🔬Interesting new study: Researchers exposed lab-grown human muscle tissues to blood serum from people with ME/CFS and Long COVID.
After 48 muscles:
- Produced less force
- Fatigued faster
- Lost their ability to hold peak strength
Let’s breakdown the full paper 🧵
After 48 muscles:
- Produced less force
- Fatigued faster
- Lost their ability to hold peak strength
Let’s breakdown the full paper 🧵

Cohort: 4 ME/CFS patients, 5 Long COVID patients, 4 healthy controls (all female).
Method: Researchers grew 3D muscle tissues from human cells, exposed them to patient serum for 48–144h, and tested strength, gene activity (using RNA-seq), structure, and metabolism.
Method: Researchers grew 3D muscle tissues from human cells, exposed them to patient serum for 48–144h, and tested strength, gene activity (using RNA-seq), structure, and metabolism.
Muscles treated with ME/CFS serum were generally weaker.
Muscles treated with Long COVID serum crashed sooner and couldn’t maintain strength after hitting their peak.
This early fatigue pattern supports what many patients report, myself included.
Muscles treated with Long COVID serum crashed sooner and couldn’t maintain strength after hitting their peak.
This early fatigue pattern supports what many patients report, myself included.
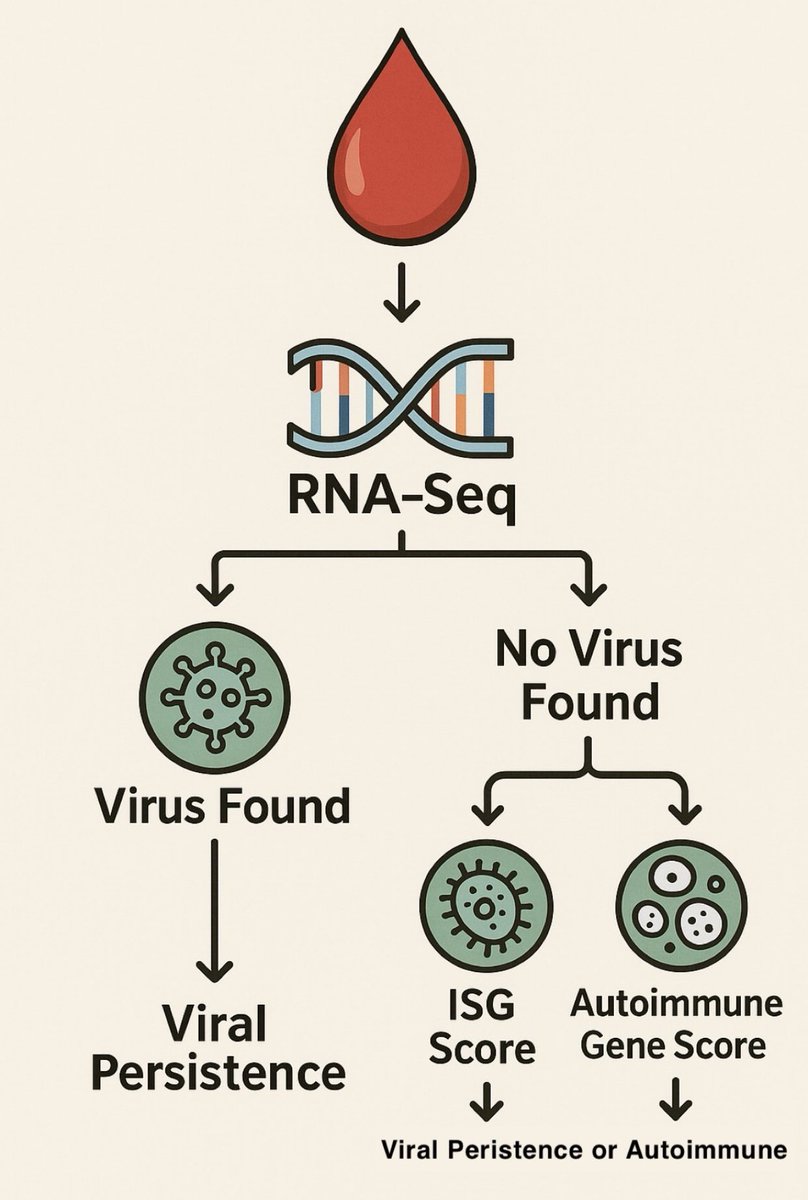
Researchers then looked at gene activity (transcriptomics), using RNA sequencing in the muscles to find out why this weakness happened.
