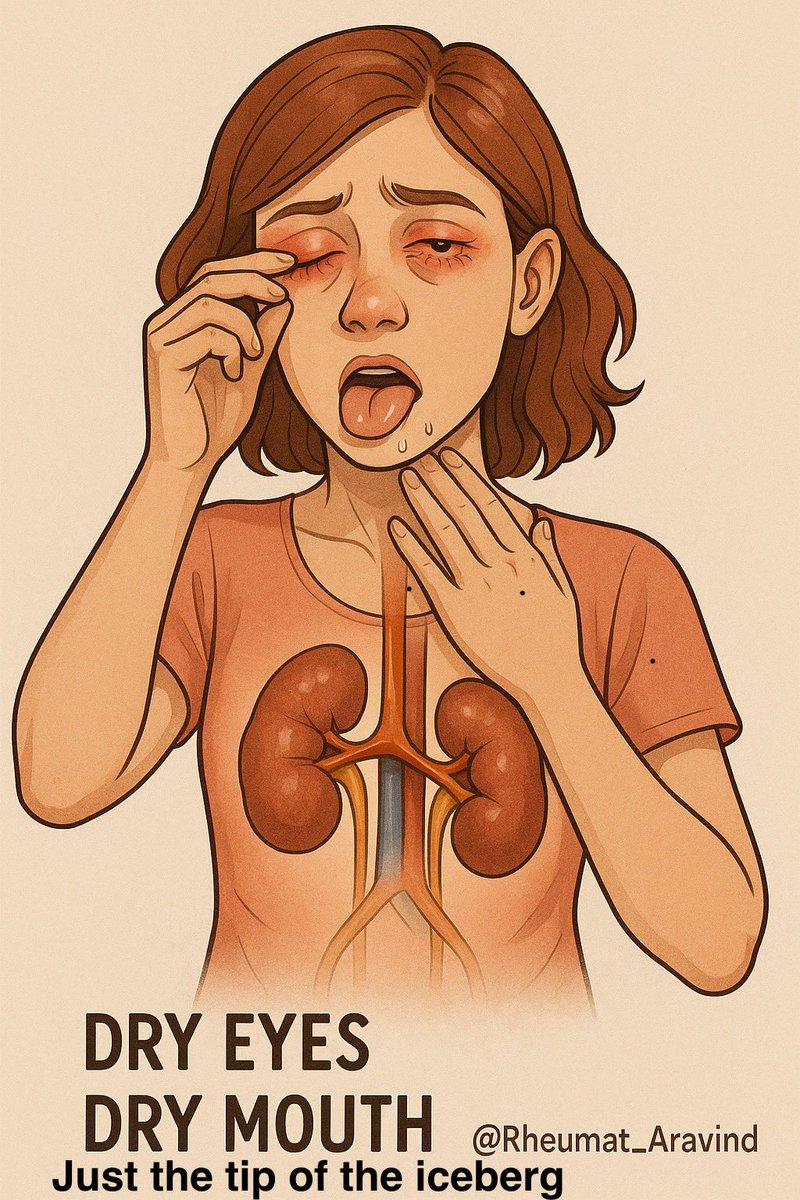
1/ 🧵 Most people think Sjögren’s disease means dry eyes and mouth—but did you know it can also affect your kidneys? Kidney problems in Sjögren’s are serious but often missed. Here’s everything you need to know. 👇
@IhabFathiSulima @DrAkhilX @CelestinoGutirr @JasmineNephro @arvindcanchi @SarahSchaferMD @NeuroSjogrens @elisa_comer @SjogrensIrl @SjogrensForum @SjogrensOrg @SjogrensCa #MedTwitter #Rheumatology
