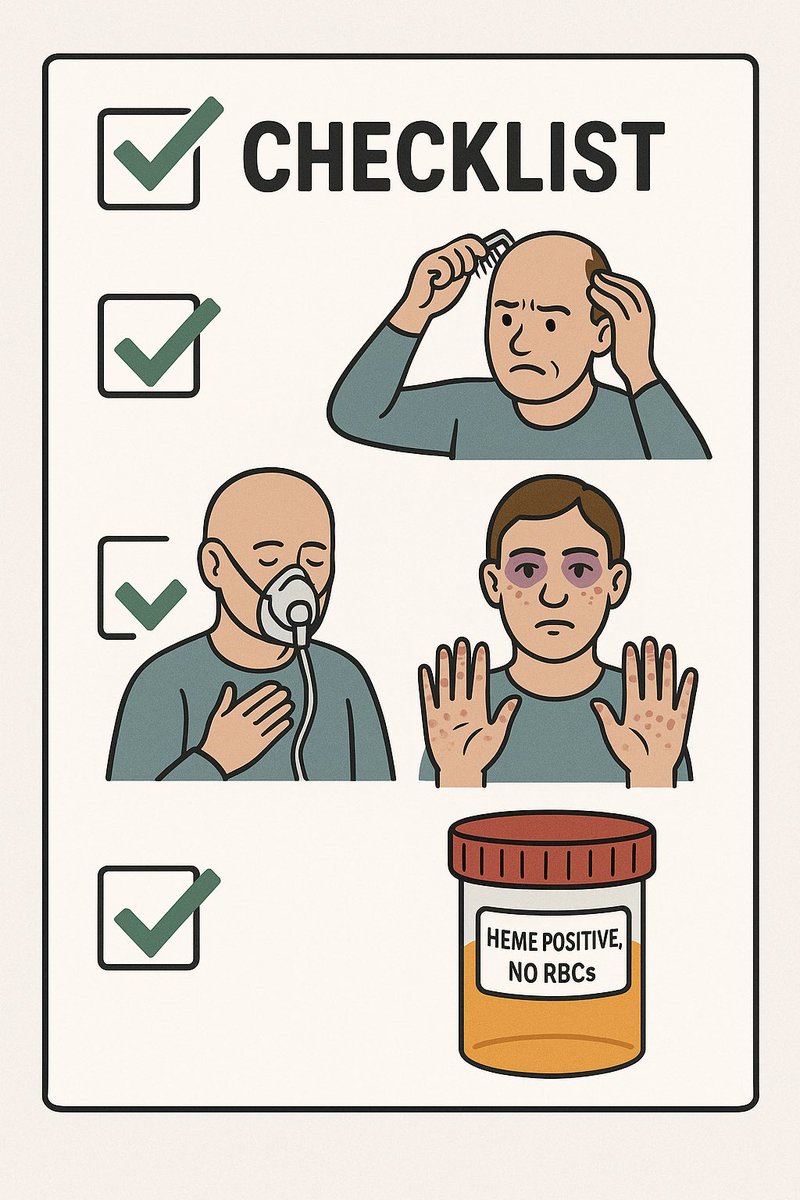
3) Red flags that trump a normal CK
•True proximal weakness (chair rise, comb hair, neck flexors)
•Dysphagia/aspiration, nasal speech, weak cough
•Dyspnea or rapid desaturation (think RP-ILD)
•Pathognomonic rashes: heliotrope, Gottron papules, mechanic’s hands
•Dark urine (heme-positive, no RBCs)
•True proximal weakness (chair rise, comb hair, neck flexors)
•Dysphagia/aspiration, nasal speech, weak cough
•Dyspnea or rapid desaturation (think RP-ILD)
•Pathognomonic rashes: heliotrope, Gottron papules, mechanic’s hands
•Dark urine (heme-positive, no RBCs)
4) What to order next (CK normal but you’re worried)
