🧵 Giant Cell Arteritis — Save a Sight in 5 Minutes
The vision loss is often permanent—and preventable.
A zero-fluff checklist: who to treat before tests, when ultrasound beats biopsy, steroid start & taper, and the traps (normal ESR/CRP, “PMR only,” jaw pain without headache).
@IhabFathiSulima @DrAkhilX @CelestinoGutirr @Janetbirdope @vascuk #MedTwitter #NEETPG
The vision loss is often permanent—and preventable.
A zero-fluff checklist: who to treat before tests, when ultrasound beats biopsy, steroid start & taper, and the traps (normal ESR/CRP, “PMR only,” jaw pain without headache).
@IhabFathiSulima @DrAkhilX @CelestinoGutirr @Janetbirdope @vascuk #MedTwitter #NEETPG
Why this matters
•GCA is the most common primary vasculitis >50 years
•~15–20% develop vision loss — often before diagnosis
•Half lose the other eye within days if untreated
•Risk drops almost to zero with prompt steroids
•GCA is the most common primary vasculitis >50 years
•~15–20% develop vision loss — often before diagnosis
•Half lose the other eye within days if untreated
•Risk drops almost to zero with prompt steroids

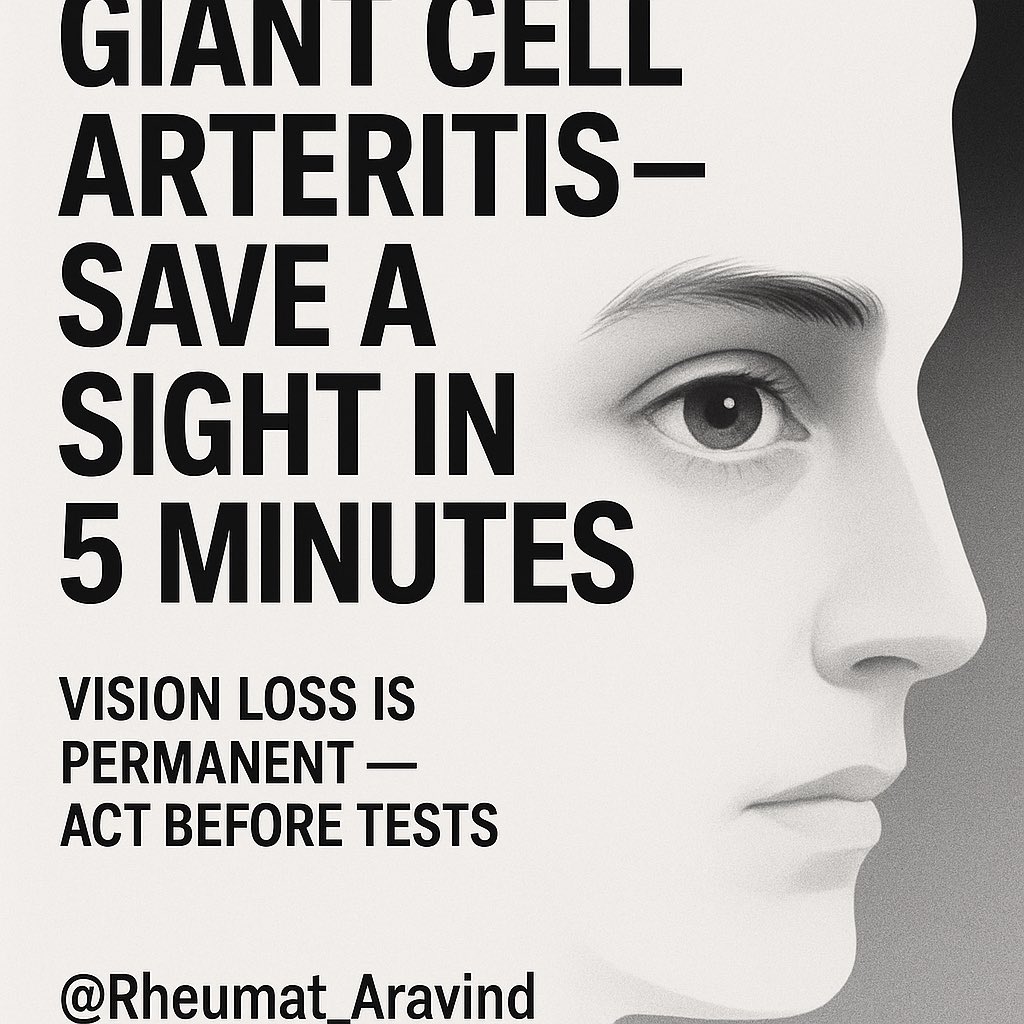