@IhabFathiSulima @DrAkhilX @CelestinoGutirr @JasmineNephro @arvindcanchi @SarahSchaferMD @NeuroSjogrens @elisa_comer @SjogrensIrl @SjogrensForum @SjogrensOrg @SjogrensCa #MedTwitter #Rheumatology
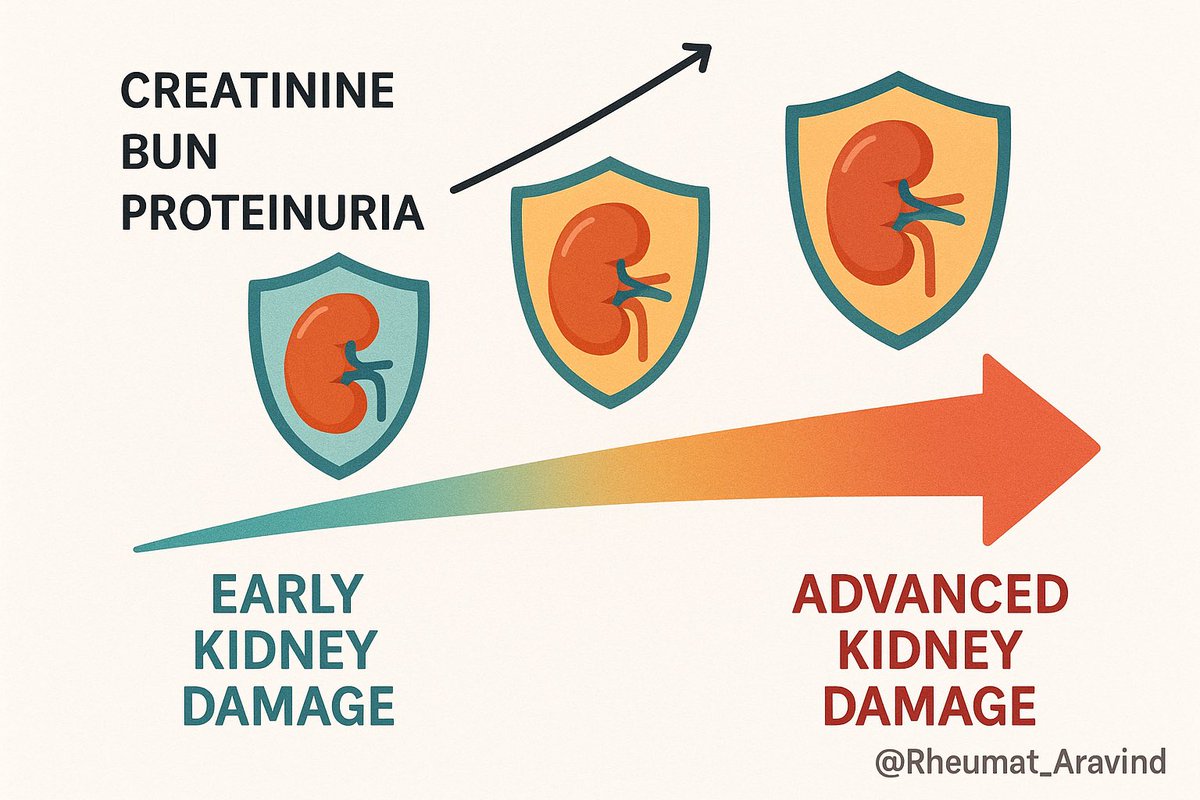
2/ Renal involvement in Sjögren’s can take many forms, from mild lab abnormalities to full-blown kidney disease. Early detection is key to prevent lasting damage. 
