🧵 C3 vs C4 — What the Pattern Really Means (in 30 seconds)
We order complements all the time.
But the pattern is the diagnosis.
Here’s the fast way to read C3/C4 without overthinking. 👇
@IhabFathiSulima @DrAkhilX @CelestinoGutirr @DurgaPrasannaM1 @SarahSchaferMD @EMJNephrology #MedTwitter #Rheumatology
We order complements all the time.
But the pattern is the diagnosis.
Here’s the fast way to read C3/C4 without overthinking. 👇
@IhabFathiSulima @DrAkhilX @CelestinoGutirr @DurgaPrasannaM1 @SarahSchaferMD @EMJNephrology #MedTwitter #Rheumatology

1) Quick primer
•C3 = shared hub (alternative + classical).
•C4 = classical pathway marker (C1q → C4).
Pattern > any single value.
•C3 = shared hub (alternative + classical).
•C4 = classical pathway marker (C1q → C4).
Pattern > any single value.

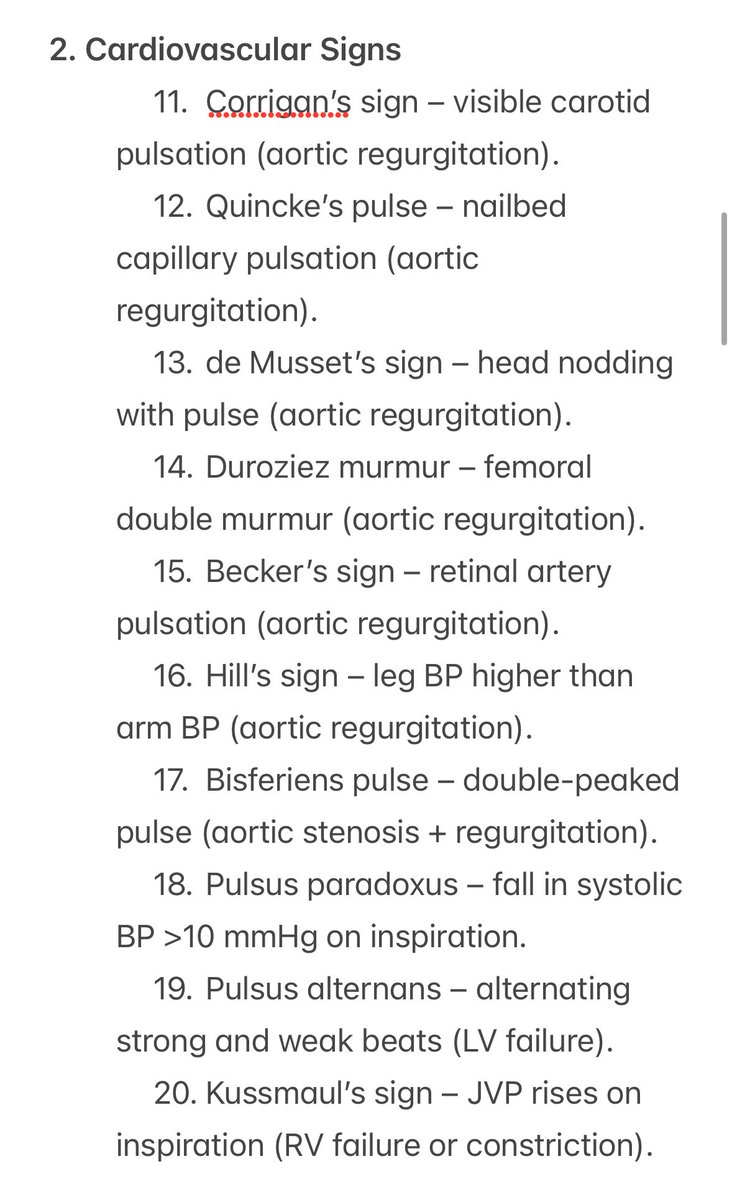
2) Both C3 ↓ and C4 ↓ → immune-complex “classical burn”
Think: active SLE, infective endocarditis, serum-sickness/drug IC, mixed cryoglobulinemia.
Next: CH50, anti-dsDNA, C1q binding/anti-C1q, blood cultures if febrile.
Think: active SLE, infective endocarditis, serum-sickness/drug IC, mixed cryoglobulinemia.
Next: CH50, anti-dsDNA, C1q binding/anti-C1q, blood cultures if febrile.