•Aldolase, LDH, AST/ALT, GGT
•AST/ALT high with normal GGT → likely muscle source
•Urine dip: heme + / RBC − → myoglobinuria
•Ferritin (very high with MDA5/RP-ILD or MAS)
•If breathless: CXR/HRCT ± PFTs
•Aldolase, LDH, AST/ALT, GGT
•AST/ALT high with normal GGT → likely muscle source
•Urine dip: heme + / RBC − → myoglobinuria
•Ferritin (very high with MDA5/RP-ILD or MAS)
•If breathless: CXR/HRCT ± PFTs
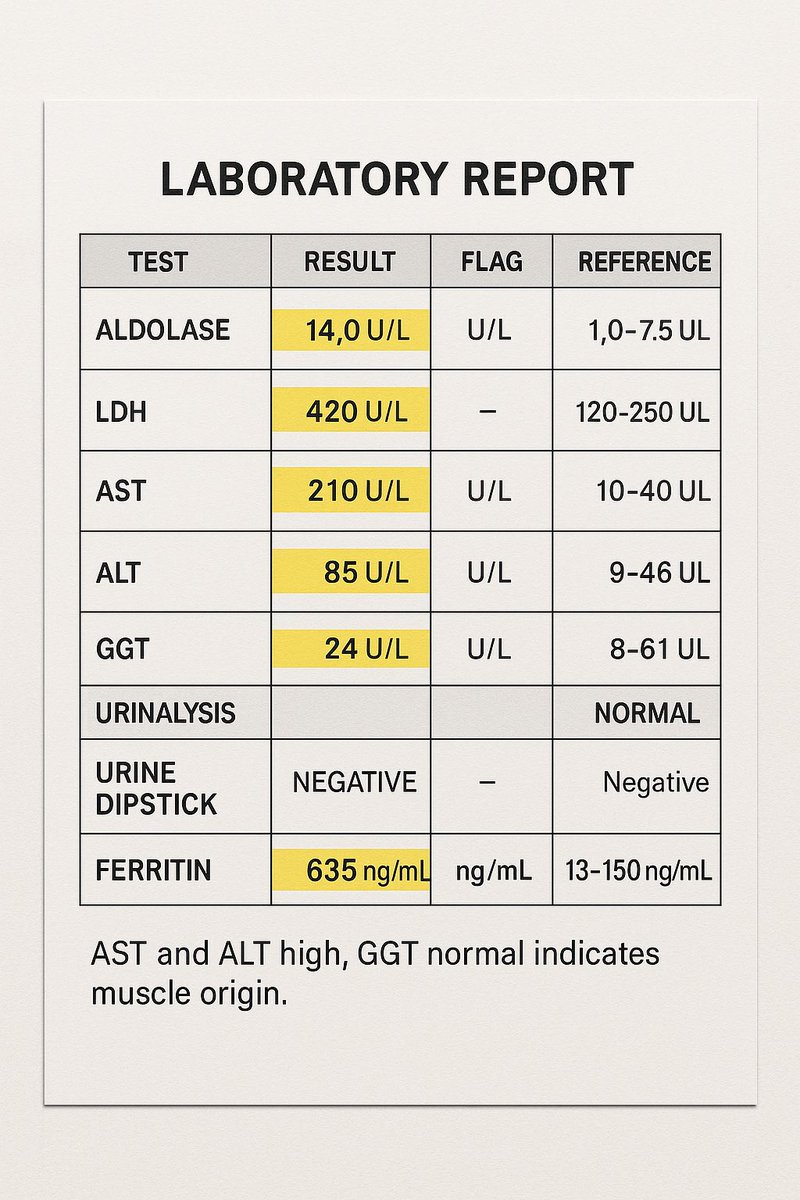
5) Pattern pearls
•CK normal + Aldolase high → perimysial process (think dermatomyositis, overlap)
•AST ≫ ALT, GGT normal → muscle, not liver
•LDH high supports muscle injury but is nonspecific
