🧵🤰💊 Managing Rheumatoid Arthritis during pregnancy & breastfeeding isn’t just about the right meds — it’s about timing, planning, and protecting both mum & baby.
Here’s your evidence-based, easy-to-follow guide 👇
@IhabFathiSulima @DrAkhilX @CelestinoGutirr @DurgaPrasannaM1 @RA_information #MedTwitter #Rheumatology
Here’s your evidence-based, easy-to-follow guide 👇
@IhabFathiSulima @DrAkhilX @CelestinoGutirr @DurgaPrasannaM1 @RA_information #MedTwitter #Rheumatology
1️⃣ Planning is key
RA and pregnancy can coexist safely with the right plan.
Pre-pregnancy counselling is essential — discuss disease control, medication safety, and timing of conception.
RA and pregnancy can coexist safely with the right plan.
Pre-pregnancy counselling is essential — discuss disease control, medication safety, and timing of conception.
2️⃣ Disease activity matters
Best pregnancy outcomes happen when RA is in remission or low activity for ≥3–6 months before conception.
Active disease → ↑ risk of miscarriage, preterm birth, and growth restriction.
Best pregnancy outcomes happen when RA is in remission or low activity for ≥3–6 months before conception.
Active disease → ↑ risk of miscarriage, preterm birth, and growth restriction.

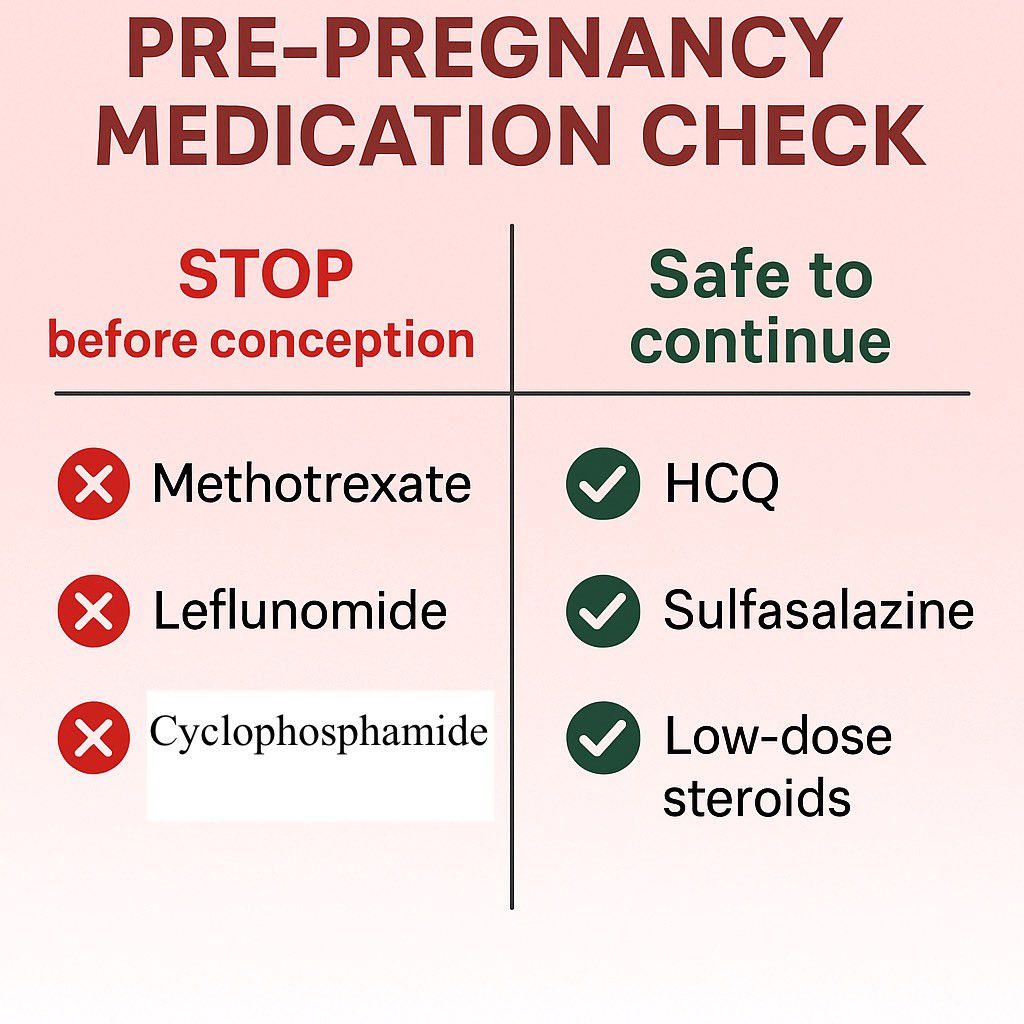
3️⃣ Pre-pregnancy medication check