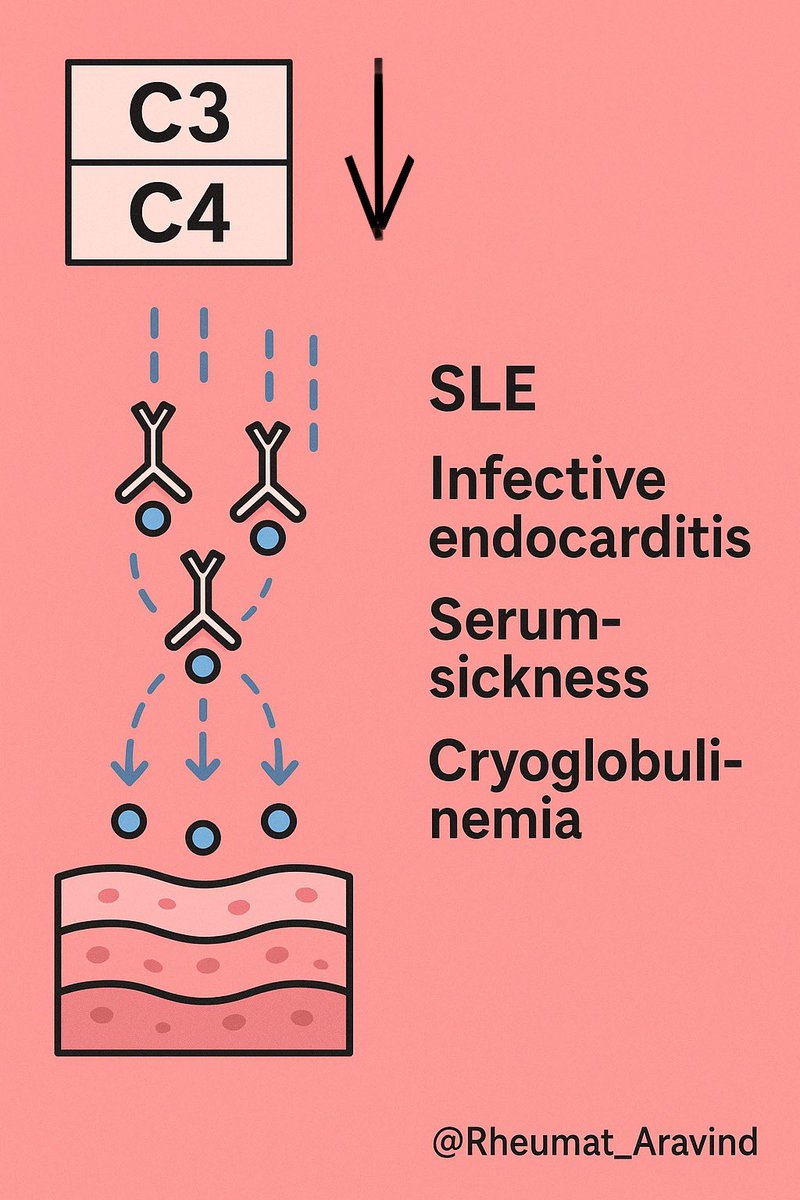
3) C3 ↓ with C4 normal → alternative pathway
Think: post-infectious GN, C3 glomerulopathy, atypical HUS.
Next: AH50, C3 nephritic factor, factor H/I, renal workup.
Think: post-infectious GN, C3 glomerulopathy, atypical HUS.
Next: AH50, C3 nephritic factor, factor H/I, renal workup.