•CK normal + Aldolase high → perimysial process (think dermatomyositis, overlap)
•AST ≫ ALT, GGT normal → muscle, not liver
•LDH high supports muscle injury but is nonspecific

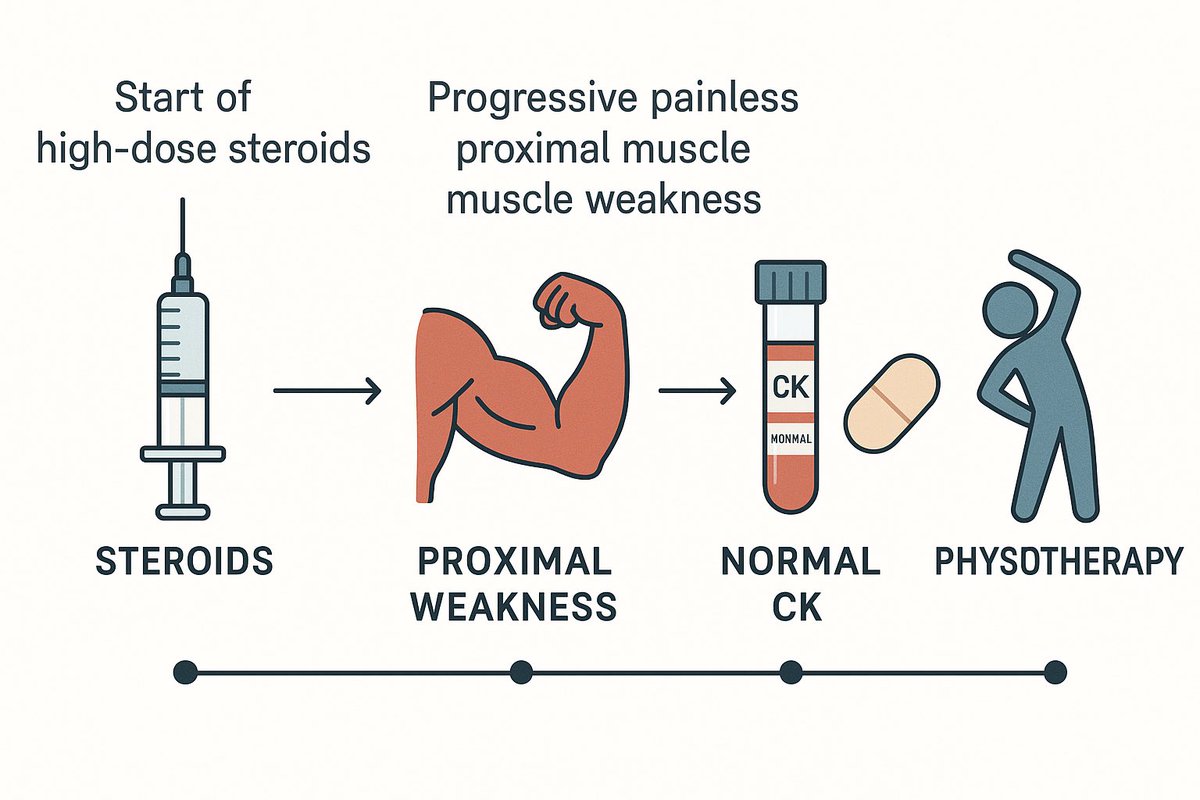
6) Don’t confuse with steroid myopathy
•Timing: weeks after starting/high-dose steroids
•Painless proximal weakness, CK normal
•Plan: taper steroids, add physio, use steroid-sparing agent for underlying rheum disease.
•Timing: weeks after starting/high-dose steroids
•Painless proximal weakness, CK normal
•Plan: taper steroids, add physio, use steroid-sparing agent for underlying rheum disease.