Both ME/CFS and Long COVID changed hundreds of genes compared to healthy serum.
We are doing whole blood RNA sequencing at @amaticahealth
Both ME/CFS and Long COVID changed hundreds of genes compared to healthy serum.
We are doing whole blood RNA sequencing at @amaticahealth
Will be interesting to see if blood shows similar changes as muscles and how they also vary.
We will also be hoping to do muscle biopsy RNA sequencing in the future via grant funding and will take patients from our RNA whole blood cohort to have both sets of data.
We will also be hoping to do muscle biopsy RNA sequencing in the future via grant funding and will take patients from our RNA whole blood cohort to have both sets of data.
Video explainer on what RNA, RNA Sequencing & Gene expression is on our website:
amaticahealth.com/me-cfs-long-co…
amaticahealth.com/me-cfs-long-co…
ME/CFS serum increased activity of genes related to:
- Protein production
- Muscle structure
- Extracellular matrix (the “scaffolding” around cells)
But it reduced genes involved in energy production and general metabolism.
- Protein production
- Muscle structure
- Extracellular matrix (the “scaffolding” around cells)
But it reduced genes involved in energy production and general metabolism.
Long COVID serum also increased protein production genes, but showed stronger activation of:
- Mitochondrial structure
- Fatty acid metabolism
- Electron transport chain (for energy production)
It also reduced genes for normal cellular functions.
- Mitochondrial structure
- Fatty acid metabolism
- Electron transport chain (for energy production)
It also reduced genes for normal cellular functions.
This suggests:
- ME/CFS muscles prioritize structure, possibly trying to repair or reinforce themselves.
- Long COVID muscles activate energy systems more, possibly trying to fuel themselves under stress.
- ME/CFS muscles prioritize structure, possibly trying to repair or reinforce themselves.
- Long COVID muscles activate energy systems more, possibly trying to fuel themselves under stress.
A key energy-regulating gene, PDK4, went up in both conditions. It shifts energy use from glucose toward fats.
This is usually a stress response.
Glycolysis genes (like ENO3) also increased = more glucose breakdown for quick energy.
This is usually a stress response.
Glycolysis genes (like ENO3) also increased = more glucose breakdown for quick energy.
Calcium-handling genes were altered:
- More calcium was being pulled into storage inside the cell
- Less calcium was being pumped out
This imbalance can stress mitochondria and cause fatigue.
- More calcium was being pulled into storage inside the cell
- Less calcium was being pumped out
This imbalance can stress mitochondria and cause fatigue.
At the same time, antioxidant defenses were lower. A key enzyme called SOD2, which clears damaging molecules in mitochondria, went down.
That suggests more oxidative stress, which can further damage muscle.
That suggests more oxidative stress, which can further damage muscle.
Muscle growth-related genes like FHL1 were up.
This, along with larger muscle fiber diameter, shows the tissue was trying to compensate by growing or strengthening.
This was confirmed by microscope imaging.
This, along with larger muscle fiber diameter, shows the tissue was trying to compensate by growing or strengthening.
This was confirmed by microscope imaging.
The mitochondria (the cell’s energy producers) also changed.
Instead of their normal shape, they became highly fused and elongated, forming large networks.
This is a common stress response to increase energy efficiency.