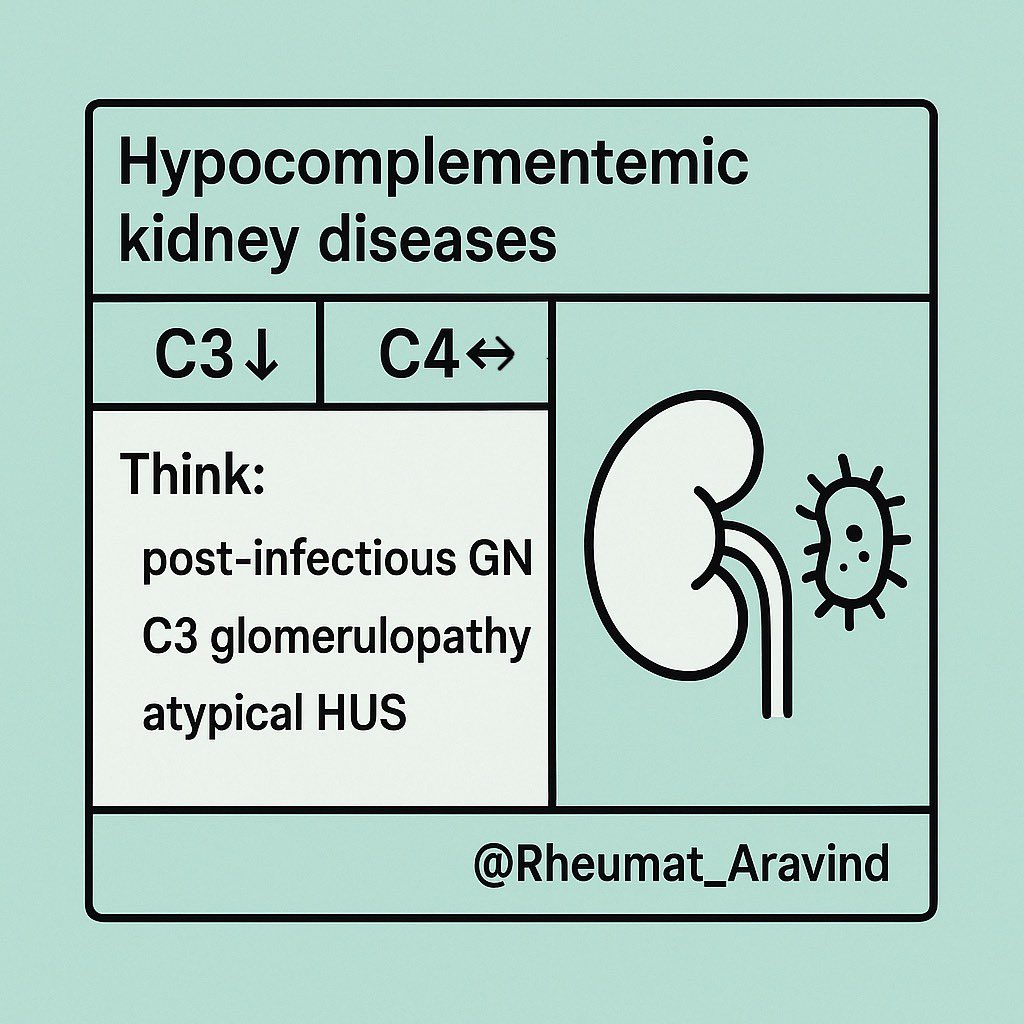
4) C3 normal with C4 ↓ → early classical activation/C1 issues
Think: hereditary or acquired C1-inhibitor deficiency (HAE), cold agglutinin disease, cryoglobulinemia (often C4 ≪ C3).
Next: C1-INH level/function, C1q, hemolysis workup, hepatitis serology.
Think: hereditary or acquired C1-inhibitor deficiency (HAE), cold agglutinin disease, cryoglobulinemia (often C4 ≪ C3).