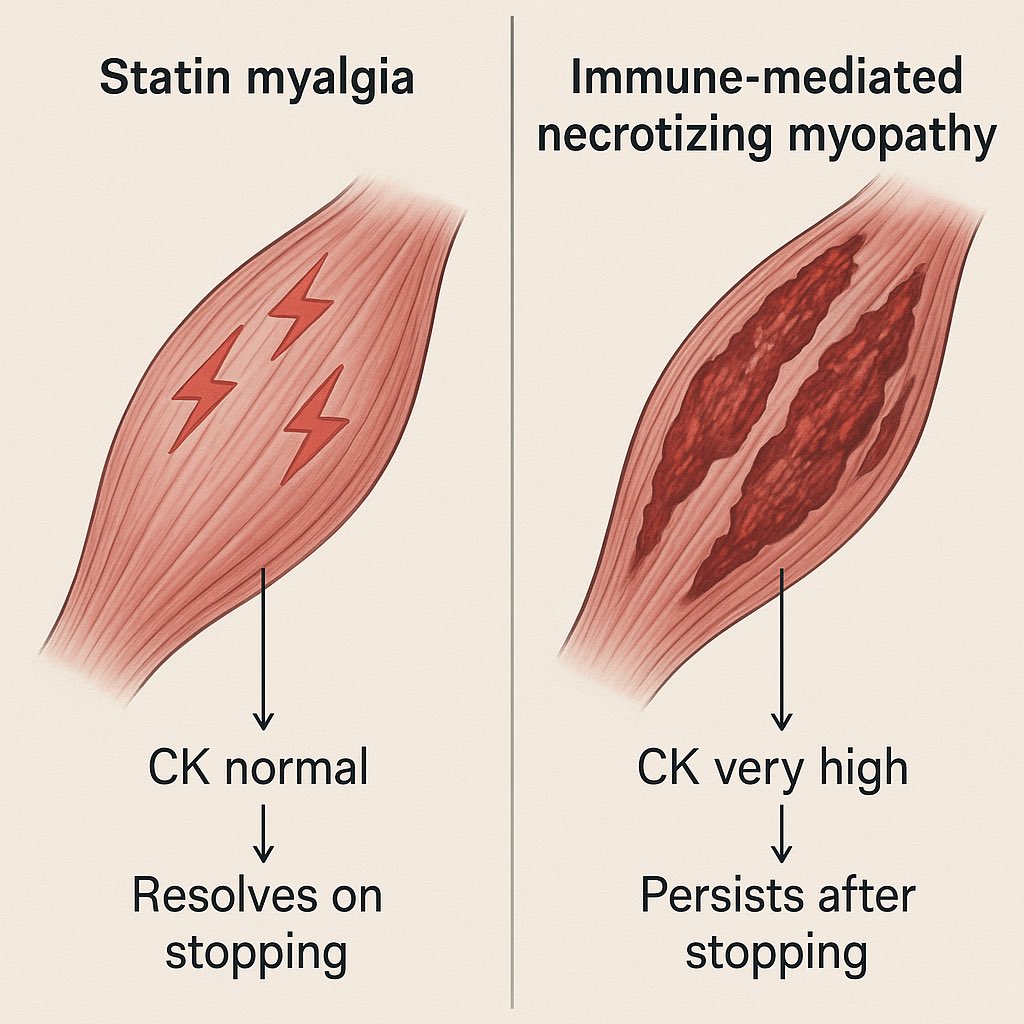
7) Statin story (two different beasts)
•Simple statin myalgia: CK normal or mild ↑; resolves on stopping
•Immune-mediated necrotizing myopathy (anti-HMGCR): very high CK, weakness persists after stopping → needs immunosuppression
•Simple statin myalgia: CK normal or mild ↑; resolves on stopping
•Immune-mediated necrotizing myopathy (anti-HMGCR): very high CK, weakness persists after stopping → needs immunosuppression
