🧵 2025 AHA Hypertension Guidelines: Changes & New Updates
1/ The 2025 AHA/ACC hypertension guideline replaces the 2017 version with key, evidence-driven changes. Here are the must-know updates for your clinical practice.
@IhabFathiSulima @DrAkhilX @TrackYourHeart @sumersethi @Mahmoud33986639 @latchumanadhas #MedTwitter
1/ The 2025 AHA/ACC hypertension guideline replaces the 2017 version with key, evidence-driven changes. Here are the must-know updates for your clinical practice.
@IhabFathiSulima @DrAkhilX @TrackYourHeart @sumersethi @Mahmoud33986639 @latchumanadhas #MedTwitter
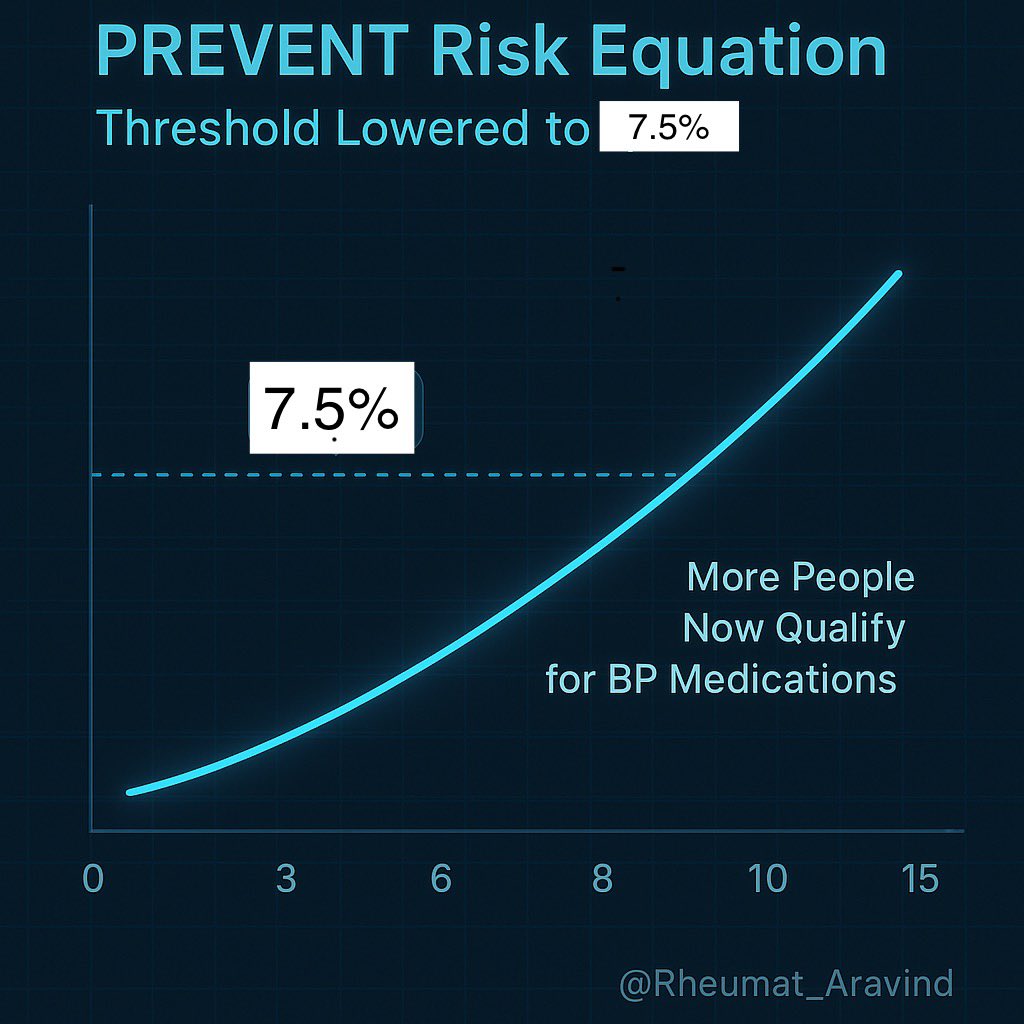
2/ PREVENT Risk Equation Now Central
All therapy decisions now use the PREVENT risk score (not pooled cohort equations). The 10-year CVD risk threshold to start medication is now ≥7.5%—so more patients, especially with moderate risk, will get earlier treatment.
