💡 “When Joint Pain Is NOT Arthritis” — The 7 Red Flags Every Doctor Should Know
Tweet 1:
“Not every swollen or painful joint is arthritis. Missing the real cause can delay life-saving treatment.
Here are 7 red flags that should make you think beyond rheumatology 👇”
@IhabFathiSulima @DrAkhilX @CelestinoGutirr @SarahSchaferMD @NeuroSjogrens #MedTwitter
Tweet 1:
“Not every swollen or painful joint is arthritis. Missing the real cause can delay life-saving treatment.
Here are 7 red flags that should make you think beyond rheumatology 👇”
@IhabFathiSulima @DrAkhilX @CelestinoGutirr @SarahSchaferMD @NeuroSjogrens #MedTwitter
Tweet 2:
1️⃣ Fever + Acute Monoarthritis
•Think septic arthritis until proven otherwise
•Don’t start steroids until infection is ruled out
1️⃣ Fever + Acute Monoarthritis
•Think septic arthritis until proven otherwise
•Don’t start steroids until infection is ruled out
Tweet 3:
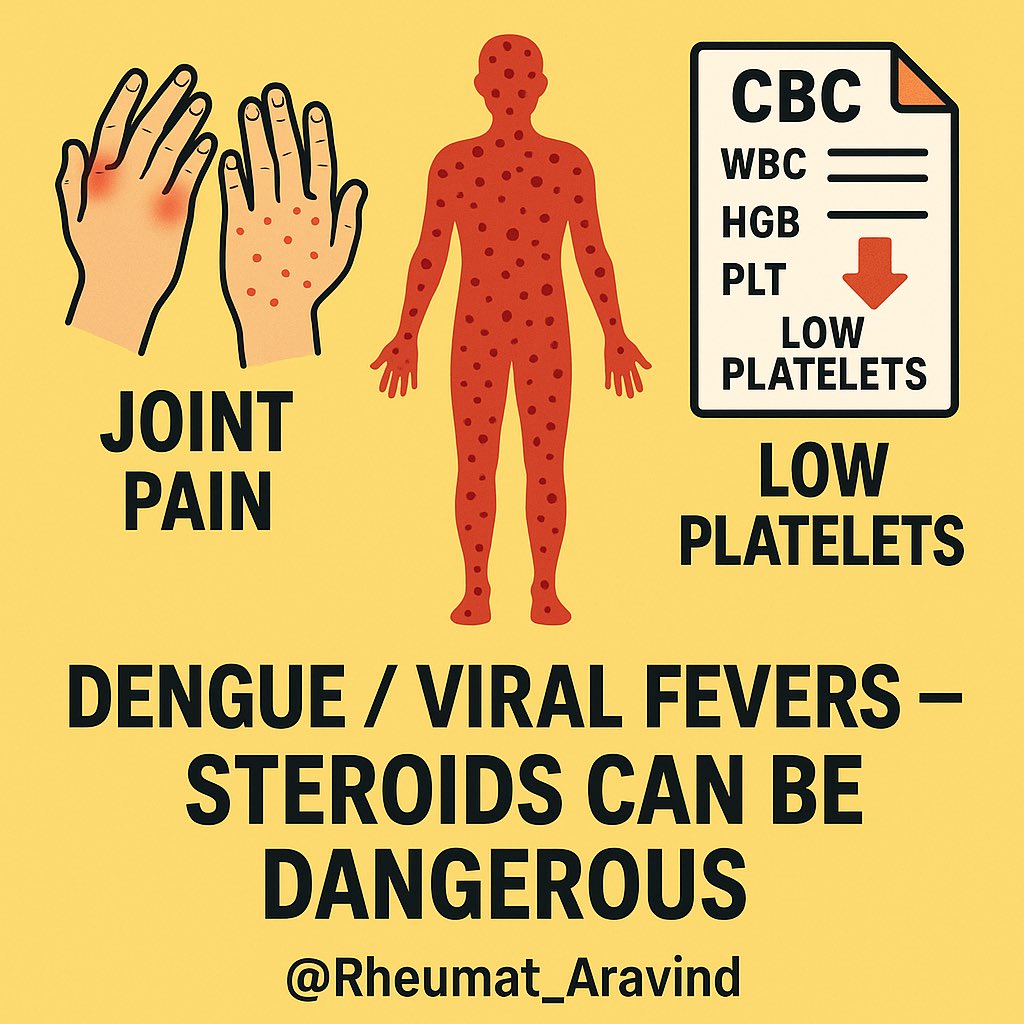
2️⃣ Joint Pain + Rash + Low Platelets
•Could be dengue or other viral fevers