Some drugs must be stopped well before conception:
❌ Methotrexate — stop ≥3 months before
❌ Leflunomide — cholestyramine washout needed
❌ Cyclophosphamide — avoid completely
✅ Hydroxychloroquine, sulfasalazine, low-dose steroids are safe
Some drugs must be stopped well before conception:
❌ Methotrexate — stop ≥3 months before
❌ Leflunomide — cholestyramine washout needed
❌ Cyclophosphamide — avoid completely
✅ Hydroxychloroquine, sulfasalazine, low-dose steroids are safe
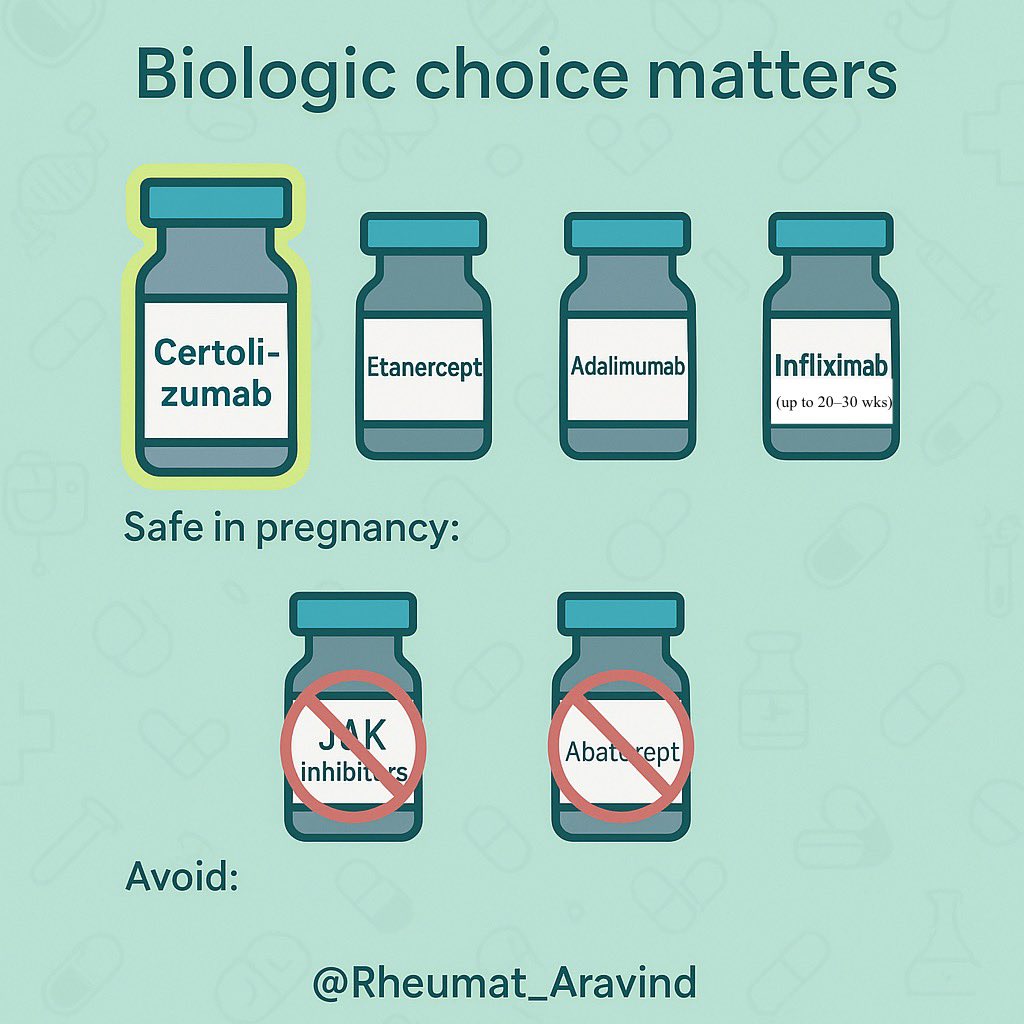
4️⃣ Biologics & tsDMARDs
•Certolizumab pegol: safest TNF inhibitor in pregnancy (minimal placental transfer)
•Etanercept, adalimumab, infliximab: can be used until 20–30 weeks if needed