Instead of their normal shape, they became highly fused and elongated, forming large networks.
This is a common stress response to increase energy efficiency.
Researchers measured real-time energy use in the cells.
Both ME/CFS and Long COVID muscles consumed more oxygen than controls.
But ME/CFS muscles had the highest energy use of all.
Both ME/CFS and Long COVID muscles consumed more oxygen than controls.
But ME/CFS muscles had the highest energy use of all.
In ME/CFS tissues:
- Baseline oxygen consumption was highest
- Proton leak (wasted oxygen use) was highest
- Glycolysis (non-oxygen energy pathway) also increased
This shows heavy energy strain.
- Baseline oxygen consumption was highest
- Proton leak (wasted oxygen use) was highest
- Glycolysis (non-oxygen energy pathway) also increased
This shows heavy energy strain.
In Long COVID tissues:
- Some energy markers went up
- But more oxygen was used by non-mitochondrial processes (likely inflammation or oxidative stress)
This means the mitochondria were less involved in energy production.
- Some energy markers went up
- But more oxygen was used by non-mitochondrial processes (likely inflammation or oxidative stress)
This means the mitochondria were less involved in energy production.
In short:
ME/CFS muscles pushed all systems harder (both mitochondrial and glycolytic)
Long COVID muscles tried to adapt, but energy use was less efficient.
Possibly due to Long COVID being earlier into the process?
ME/CFS muscles pushed all systems harder (both mitochondrial and glycolytic)
Long COVID muscles tried to adapt, but energy use was less efficient.
Possibly due to Long COVID being earlier into the process?
What happens if exposure to patient serum continues?
Researchers ran long-term tests (up to 144 hours).
The muscles began to fail.
Researchers ran long-term tests (up to 144 hours).
The muscles began to fail.
By day 4-6:
- Muscle tissues got thinner
- Mitochondria broke apart into small, dysfunctional fragments
- Some mitochondria turned into ring shapes, a sign of severe damage
- Force production collapsed
- Muscle tissues got thinner
- Mitochondria broke apart into small, dysfunctional fragments
- Some mitochondria turned into ring shapes, a sign of severe damage
- Force production collapsed
This shows the muscles entered a second phase:
From early adaptation (trying to compensate) to collapse (losing structure and function).
This mirrors what happens in patients with long-term fatigue and muscle issues.
From early adaptation (trying to compensate) to collapse (losing structure and function).
This mirrors what happens in patients with long-term fatigue and muscle issues.
Key takeaway:
The blood of ME/CFS and Long COVID patients contains factors that directly damage muscle, even without any exercise.
This damage is not due to inactivity. It is driven by circulating biological signals.
The blood of ME/CFS and Long COVID patients contains factors that directly damage muscle, even without any exercise.
This damage is not due to inactivity. It is driven by circulating biological signals.
These findings support patient reports of:
- Muscle weakness
- Exertion intolerance
- Fatigue after light activity
- Long-term muscle loss
All of this was reproduced in a controlled lab model.
- Muscle weakness
- Exertion intolerance
- Fatigue after light activity
- Long-term muscle loss
All of this was reproduced in a controlled lab model.
While both ME/CFS and Long COVID had similar effects, there were differences:
- ME/CFS caused more metabolic overdrive
- Long COVID had more uncoupled, inefficient energy use
- ME/CFS showed more structural remodeling
- ME/CFS caused more metabolic overdrive
- Long COVID had more uncoupled, inefficient energy use
- ME/CFS showed more structural remodeling
We will be measuring all genes mentioned above in whole blood, very interested to see the findings in patients with muscle weakness like myself. To join:
amaticahealth.com/me-cfs-long-co…
The full paper:
iopscience.iop.org/article/10.108…
amaticahealth.com/me-cfs-long-co…
The full paper:
iopscience.iop.org/article/10.108…
• • •
Missing some Tweet in this thread? You can try to
force a refresh