Next: C1-INH level/function, C1q, hemolysis workup, hepatitis serology.
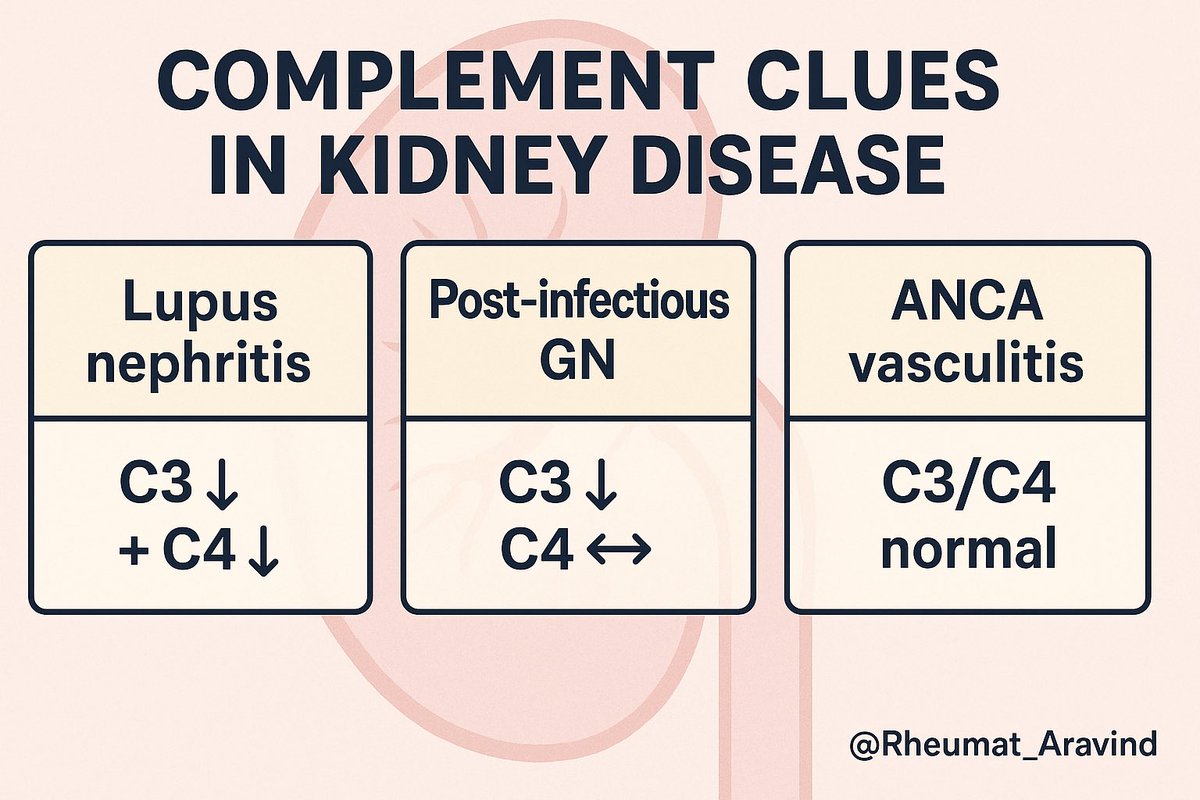
5) Kidneys cheat-sheet
•Lupus nephritis: C3 ↓ + C4 ↓
•Post-infectious GN / C3G: C3 ↓, C4 ↔
•ANCA vasculitis: C3/C4 usually normal
•Lupus nephritis: C3 ↓ + C4 ↓
•Post-infectious GN / C3G: C3 ↓, C4 ↔
•ANCA vasculitis: C3/C4 usually normal
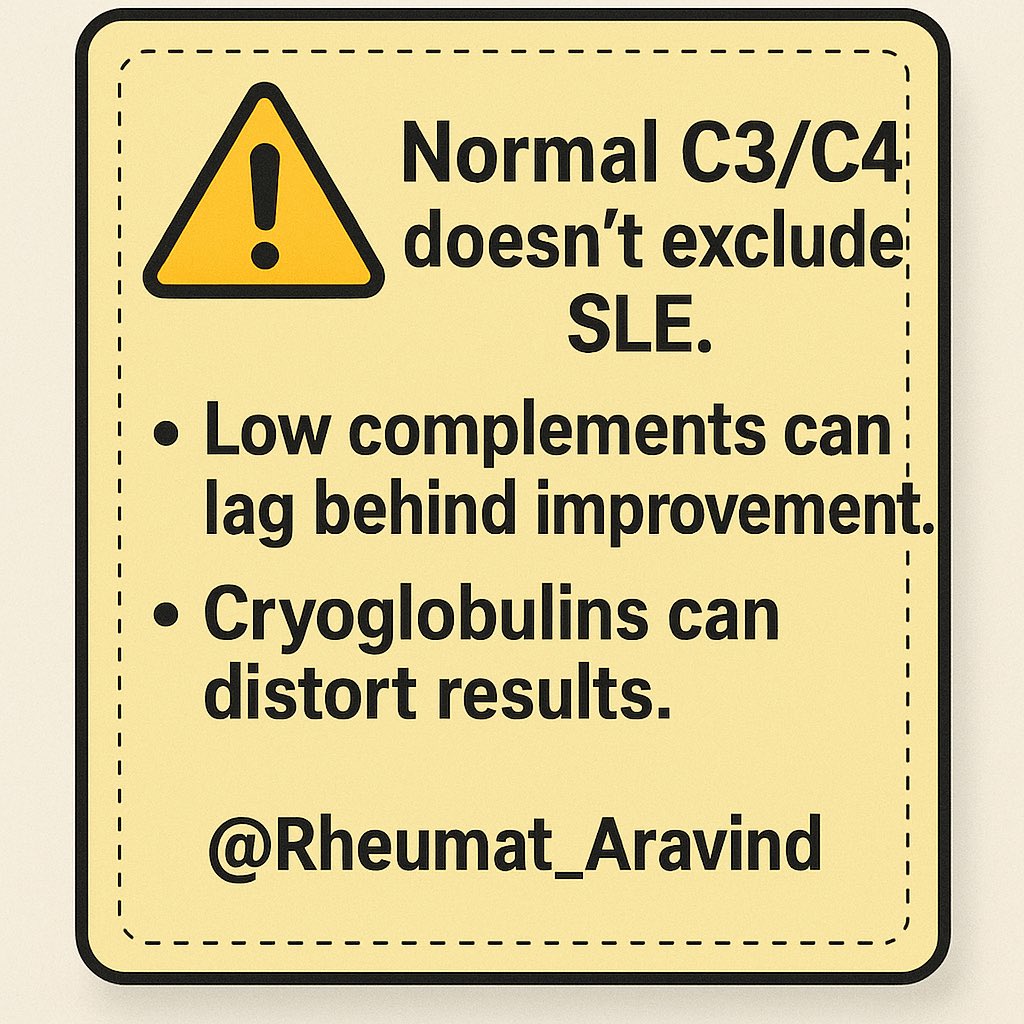
6) Pitfalls
•Normal complements do not exclude SLE (C3 is an acute-phase reactant).