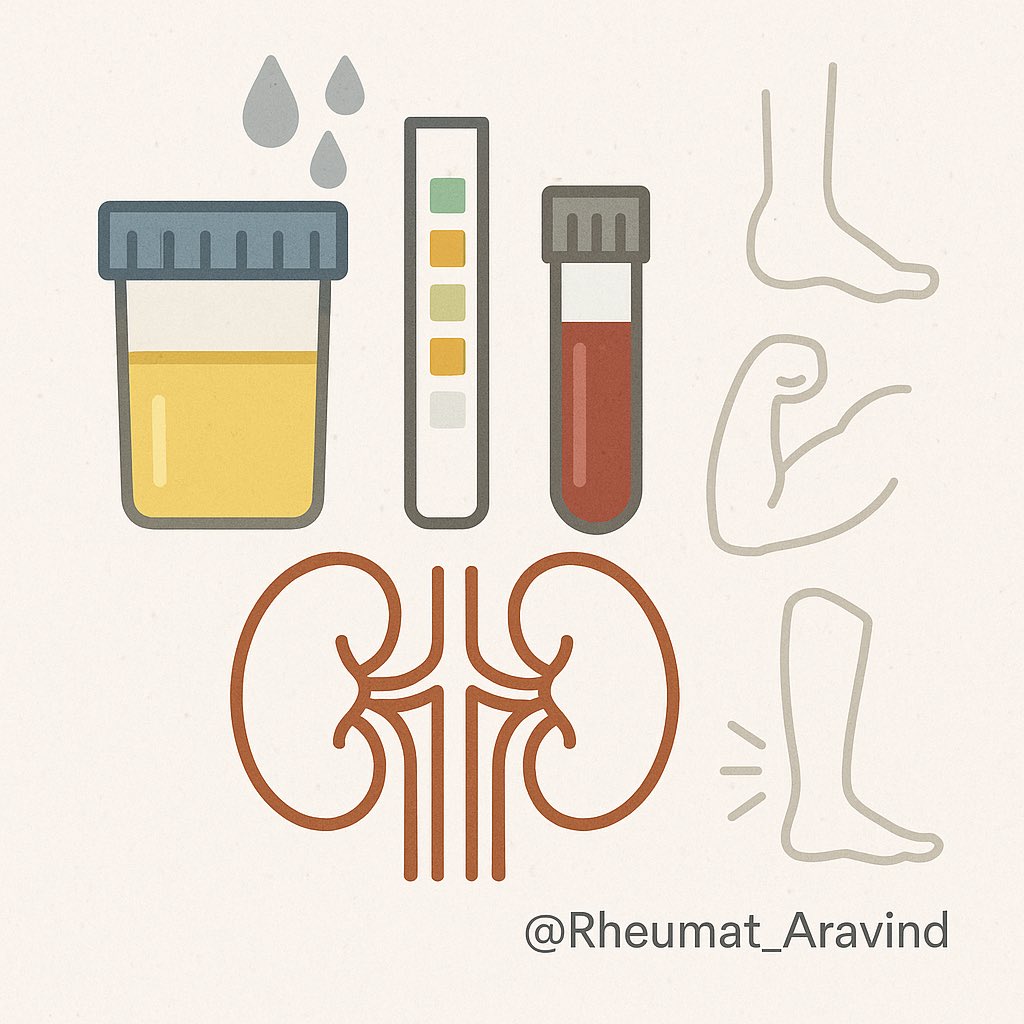
3/ Common kidney-related symptoms and signs include:
•Excess protein or blood in urine
•Excessive thirst and urination
•Muscle weakness due to low potassium
•Fatigue and swelling
•Sometimes no symptoms, only abnormal lab tests
•Excess protein or blood in urine
•Excessive thirst and urination
•Muscle weakness due to low potassium