•Avoid JAK inhibitors & abatacept in pregnancy
•Certolizumab pegol: safest TNF inhibitor in pregnancy (minimal placental transfer)
•Etanercept, adalimumab, infliximab: can be used until 20–30 weeks if needed
•Avoid JAK inhibitors & abatacept in pregnancy
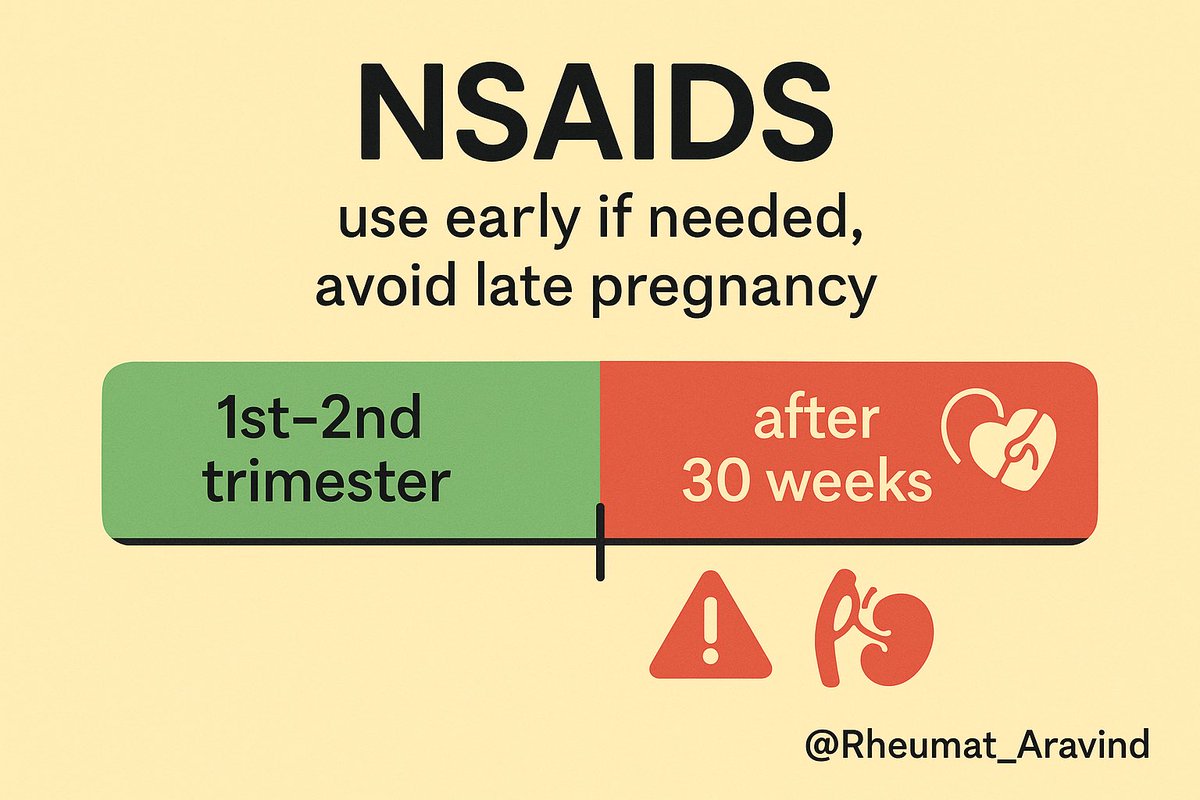
5️⃣ NSAIDs
•Can be used in 1st & 2nd trimesters if essential
•Avoid after 30 weeks (risk of ductus arteriosus closure)
•Can be used in 1st & 2nd trimesters if essential
•Avoid after 30 weeks (risk of ductus arteriosus closure)
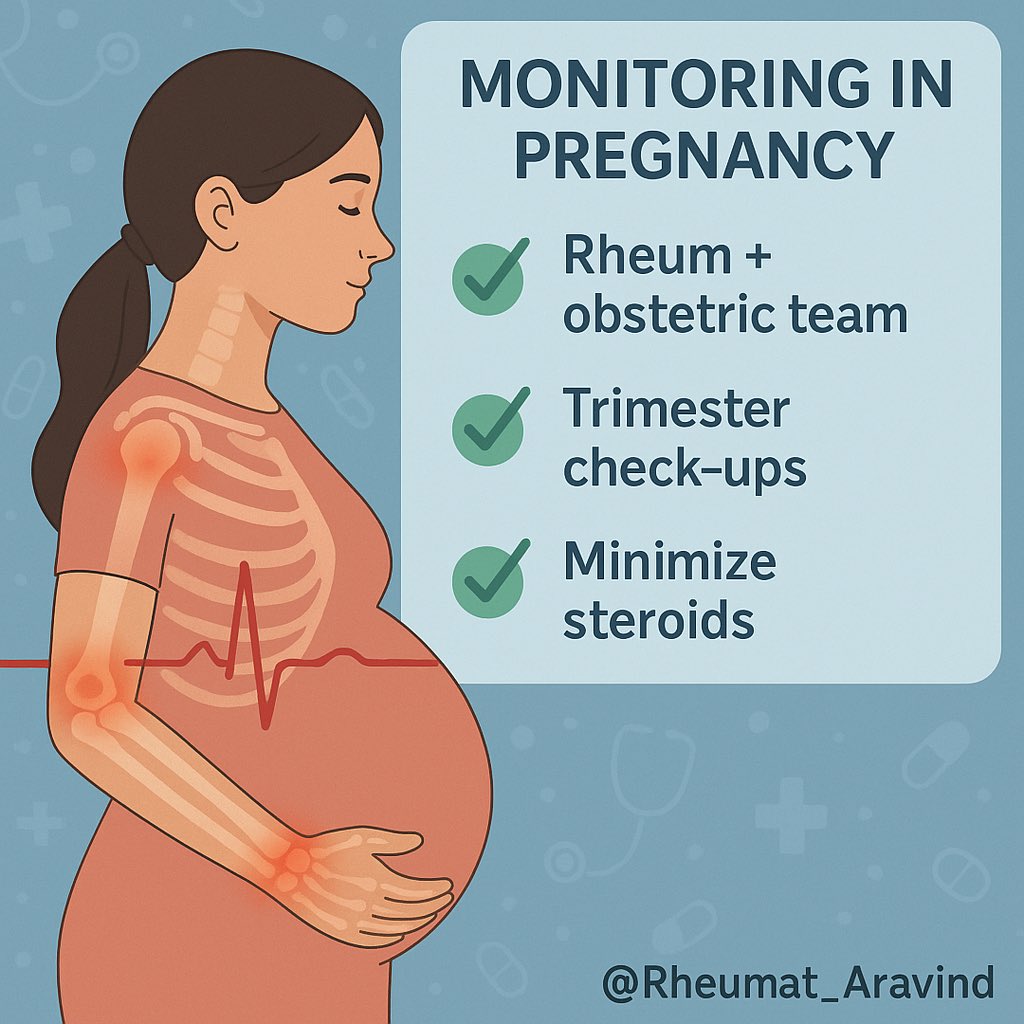
6️⃣ Monitoring in pregnancy
•Multidisciplinary approach: rheumatology + obstetrics