•Low complements can lag behind clinical improvement.
•Lab interference (cryoglobulins) can distort results—warm the sample.
•Normal complements do not exclude SLE (C3 is an acute-phase reactant).
•Low complements can lag behind clinical improvement.
•Lab interference (cryoglobulins) can distort results—warm the sample.
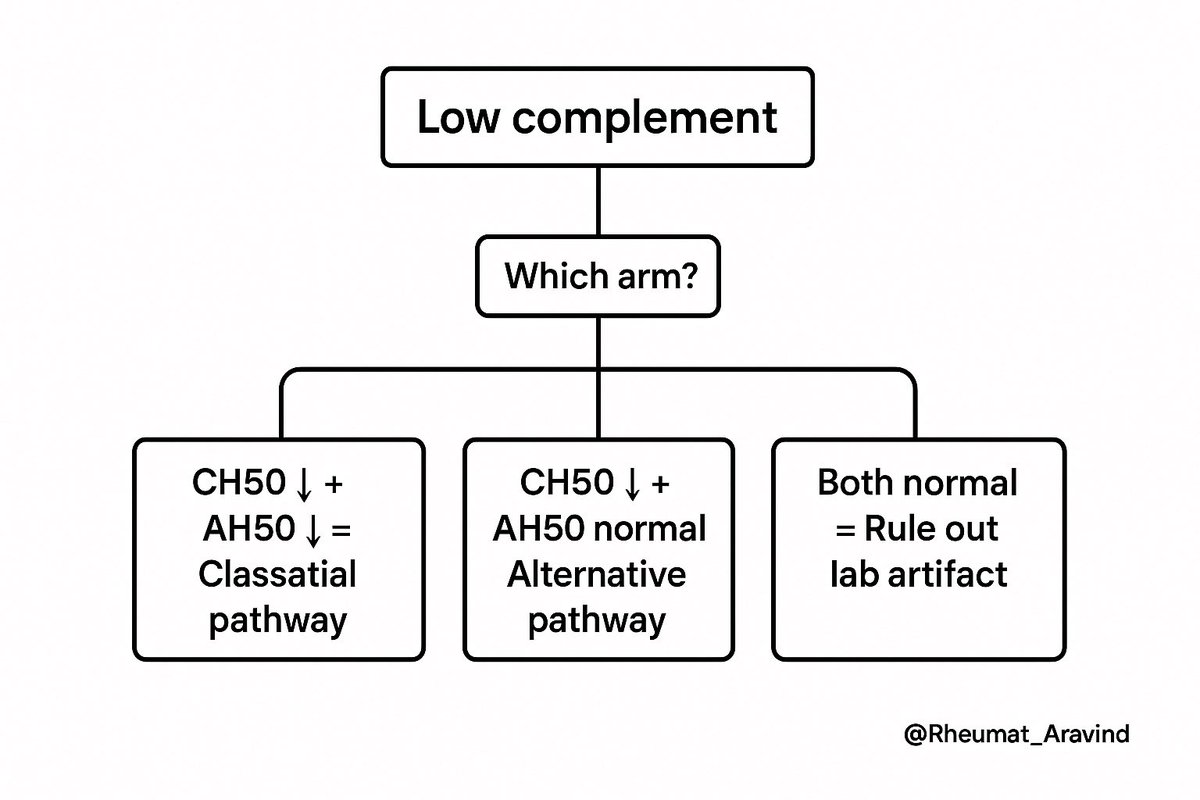
7) What to add when unsure
Order CH50 & AH50 together → tells you which arm is broken.