•Fatigue and swelling
•Sometimes no symptoms, only abnormal lab tests
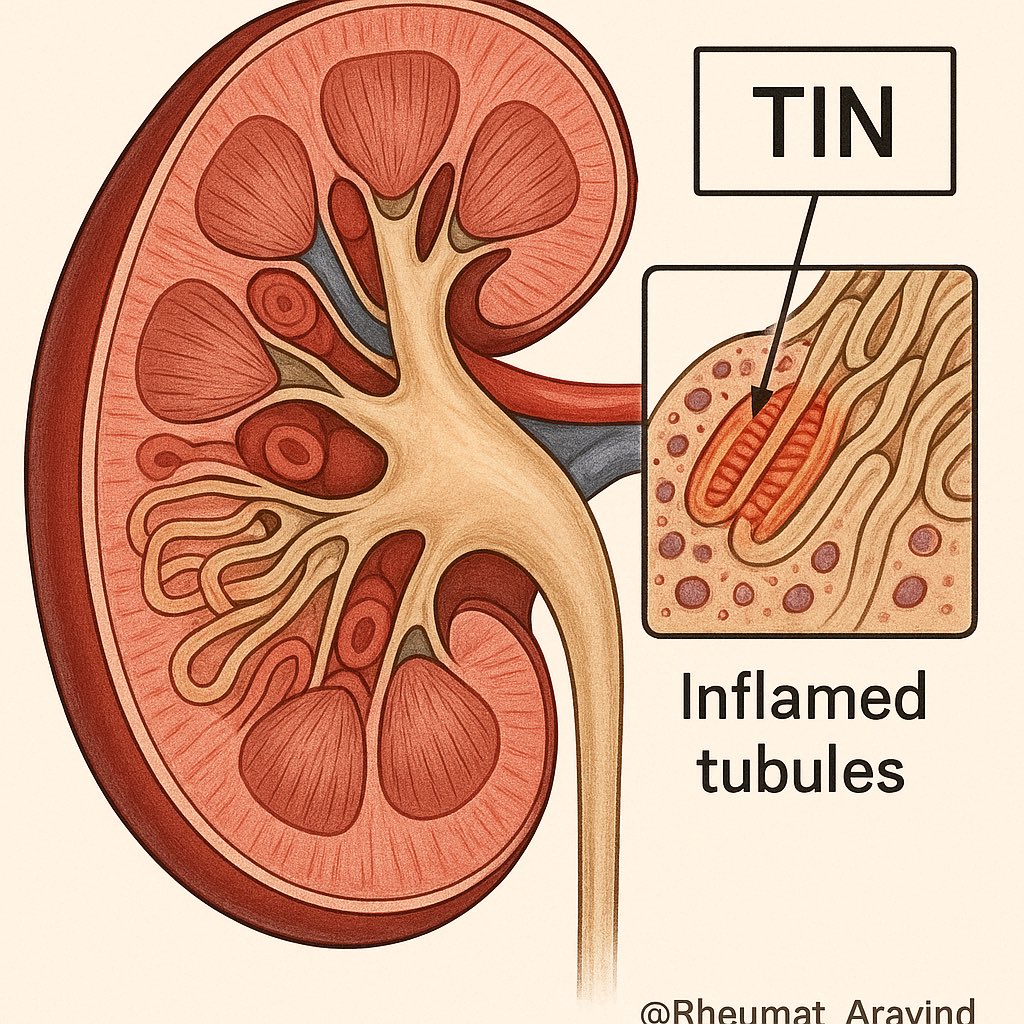
4/ The most frequent kidney problem in Sjögren’s is tubulointerstitial nephritis (TIN)—inflammation and scarring around tiny kidney tubes—leading to impaired kidney function. 
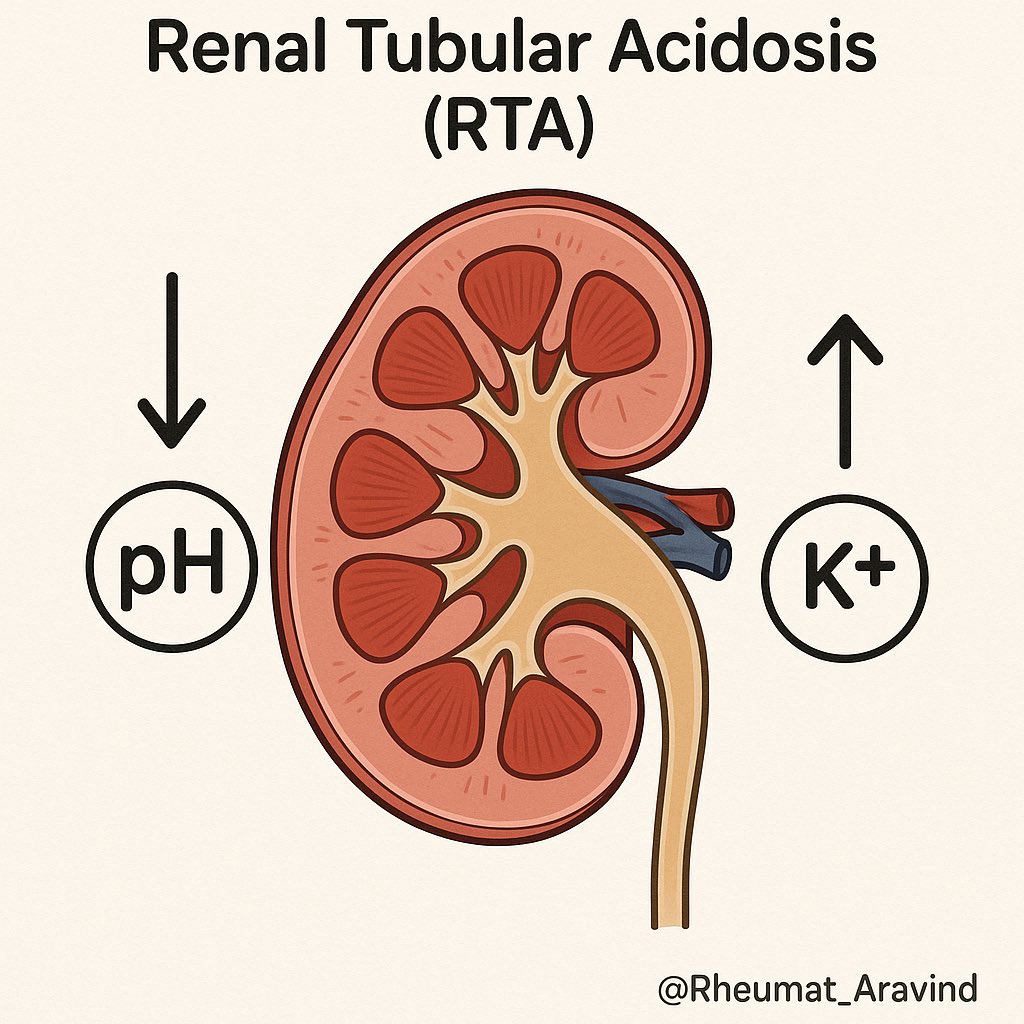