All therapy decisions now use the PREVENT risk score (not pooled cohort equations). The 10-year CVD risk threshold to start medication is now ≥7.5%—so more patients, especially with moderate risk, will get earlier treatment.
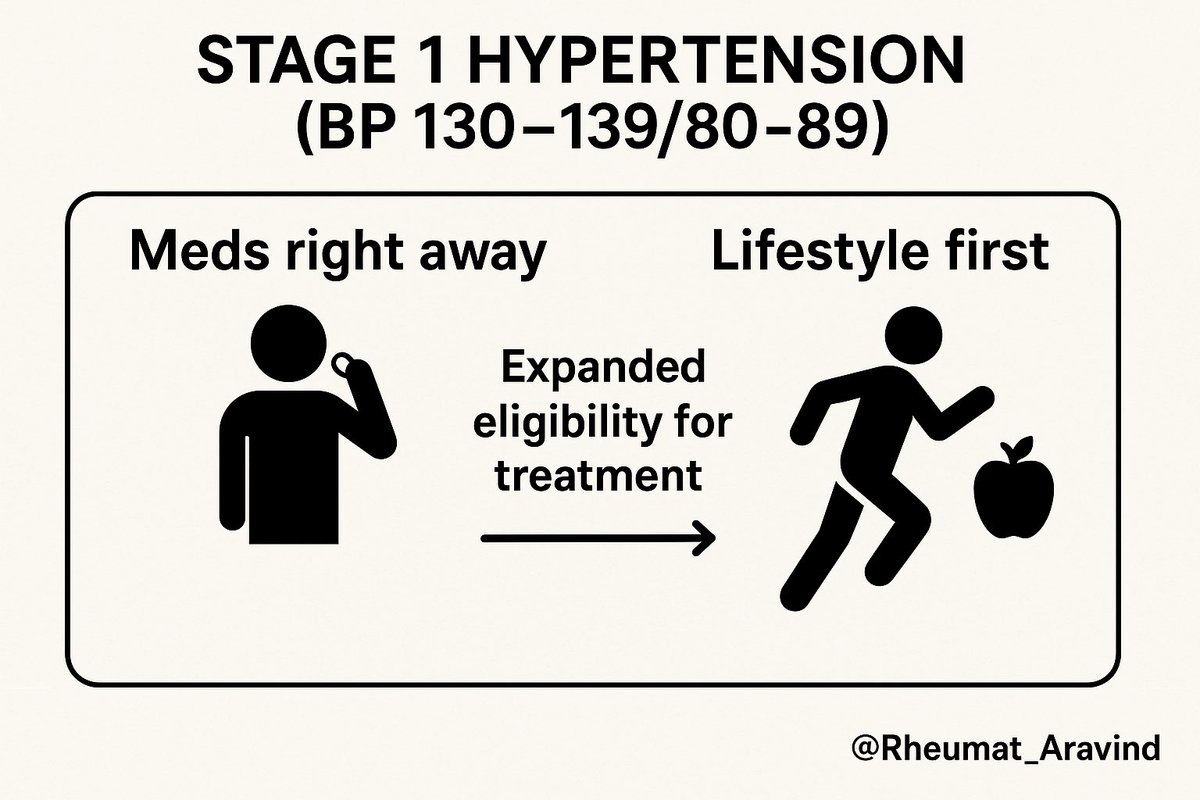
3/ Initiation of Therapy at Lower Thresholds
Stage 1 hypertension (130–139/80–89 mm Hg):
•If CVD, CKD, diabetes, or PREVENT risk ≥7.5%, start antihypertensive immediately.
•If PREVENT risk <7.5%: start with lifestyle changes for 3–6 months. If BP stays ≥130/80, add medication.
This expands eligibility —more aggressive than 2017.
Stage 1 hypertension (130–139/80–89 mm Hg):
•If CVD, CKD, diabetes, or PREVENT risk ≥7.5%, start antihypertensive immediately.
•If PREVENT risk <7.5%: start with lifestyle changes for 3–6 months. If BP stays ≥130/80, add medication.
This expands eligibility —more aggressive than 2017.
4/ Single-Pill Combinations as First-Line Therapy
Most patients are now encouraged to start with 2-drug, single-pill combo antihypertensives to boost adherence and BP control.
Most patients are now encouraged to start with 2-drug, single-pill combo antihypertensives to boost adherence and BP control.