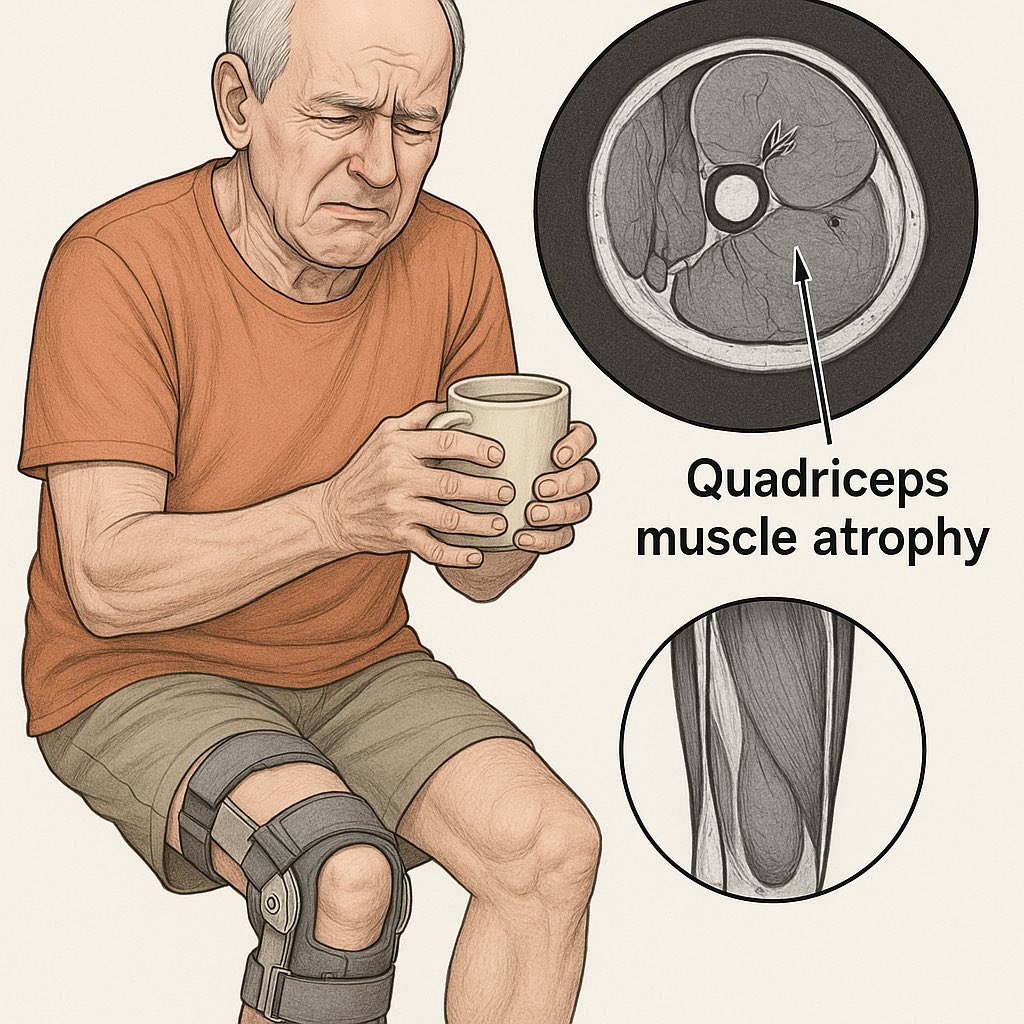
8) Inclusion body myositis (don’t overtreat like PMR/RA)
•Men >50, finger-flexor and quadriceps weakness, falls, CK normal–mild
•Poor steroid response; think biopsy, rehab, assist devices.
•Men >50, finger-flexor and quadriceps weakness, falls, CK normal–mild
•Poor steroid response; think biopsy, rehab, assist devices.