•ESR/CRP may be high but steroids can be dangerous
2️⃣ Joint Pain + Rash + Low Platelets
•Could be dengue or other viral fevers
•ESR/CRP may be high but steroids can be dangerous
Tweet 4:
3️⃣ Back Pain + Weight Loss + Night Sweats
•Rule out spinal TB, lymphoma, metastatic cancer
•Don’t rush to label as spondyloarthritis
3️⃣ Back Pain + Weight Loss + Night Sweats
•Rule out spinal TB, lymphoma, metastatic cancer
•Don’t rush to label as spondyloarthritis
Tweet 5:
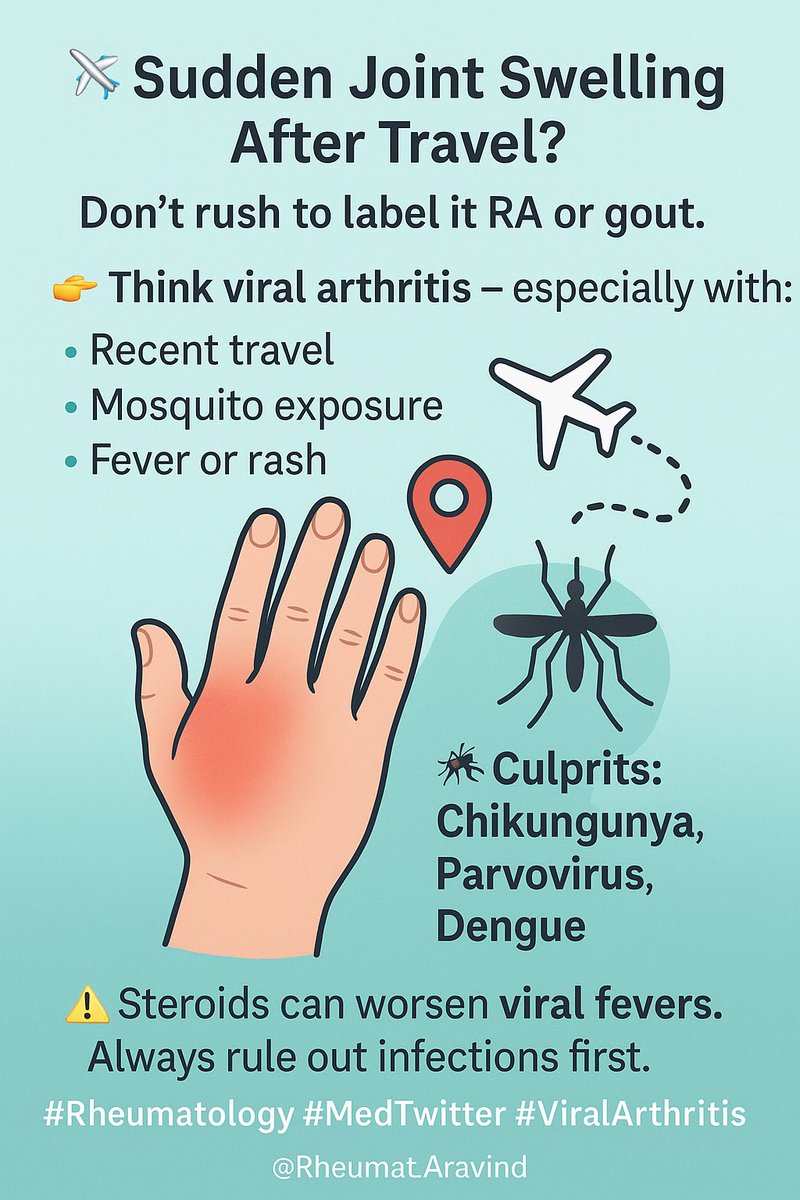
4️⃣ Sudden Swelling + Travel History
•Think viral arthritis (Chikungunya, Parvovirus)
•Usually self-limiting, but steroids may prolong symptoms
4️⃣ Sudden Swelling + Travel History
•Think viral arthritis (Chikungunya, Parvovirus)
•Usually self-limiting, but steroids may prolong symptoms
Tweet 6:
5️⃣ Polyarthritis + New Heart Murmur
•Consider infective endocarditis
•Early antibiotics can save lives
5️⃣ Polyarthritis + New Heart Murmur
•Consider infective endocarditis
•Early antibiotics can save lives