5/ Emphasis on Early Intervention
Early therapy is stressed to lower risks of heart failure, CKD, stroke, and especially cognitive decline/vascular dementia—now a stronger focus.
Early therapy is stressed to lower risks of heart failure, CKD, stroke, and especially cognitive decline/vascular dementia—now a stronger focus.
6/ Lifestyle & Alcohol: Stronger Recommendations
•Even more emphasis on dietary salt cut, physical activity, healthy weight, and stress reduction.
•New, explicit advice to avoid or strongly limit alcohol as BP-lowering strategy; alcohol is now a “risk enhancer.”
•Even more emphasis on dietary salt cut, physical activity, healthy weight, and stress reduction.
•New, explicit advice to avoid or strongly limit alcohol as BP-lowering strategy; alcohol is now a “risk enhancer.”

7/ BP Measurement Modernization
•All major decisions should be based on validated, out-of-office BP measurements (home or ambulatory monitoring).
•Recommend periodic revalidation of home devices and proper technique for all readings.
•All major decisions should be based on validated, out-of-office BP measurements (home or ambulatory monitoring).
•Recommend periodic revalidation of home devices and proper technique for all readings.

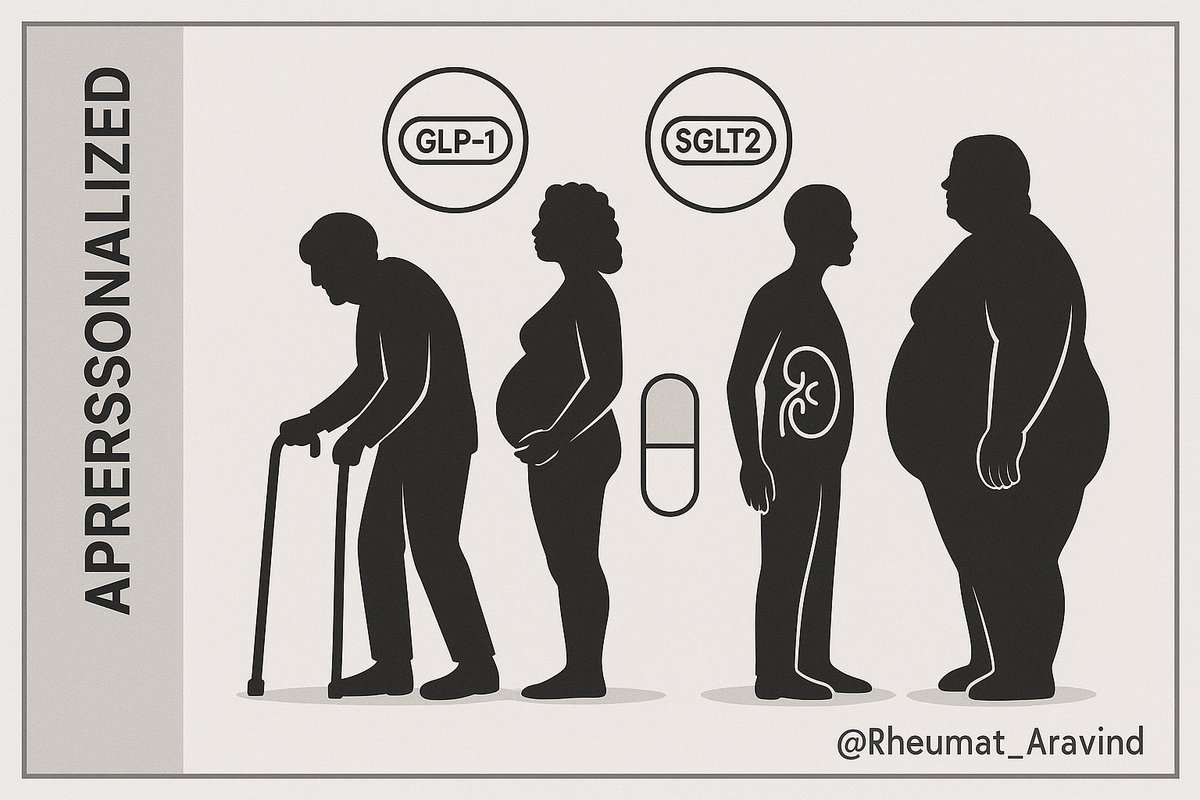
8/ Tailored Approaches for Special Groups
Guidelines offer specific recommendations for:
•CKD, diabetes, pregnancy, elderly, resistant HTN
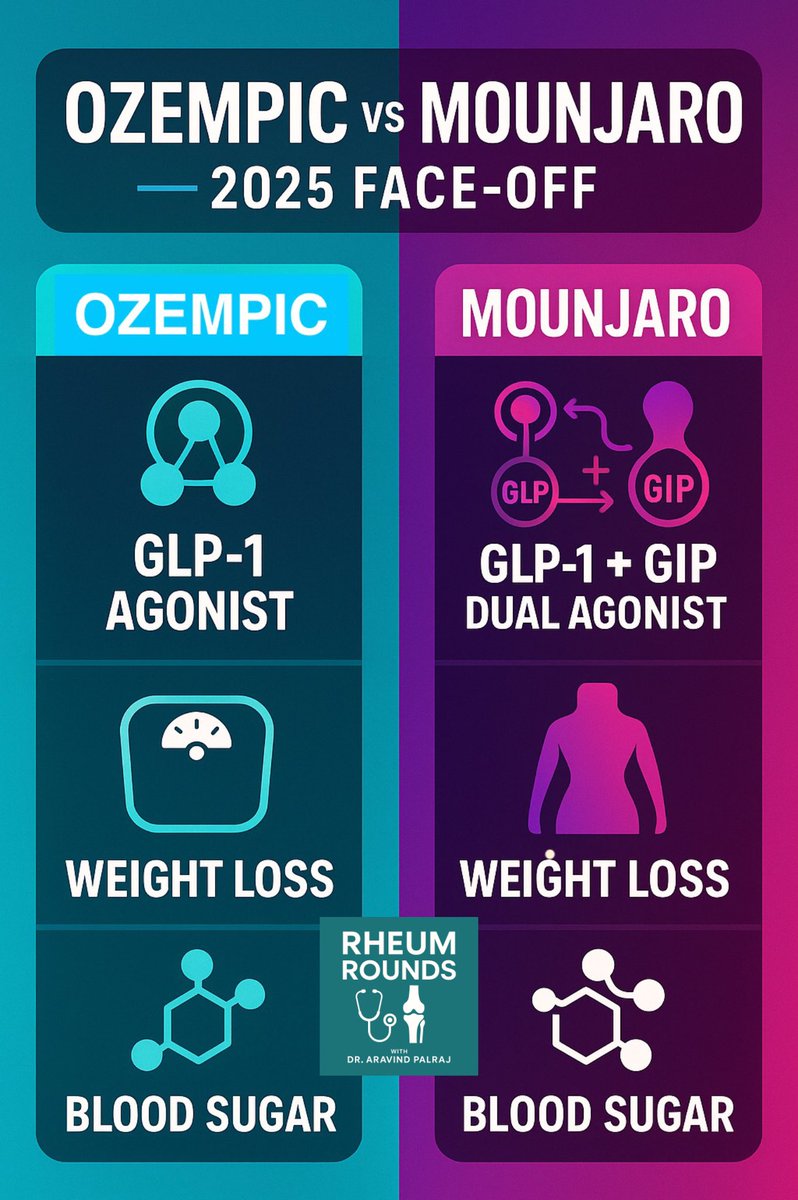
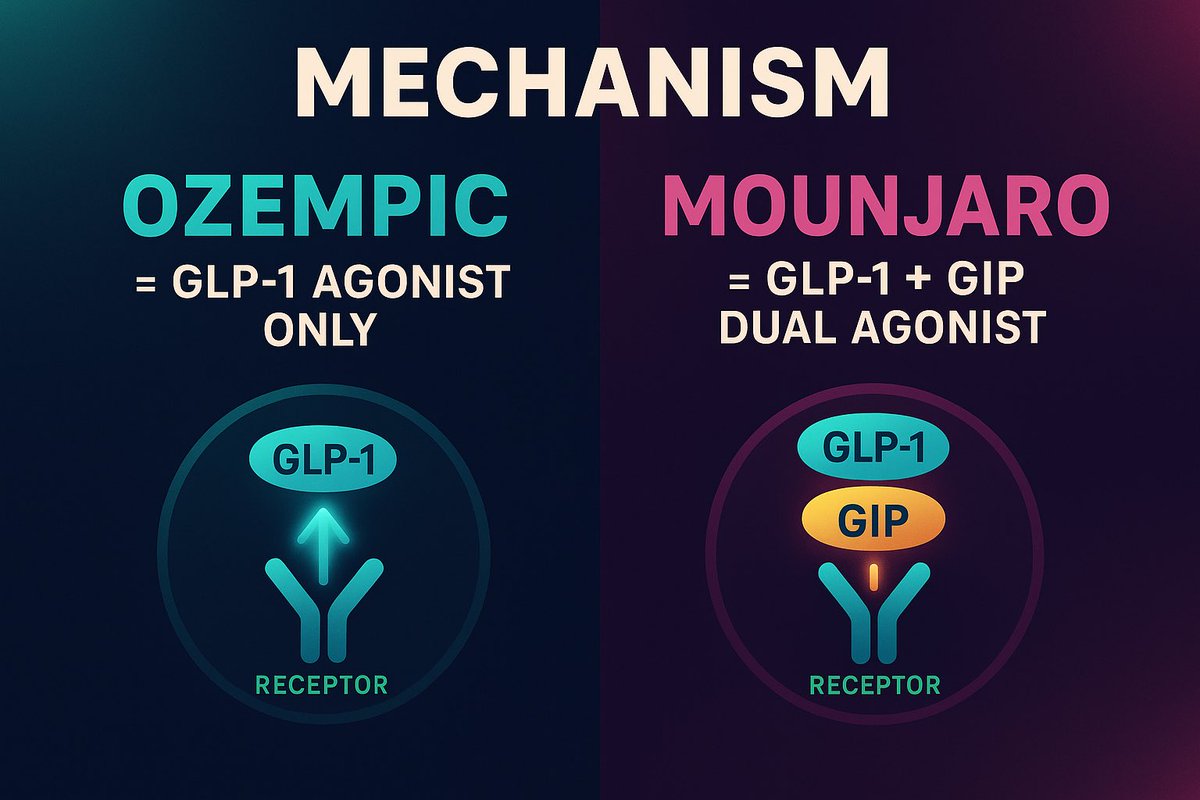
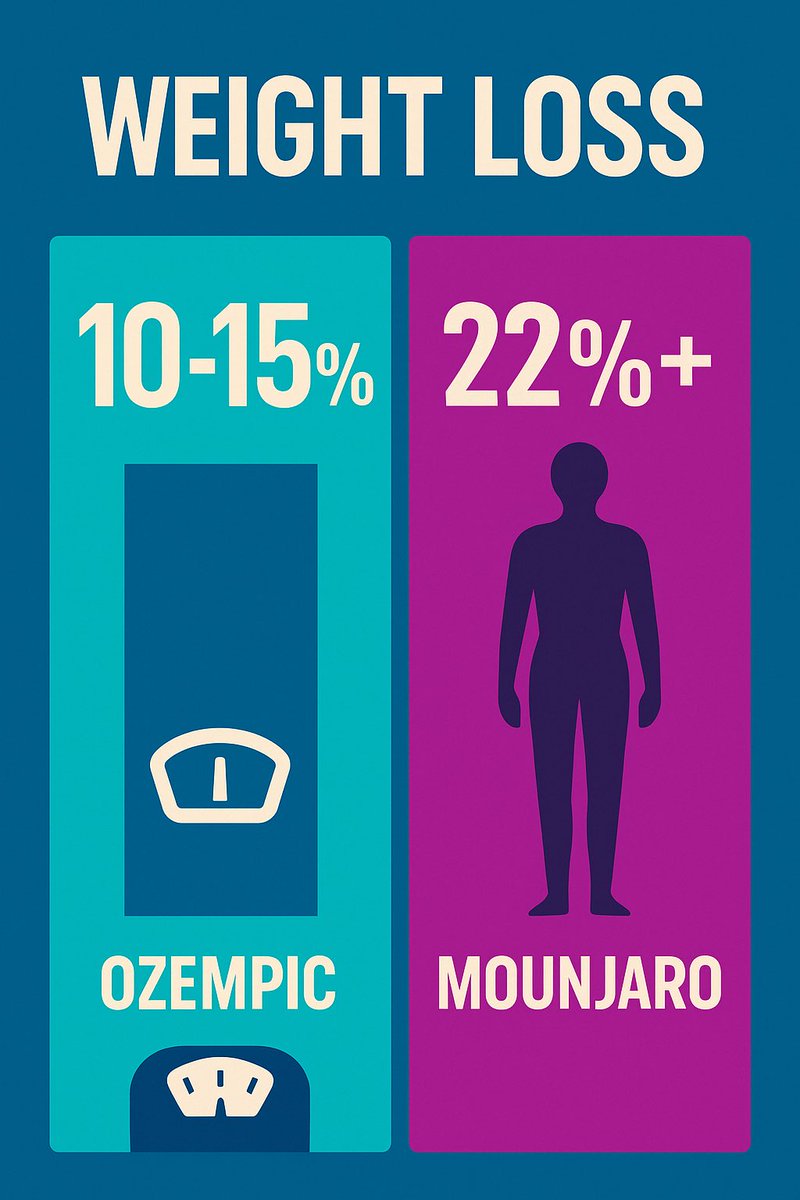
•New mention of GLP-1 and SGLT2 agonists as adjuncts for select CKD/obese/diabetes patients.