9) The lethal miss: MDA5-Dermatomyositis with RP-ILD
•Minimal/normal CK, sky-high ferritin, hand ulcers or palmar papules
•Rapidly progressive ILD → treat early (high-dose steroids + calcineurin inhibitor ± cyclophosphamide/rituximab; center-specific)
•Minimal/normal CK, sky-high ferritin, hand ulcers or palmar papules
•Rapidly progressive ILD → treat early (high-dose steroids + calcineurin inhibitor ± cyclophosphamide/rituximab; center-specific)

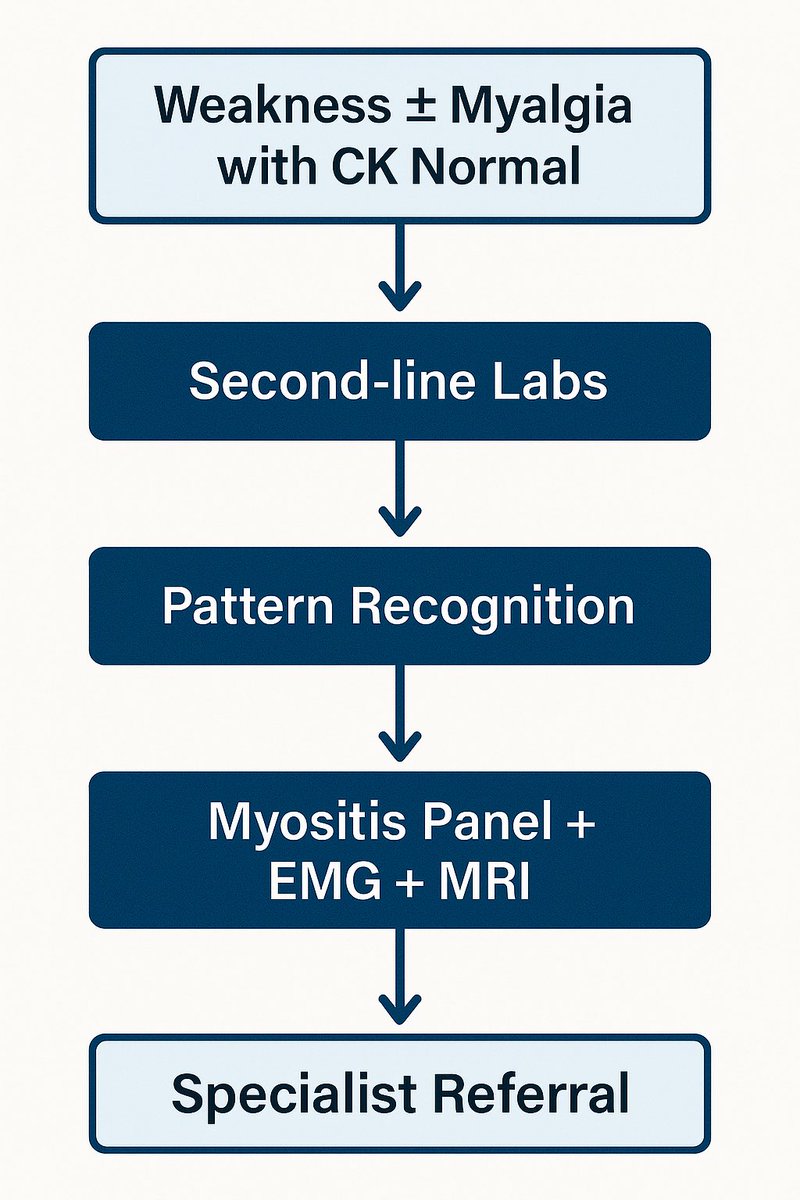
10) 30-second algorithm
Weakness ± myalgia + CK normal →
→ Check aldolase, AST/ALT, LDH, GGT, urine heme
→ Look for DM rash / IBM pattern / steroid exposure / ILD signs
→ If positive: myositis panel (MDA5, TIF1-γ, NXP2, SAE1, HMGCR, SRP, Jo-1, etc), EMG/MRI, and early rheum/pulm referral.
Weakness ± myalgia + CK normal →
→ Check aldolase, AST/ALT, LDH, GGT, urine heme
→ Look for DM rash / IBM pattern / steroid exposure / ILD signs
→ If positive: myositis panel (MDA5, TIF1-γ, NXP2, SAE1, HMGCR, SRP, Jo-1, etc), EMG/MRI, and early rheum/pulm referral.
📌 Takeaway
CK can lie. Muscles don’t.
If your exam and the story say “myositis,” keep digging even with a normal CK.
If this thread prevents one missed myositis or RP-ILD, share it. Someone will thank you later. 🔁
CK can lie. Muscles don’t.
If your exam and the story say “myositis,” keep digging even with a normal CK.
If this thread prevents one missed myositis or RP-ILD, share it. Someone will thank you later. 🔁

• • •
Missing some Tweet in this thread? You can try to
force a refresh