Tweet 7:
6️⃣ Joint Pain + Neurological Symptoms
•Could be multiple sclerosis, stroke, vasculitis
•Don’t miss CNS involvement
6️⃣ Joint Pain + Neurological Symptoms
•Could be multiple sclerosis, stroke, vasculitis
•Don’t miss CNS involvement
Tweet 8:
7️⃣ Bone Pain + Swelling Without Inflammation Markers
•Think primary bone tumor or metastasis
•X-ray can be diagnostic
7️⃣ Bone Pain + Swelling Without Inflammation Markers
•Think primary bone tumor or metastasis
•X-ray can be diagnostic

Tweet 9:
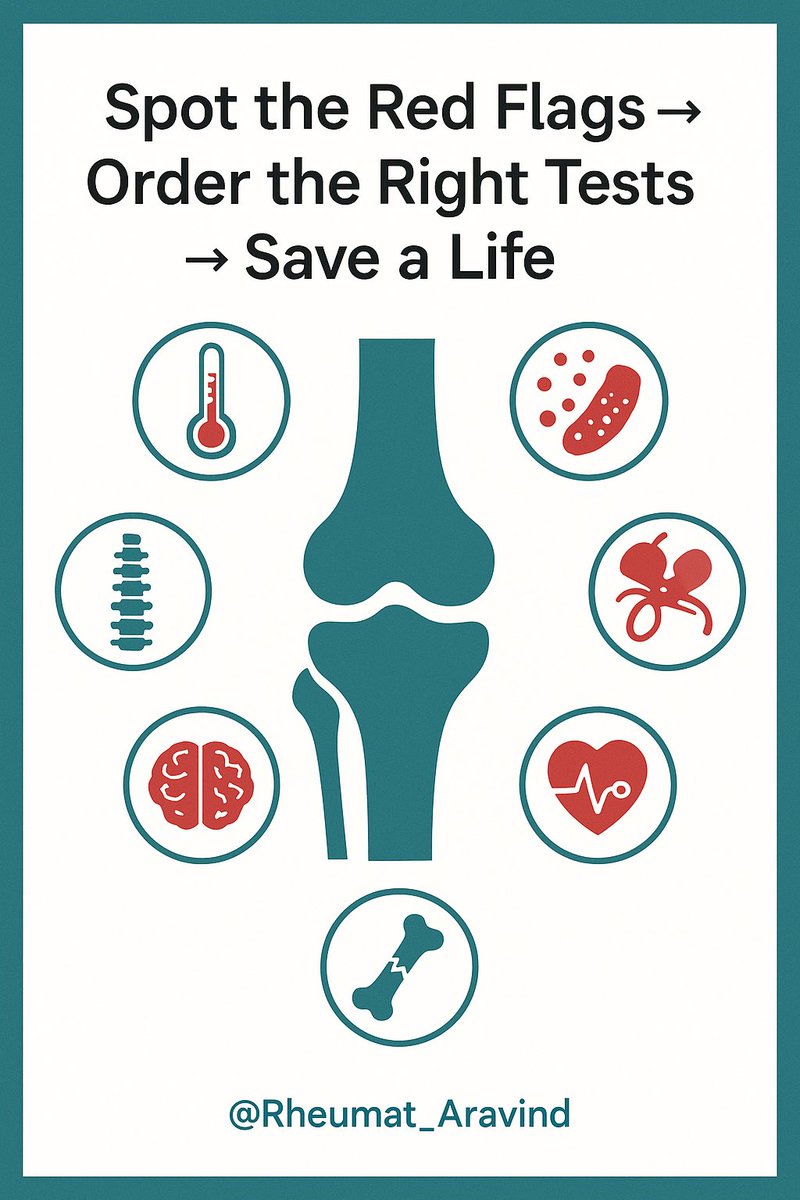
Joint pain is common. Arthritis is just one possibility.
Spot the red flags → order the right tests → save a life.
Share this so more doctors think beyond arthritis.
#MedTwitter #Rheumatology #MedEd
Joint pain is common. Arthritis is just one possibility.
Spot the red flags → order the right tests → save a life.
Share this so more doctors think beyond arthritis.
#MedTwitter #Rheumatology #MedEd
• • •
Missing some Tweet in this thread? You can try to
force a refresh