Guidelines offer specific recommendations for:
•CKD, diabetes, pregnancy, elderly, resistant HTN
•New mention of GLP-1 and SGLT2 agonists as adjuncts for select CKD/obese/diabetes patients.
9/ Equity and Outreach—New Priority
•Addressing care gaps in hypertension: Special call-out to improve equity and access in historically underserved and minoritized populations.
•Team-based care and outreach are now best practice.
•Addressing care gaps in hypertension: Special call-out to improve equity and access in historically underserved and minoritized populations.
•Team-based care and outreach are now best practice.
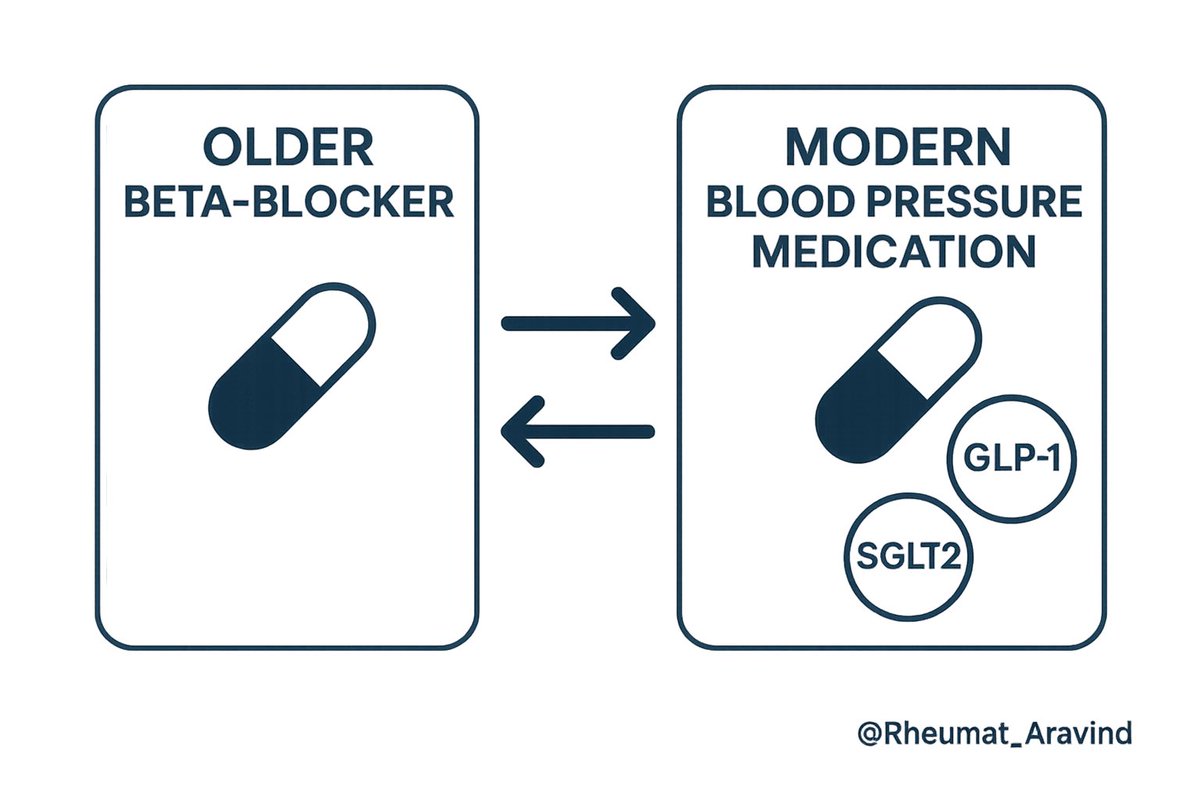
10/ Legacy Drugs & New Adjuncts
•Some older antihypertensives (simple beta-blockers, clonidine, hydralazine) are now only for specific indications—prefer modern agents for most.