Classic presentation
•Age ≥50
•New headache (often temporal)
•Jaw claudication (highly specific)
•Visual blurring / loss
•Scalp tenderness (pain on combing hair)
•± Polymyalgia rheumatica symptoms
•Age ≥50
•New headache (often temporal)
•Jaw claudication (highly specific)
•Visual blurring / loss
•Scalp tenderness (pain on combing hair)
•± Polymyalgia rheumatica symptoms
Red flags you must know
Treat before waiting for confirmatory tests if:
•Jaw claudication
•Vision loss/blurring
•Pale swollen optic disc on fundoscopy
•Temporal artery: tender, thick, pulseless
•Unexplained fever + ESR/CRP ↑ in patient >50
Treat before waiting for confirmatory tests if:
•Jaw claudication
•Vision loss/blurring
•Pale swollen optic disc on fundoscopy
•Temporal artery: tender, thick, pulseless
•Unexplained fever + ESR/CRP ↑ in patient >50

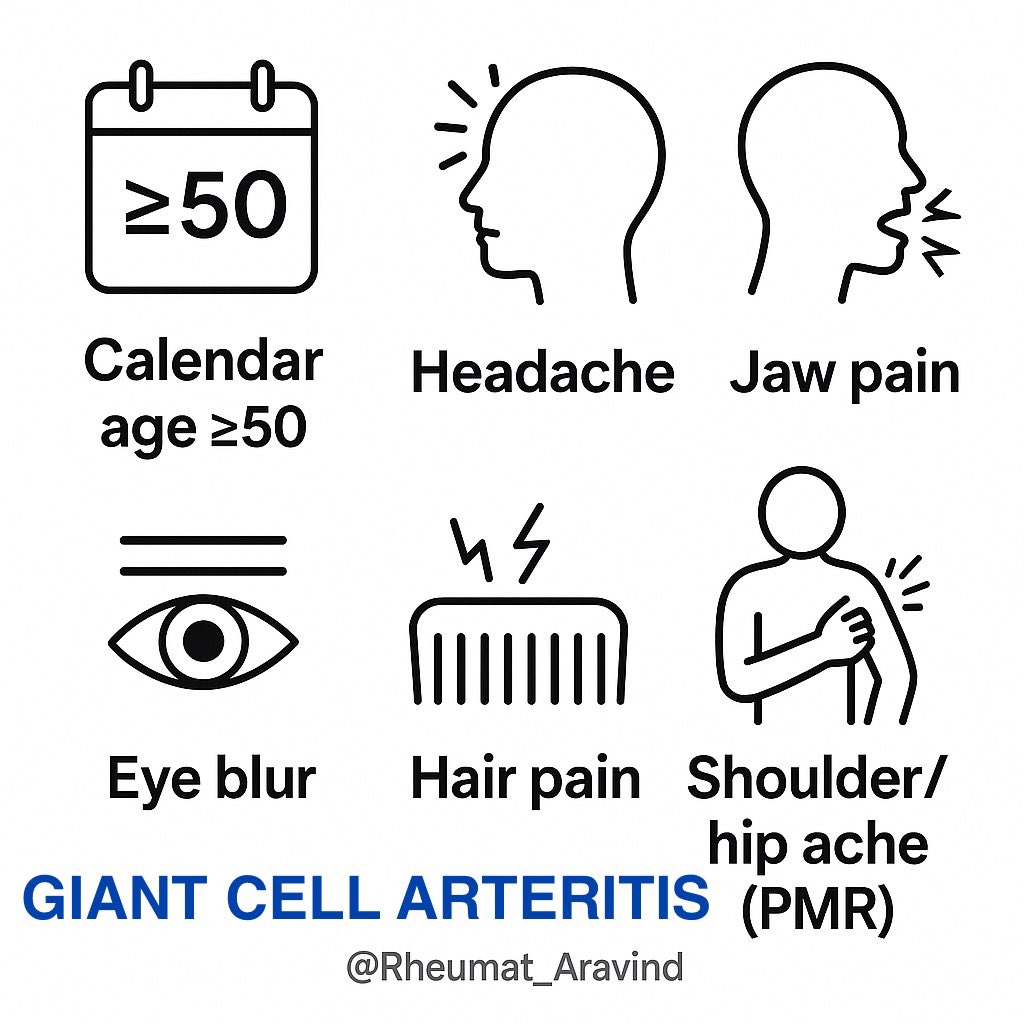
ESR & CRP are helpful but not perfect
•ESR >50 mm/hr in most — but can be normal
•CRP ↑ in ~97% — better sensitivity than ESR
•If suspicion is high → start steroids immediately
•ESR >50 mm/hr in most — but can be normal
•CRP ↑ in ~97% — better sensitivity than ESR