5/ Many patients also develop renal tubular acidosis (RTA), where kidneys fail to maintain acid-base balance, causing low potassium and other metabolic problems. 
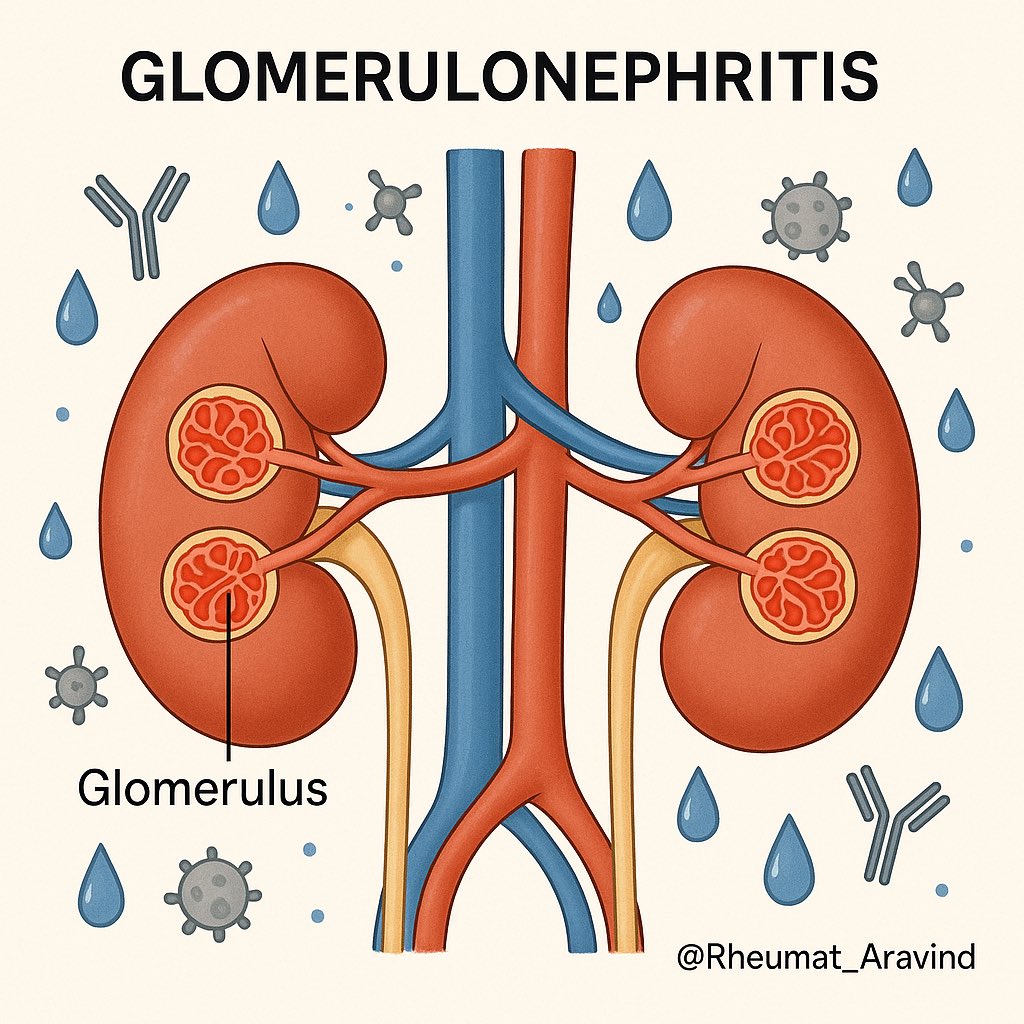
6/ Less commonly, Sjögren’s affects the glomeruli (kidney filters), causing various types of glomerulonephritis—sometimes linked to immune complexes or cryoglobulinemia. 