If angioedema: add C1q + C1-INH level & function.
If GN: add urine protein/Cr, microscopy, serologies, consider biopsy.
Order CH50 & AH50 together → tells you which arm is broken.
If angioedema: add C1q + C1-INH level & function.
If GN: add urine protein/Cr, microscopy, serologies, consider biopsy.
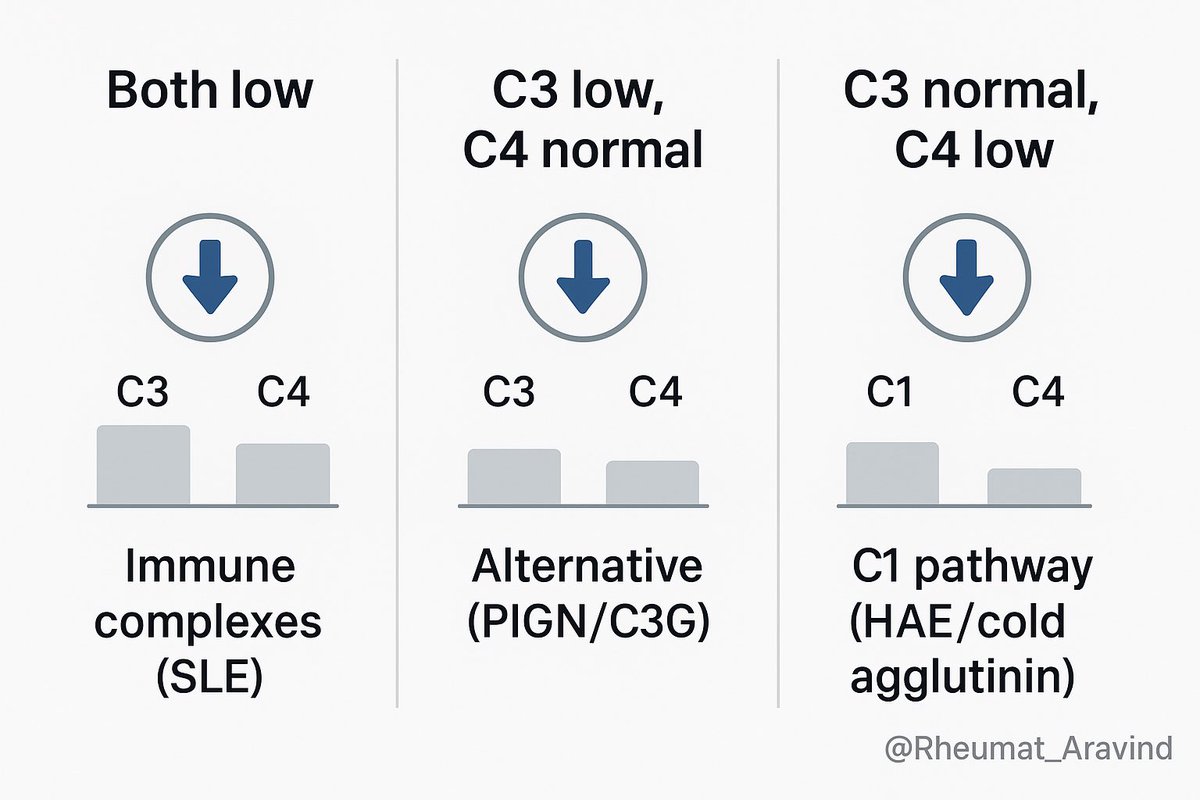
📌 Takeaway
Read complements like an ECG: pattern first.
•Both low → immune complexes (think SLE).
•C3 low, C4 normal → alternative (think PIGN/C3G).
•C3 normal, C4 low → C1 pathway (think HAE/cold agglutinin).
Context decides the rest.
#neetpg2025 #NEETPG
Read complements like an ECG: pattern first.
•Both low → immune complexes (think SLE).
•C3 low, C4 normal → alternative (think PIGN/C3G).
•C3 normal, C4 low → C1 pathway (think HAE/cold agglutinin).
Context decides the rest.
#neetpg2025 #NEETPG
• • •
Missing some Tweet in this thread? You can try to
force a refresh