•If suspicion is high → start steroids immediately
First-line tests (don’t delay steroids)
•Temporal artery ultrasound (halo sign) — sensitivity highest if done <1 week after steroid start
•Temporal artery biopsy — gold standard but can be false negative (skip lesions)
•Consider PET-CT if large-vessel GCA suspected
•Temporal artery ultrasound (halo sign) — sensitivity highest if done <1 week after steroid start
•Temporal artery biopsy — gold standard but can be false negative (skip lesions)
•Consider PET-CT if large-vessel GCA suspected

Immediate management
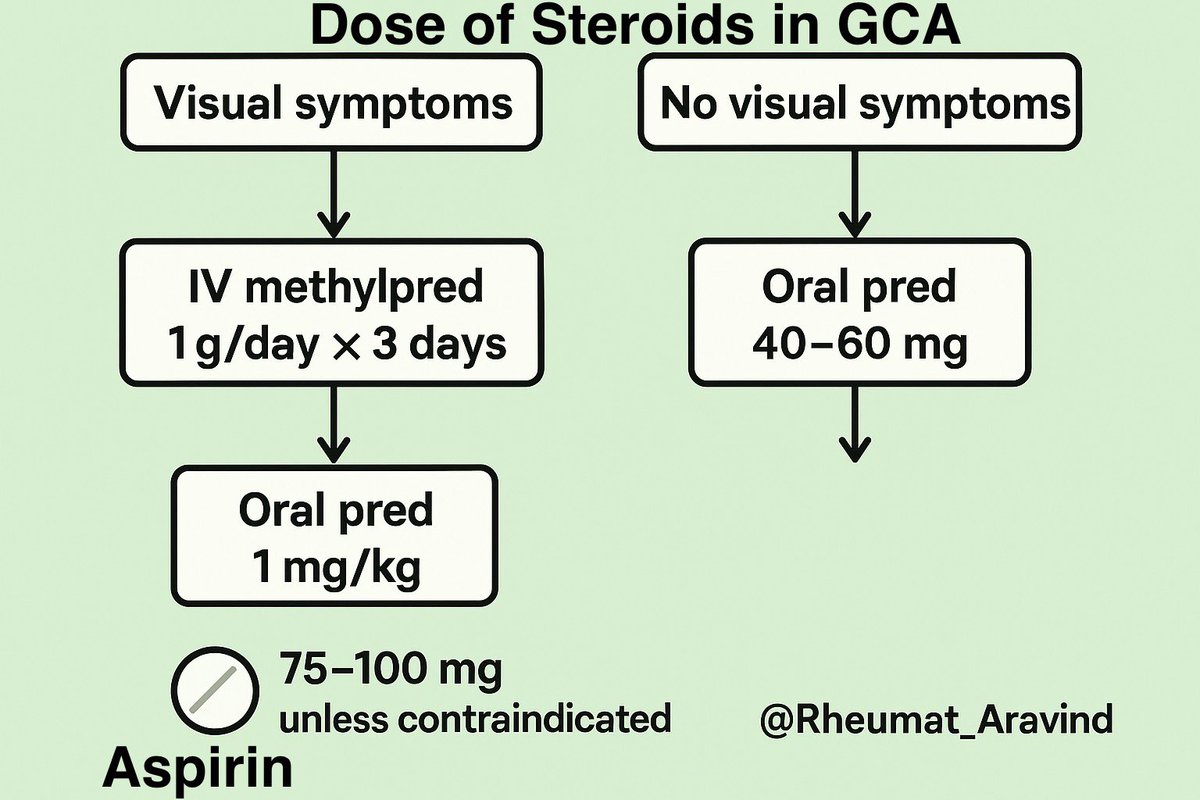
•Visual symptoms: IV methylprednisolone 1 g/day × 3 days, then oral prednisolone 1 mg/kg
•No visual symptoms: oral prednisolone 40–60 mg daily
•Aspirin 75–100 mg daily (reduces cranial ischemic events) unless contraindicated
•Visual symptoms: IV methylprednisolone 1 g/day × 3 days, then oral prednisolone 1 mg/kg
•No visual symptoms: oral prednisolone 40–60 mg daily
•Aspirin 75–100 mg daily (reduces cranial ischemic events) unless contraindicated
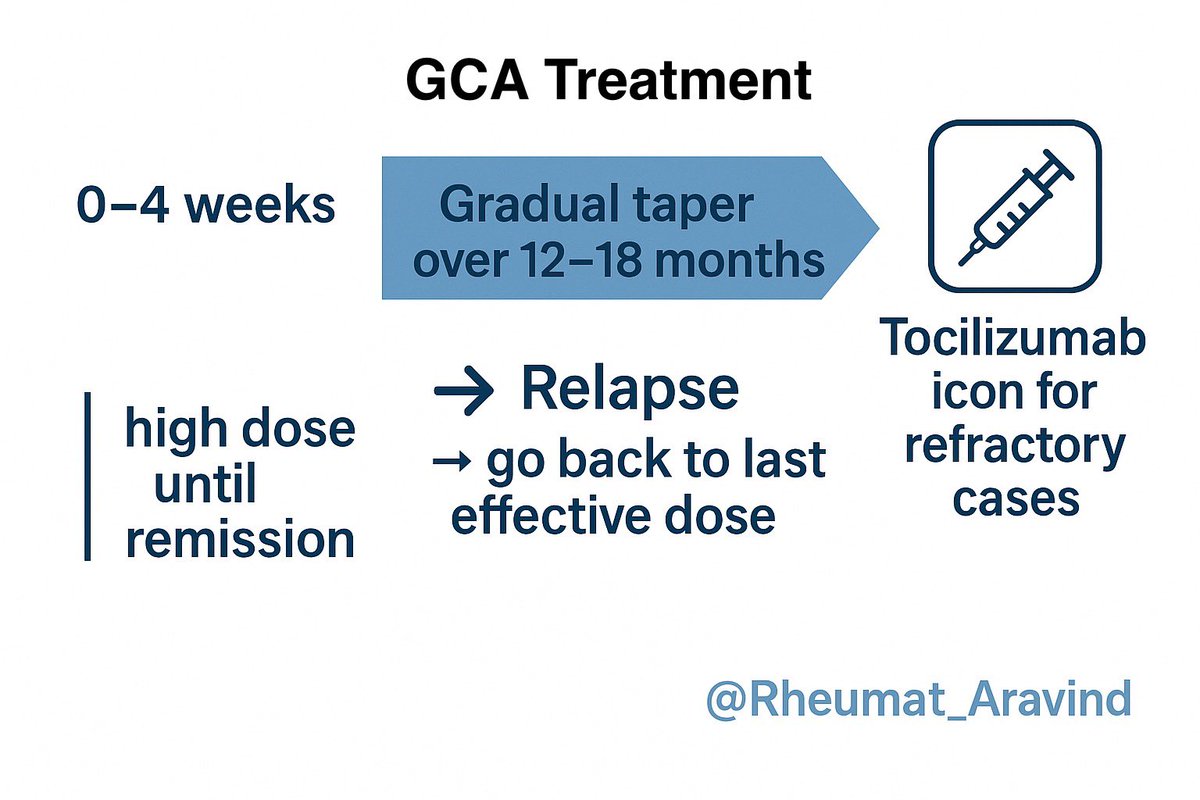
Steroid taper roadmap
•Maintain high dose until symptoms and labs normal (~2–4 wks)
•Gradual taper over 12–18 months
•Relapse = re-escalate to last effective dose
•Consider tocilizumab for relapsing/refractory or steroid-sparing
•Maintain high dose until symptoms and labs normal (~2–4 wks)
•Gradual taper over 12–18 months
•Relapse = re-escalate to last effective dose
•Consider tocilizumab for relapsing/refractory or steroid-sparing
Common traps
•ESR normal (up to 5%) → don’t rule out
•“Only PMR symptoms” can be GCA
•Jaw claudication without headache → still GCA
•Biopsy negative ≠ no GCA (skip lesions)
•ESR normal (up to 5%) → don’t rule out
•“Only PMR symptoms” can be GCA
•Jaw claudication without headache → still GCA
•Biopsy negative ≠ no GCA (skip lesions)

Takeaway
Rule of sight in GCA:
If you think it’s GCA, start steroids now.
You can always stop them later — but you can’t give sight back.
📌 Save this — you might save a sight one day.
Rule of sight in GCA:
If you think it’s GCA, start steroids now.
You can always stop them later — but you can’t give sight back.
📌 Save this — you might save a sight one day.
• • •
Missing some Tweet in this thread? You can try to
force a refresh