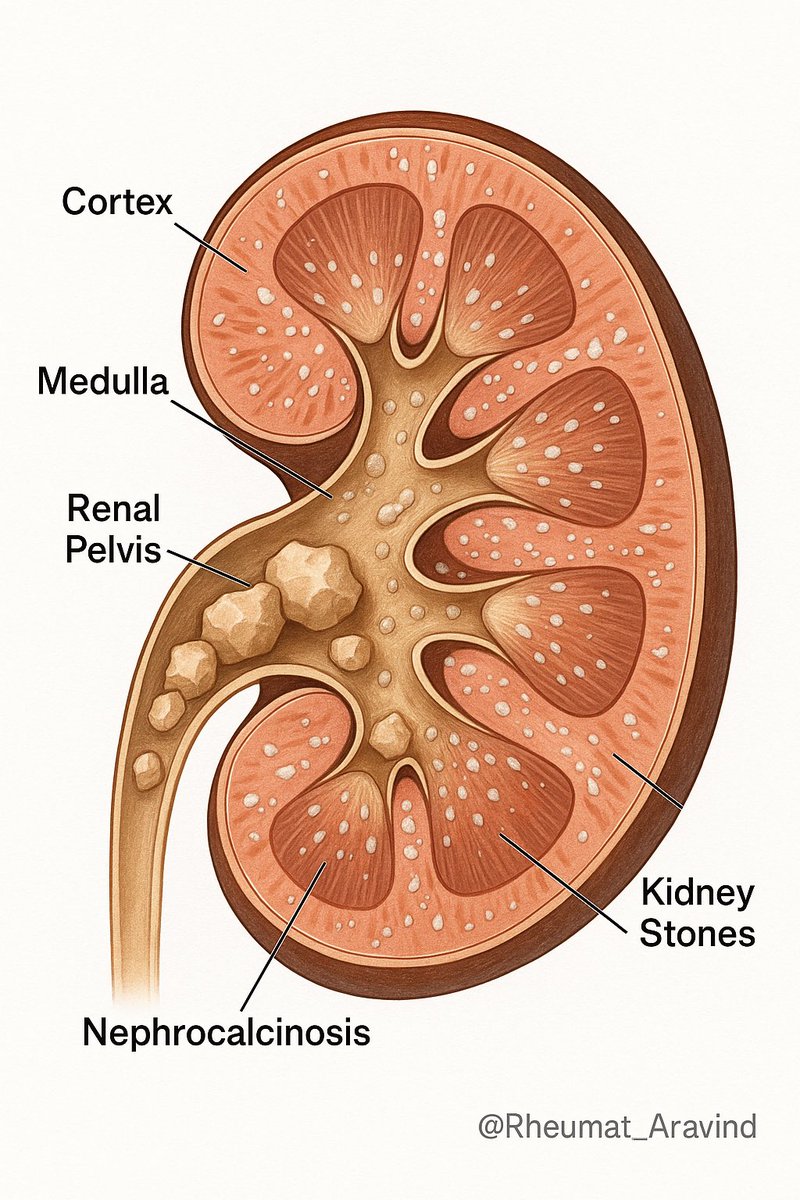
7/ Kidney stones and nephrocalcinosis (calcium deposits in kidneys) are also reported in Sjögren’s patients. 