•GLP-1 and SGLT2 inhibitors can be considered in high-risk or multi-comorbid adults.
•Some older antihypertensives (simple beta-blockers, clonidine, hydralazine) are now only for specific indications—prefer modern agents for most.
•GLP-1 and SGLT2 inhibitors can be considered in high-risk or multi-comorbid adults.
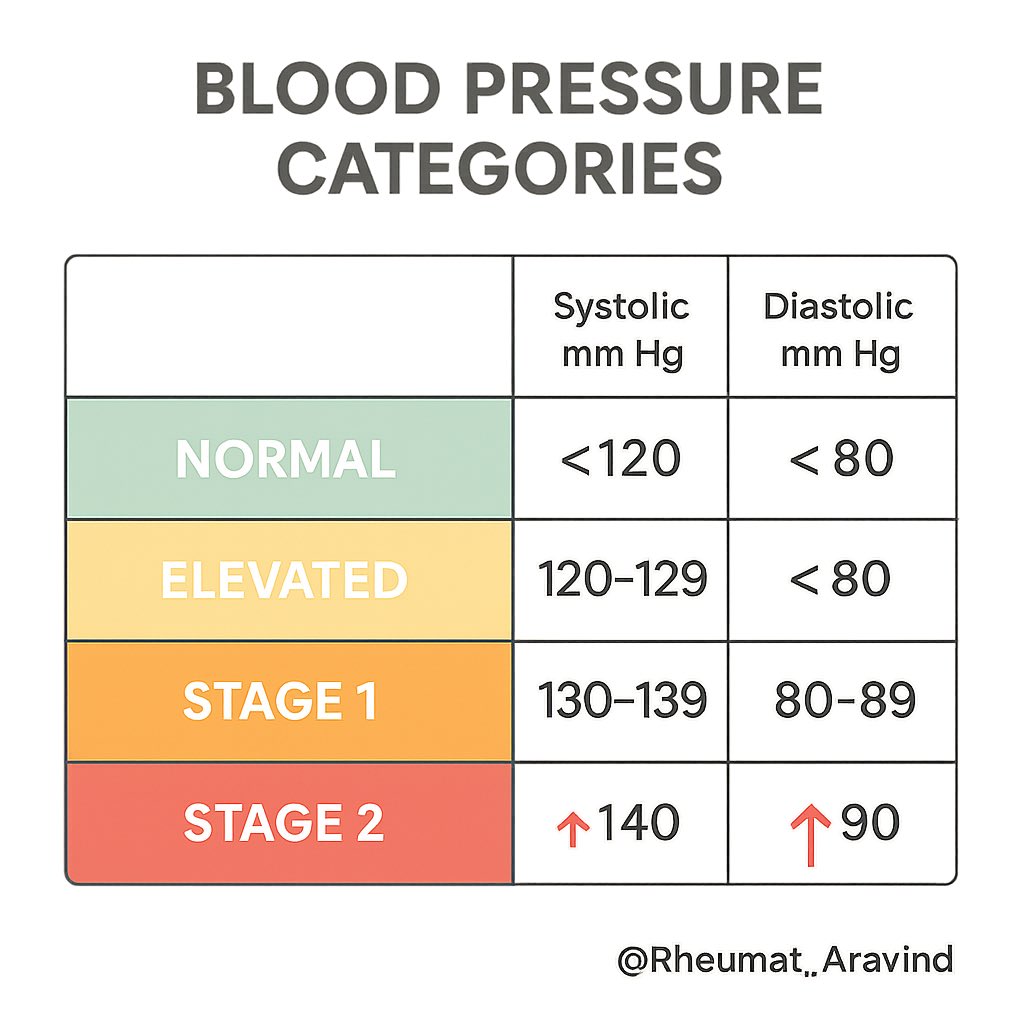
11/ BP Categories Unchanged, but Approach Is More Proactive
•Normal: <120/80 mm Hg
•Elevated: 120–129/<80 mm Hg
•Stage 1: 130–139/80–89 mm Hg
•Stage 2: ≥140/90 mm Hg
However, more patients with 130/80 and above will be started on medications if risk is moderate or higher, or if lifestyle fails.