•Monitor disease activity every trimester
•Keep steroid dose as low as possible (ideally ≤7.5 mg prednisolone)
•Multidisciplinary approach: rheumatology + obstetrics
•Monitor disease activity every trimester
•Keep steroid dose as low as possible (ideally ≤7.5 mg prednisolone)
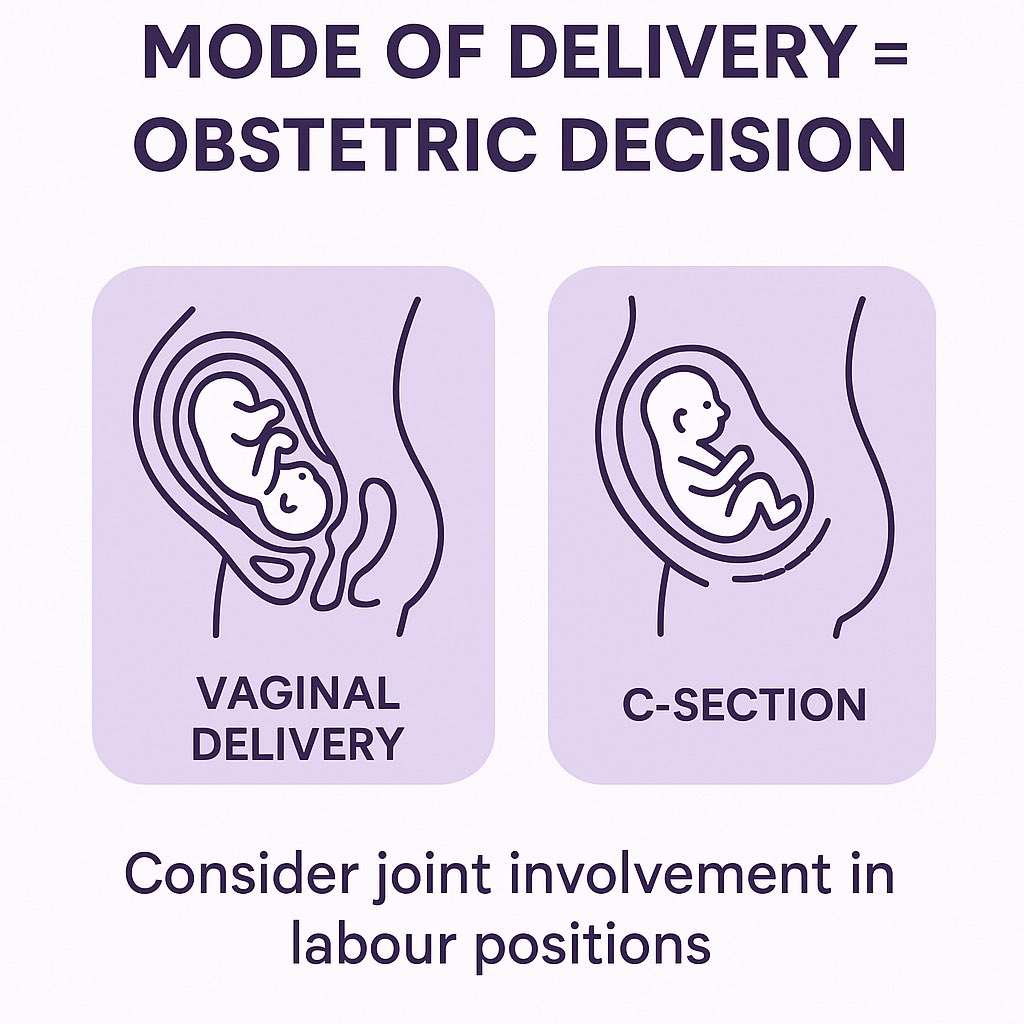
7️⃣ Delivery planning
RA itself isn’t an indication for C-section.
Mode of delivery depends on obstetric indications — but hand, wrist, or hip involvement may affect labour positions.
RA itself isn’t an indication for C-section.
Mode of delivery depends on obstetric indications — but hand, wrist, or hip involvement may affect labour positions.