8/ Renal disease may appear before classic dry eye/mouth symptoms, so screening is essential even for newly diagnosed patients. 
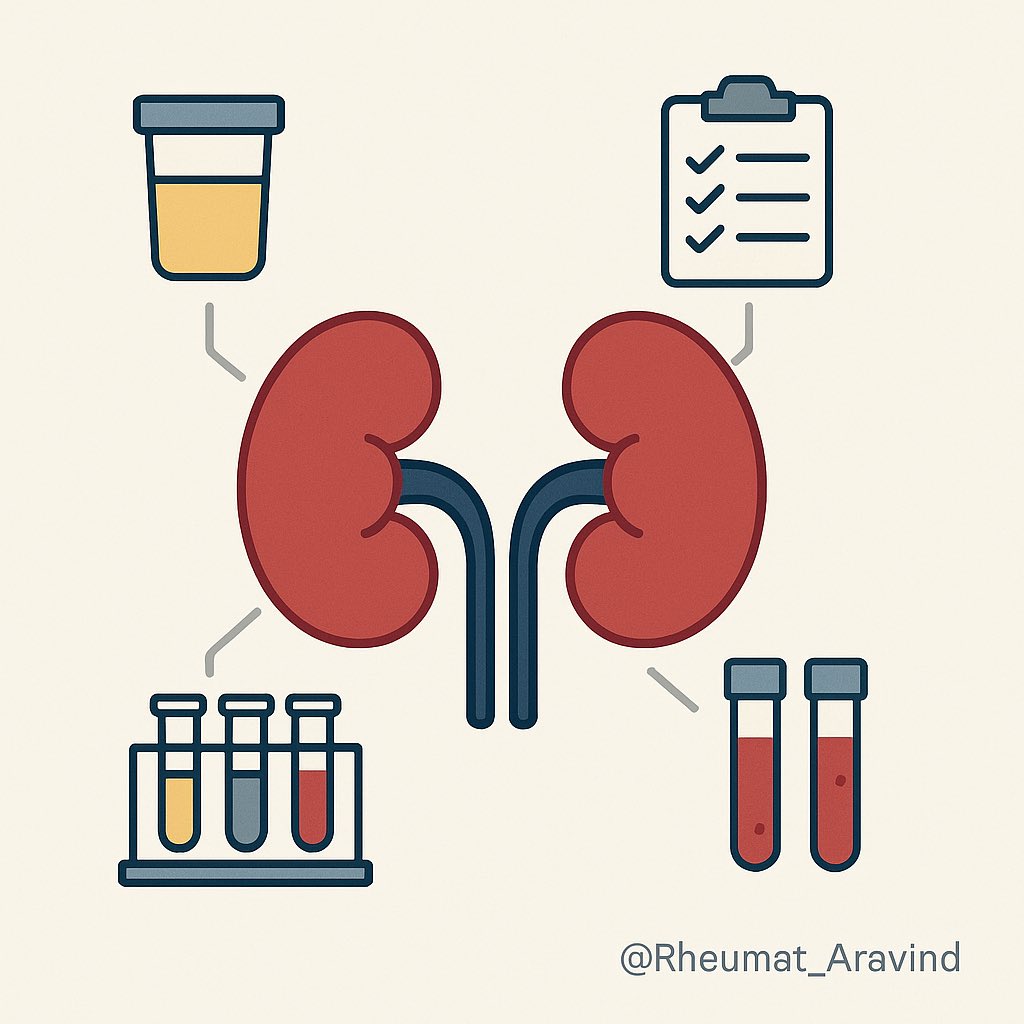
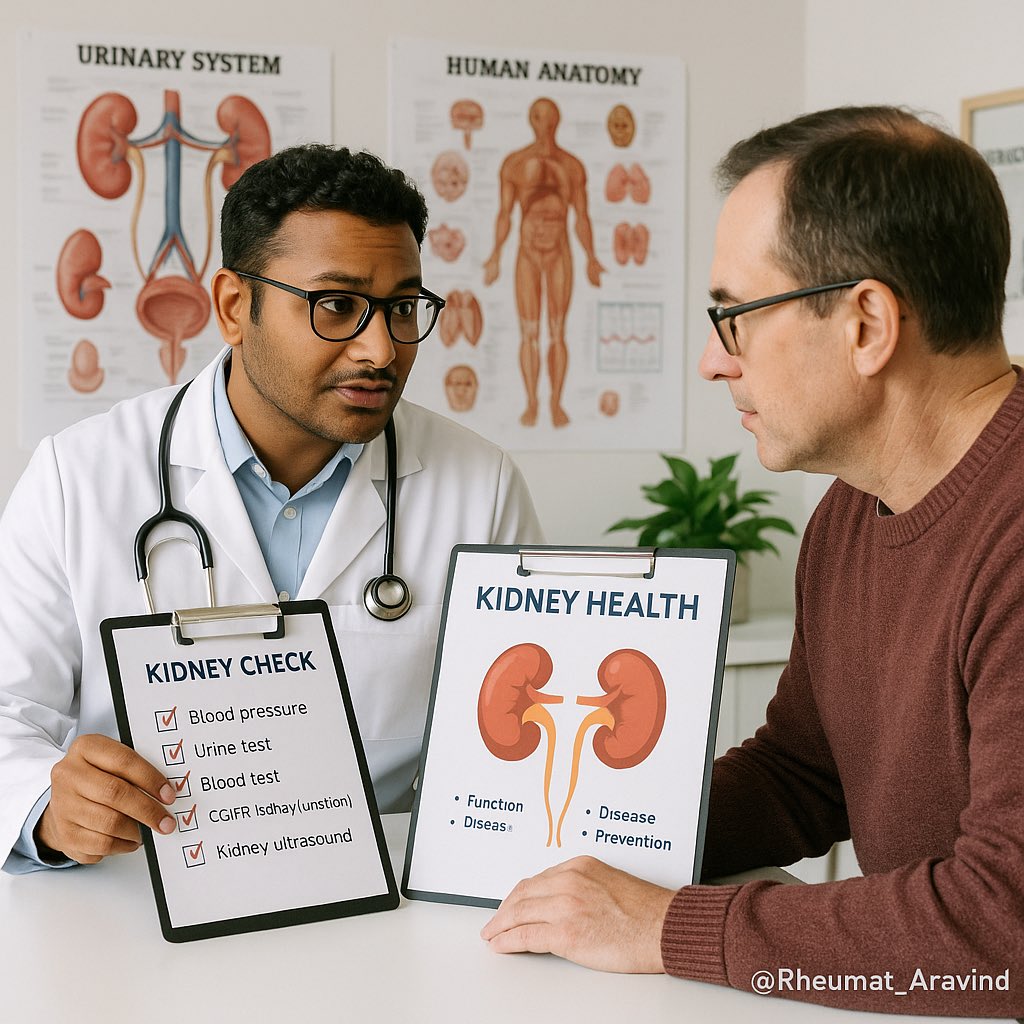
9/ To catch kidney involvement early, doctors should monitor:
•Urinalysis (for protein, blood)
•Kidney function tests (eGFR, creatinine)
•Electrolytes (especially potassium, bicarbonate)
•Urinalysis (for protein, blood)
•Kidney function tests (eGFR, creatinine)
•Electrolytes (especially potassium, bicarbonate)
10/ Treatment typically involves immunosuppressants (like steroids), potassium and bicarbonate supplements for RTA, and close follow-up to protect kidney health. 
11/ If you or someone you know has Sjögren’s—not only watch for dryness but also ask your doctor about kidney screening. Silent kidney damage is more common than you think!
Raising awareness can save lives. Please share this thread to help others understand the full impact of Sjögren’s disease. #Sjogrens #KidneyHealth #AutoimmuneDisease
Raising awareness can save lives. Please share this thread to help others understand the full impact of Sjögren’s disease. #Sjogrens #KidneyHealth #AutoimmuneDisease
• • •
Missing some Tweet in this thread? You can try to
force a refresh