•Normal: <120/80 mm Hg
•Elevated: 120–129/<80 mm Hg
•Stage 1: 130–139/80–89 mm Hg
•Stage 2: ≥140/90 mm Hg
However, more patients with 130/80 and above will be started on medications if risk is moderate or higher, or if lifestyle fails.
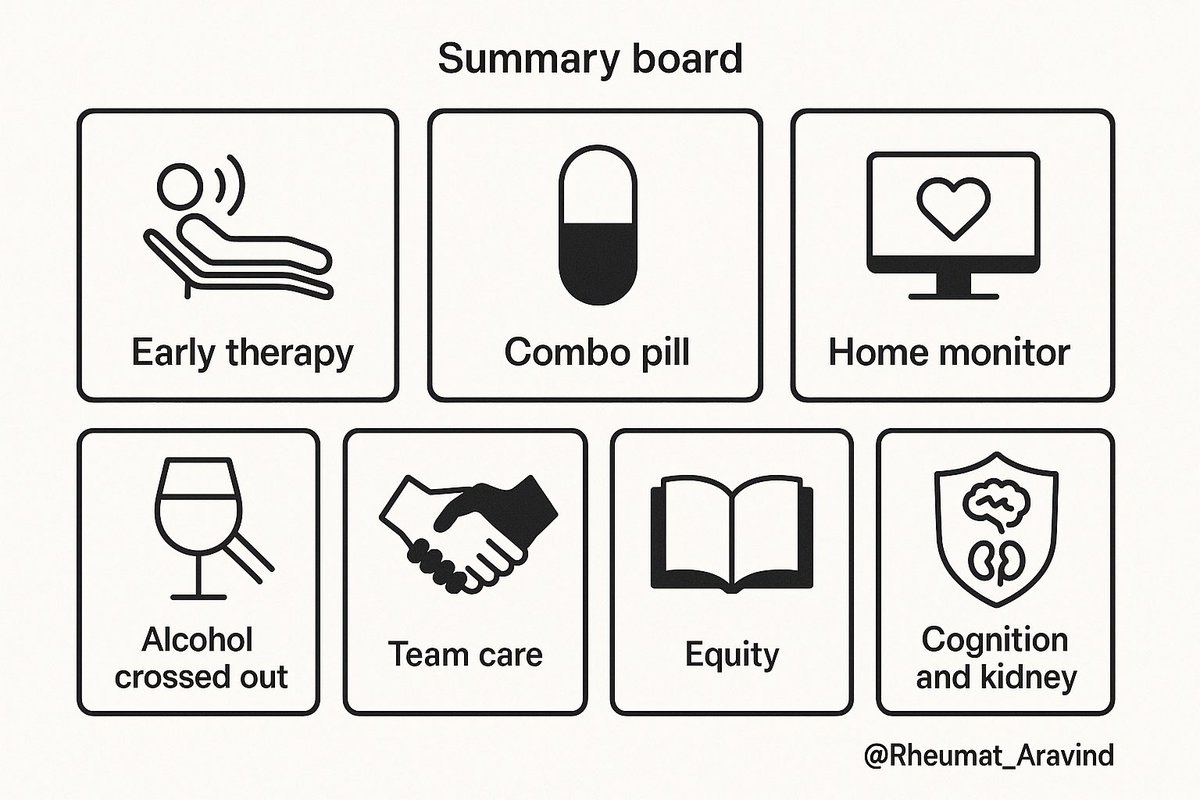
12/ Summary Takeaways
•Early, risk-based therapy
•Single-pill combos preferred
•Stronger lifestyle/alcohol guidance
•Validated home monitoring required
•Equity and outreach in focus
•Cognitive and kidney protection upgraded
Retweet to keep your colleagues, trainees, and patients up to date on the new AHA hypertension standard!
#Hypertension #AHAguidelines #BP2025
•Early, risk-based therapy
•Single-pill combos preferred
•Stronger lifestyle/alcohol guidance
•Validated home monitoring required
•Equity and outreach in focus
•Cognitive and kidney protection upgraded
Retweet to keep your colleagues, trainees, and patients up to date on the new AHA hypertension standard!
#Hypertension #AHAguidelines #BP2025
• • •
Missing some Tweet in this thread? You can try to
force a refresh