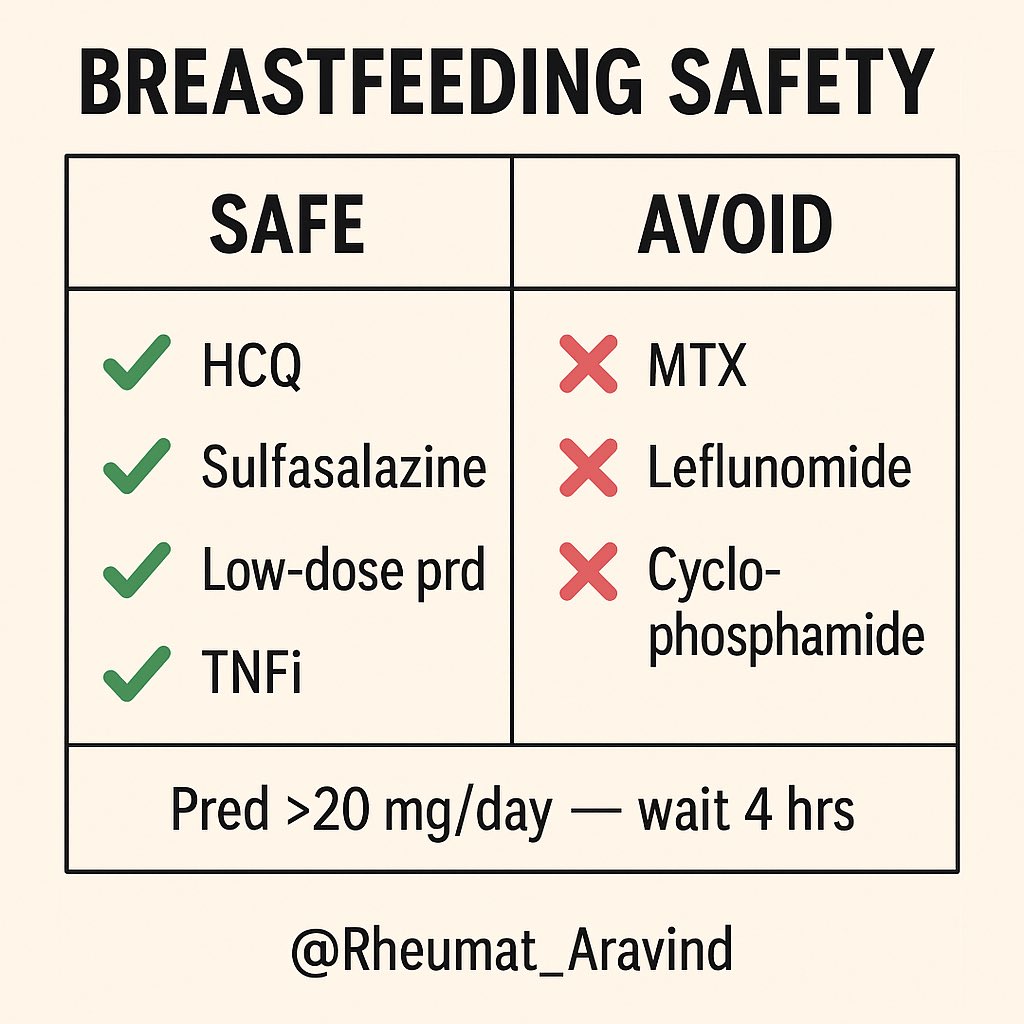
8️⃣ Breastfeeding — drug safety
Most RA-safe pregnancy drugs are also safe in breastfeeding:
✅ Hydroxychloroquine, sulfasalazine, low-dose prednisolone, most TNF inhibitors
❌ Methotrexate, leflunomide, cyclophosphamide — avoid
💡 Prednisolone >20 mg/day: wait 4 hrs after dose before feeding
Most RA-safe pregnancy drugs are also safe in breastfeeding:
✅ Hydroxychloroquine, sulfasalazine, low-dose prednisolone, most TNF inhibitors
❌ Methotrexate, leflunomide, cyclophosphamide — avoid
💡 Prednisolone >20 mg/day: wait 4 hrs after dose before feeding
9️⃣ Flares after delivery
Up to 40–50% of women flare postpartum.
Plan follow-up within the first 6 weeks to adjust meds promptly.
Up to 40–50% of women flare postpartum.
Plan follow-up within the first 6 weeks to adjust meds promptly.
🔟 Key take-home
•Plan early, aim for remission
•Choose pregnancy-safe meds
•Continue care into postpartum period
•RA control protects both mother & baby
💬 Have you managed RA in pregnancy in your practice?
What’s been your biggest challenge? Let’s discuss 👇
•Plan early, aim for remission
•Choose pregnancy-safe meds
•Continue care into postpartum period
•RA control protects both mother & baby
💬 Have you managed RA in pregnancy in your practice?
What’s been your biggest challenge? Let’s discuss 👇
• • •
Missing some Tweet in this thread? You can try to
force a refresh