(Basic) ICU Hemodynamic “Secrets” - Part2:
I know you know them, but let’s remind ourselves of some additional basic hemodynamic "secrets":
I know you know them, but let’s remind ourselves of some additional basic hemodynamic "secrets":
16. Volume status is a nebulous term, but I don’t foresee stop using it anytime soon
17. The ultimate goal of hemodynamic management is adequate tissue perfusion (TP). TP may suffer even if the macrohemodynamic markers look good. This scenario is called “hemodynamic incoherence”. Sadly,
we don’t have yet a widely available, clinically useful, research-supported tool to monitor TP; it is the next frontier…
PS: Will it be capillary refill time?
PS: Will it be capillary refill time?
18. Several patients with pulmonary edema don’t suffer from “excess total fluid volume”; they are actually “euvolemic”, but a sympathetic system surge leads to increased arterial tone (increased afterload) & fluid redistribution. Therefore, diuretics are not the answer;
non-invasive ventilation and afterload reduction are more helpful (and faster!)
I will rephrase: some patients with pulmonary edema can be treated without diuretics...
I will rephrase: some patients with pulmonary edema can be treated without diuretics...
19. A patient can be at the same time both fluid-responsive and fluid intolerant. Sorry… 🤷♂️
20. Volume responsiveness is biventricular volume responsiveness; the left ventricle can eject only what it receives. Right ventricular failure is an important cause of insufficient left ventricular preload...
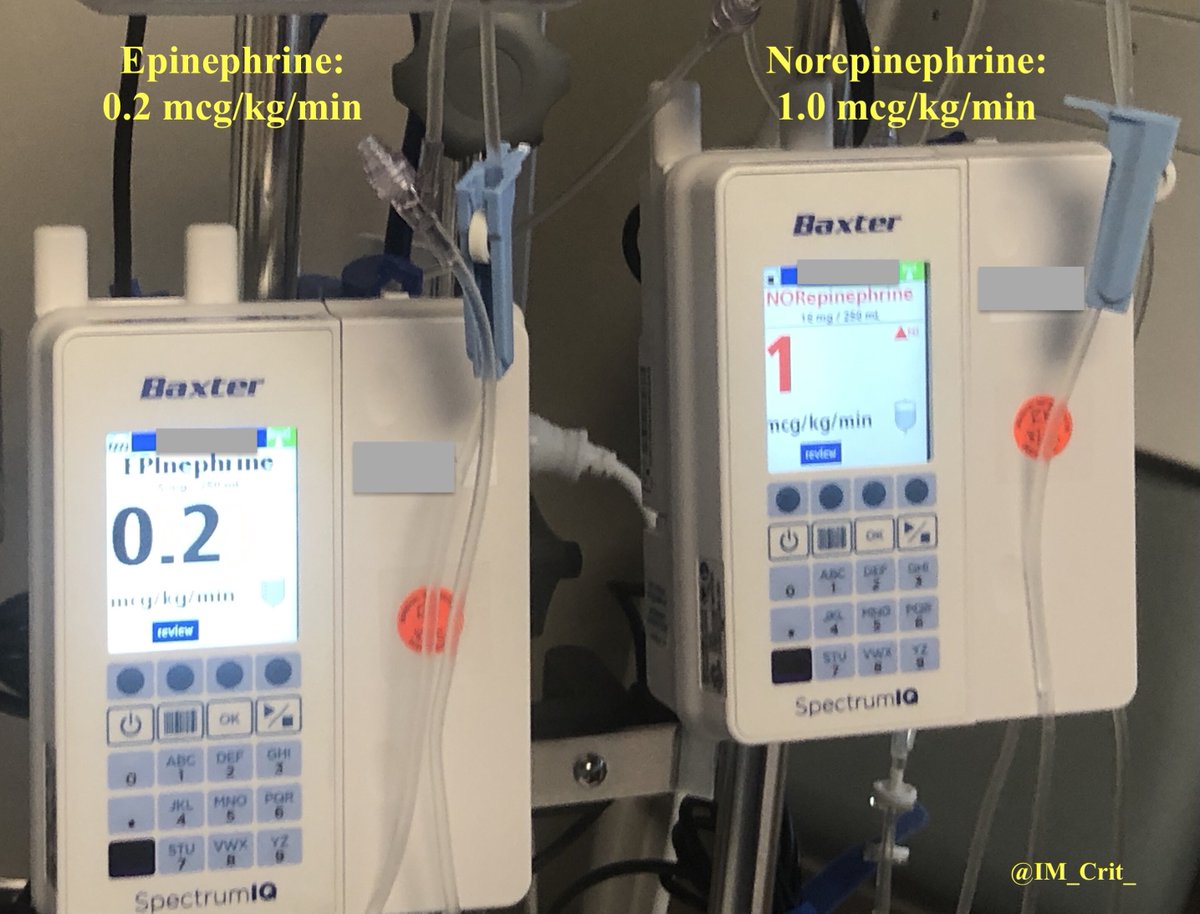
21. A hyperdynamic LV (“kissing” papillary muscles) on echo is not necessarily a sign of hypovolemia & should not reflexively trigger iv fluid bolus. Give yourself 1 mg of iv epinephrine and see what happens in your LV. Actually: don’t do it!
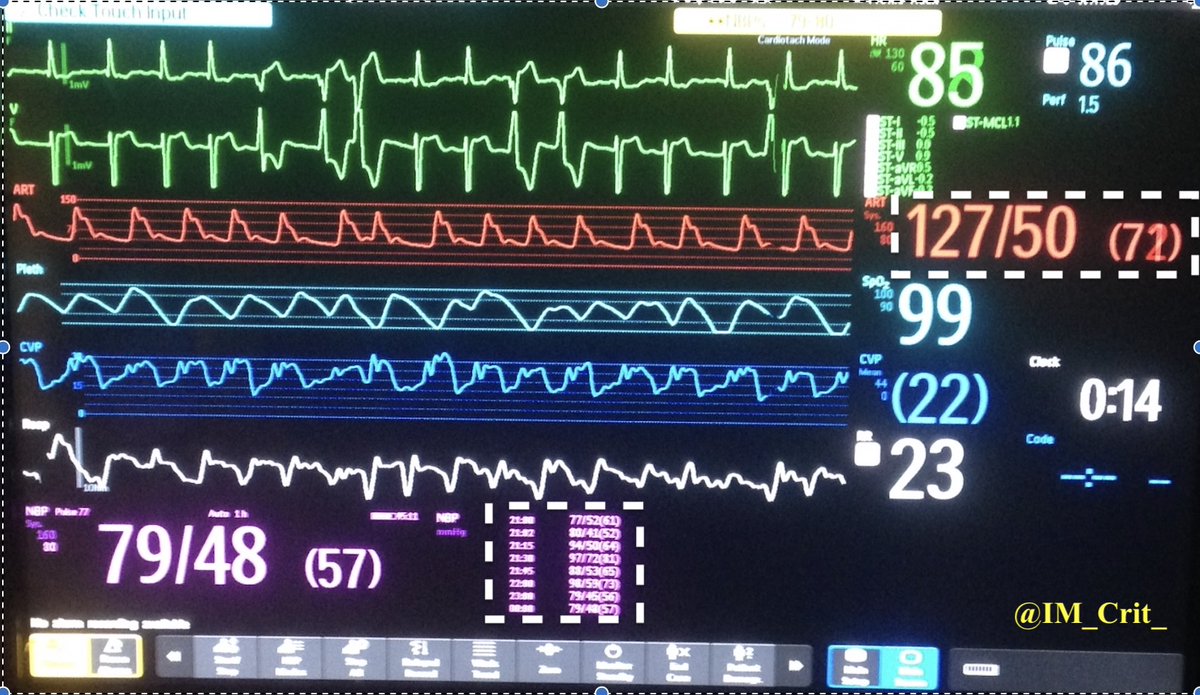
22. Right- and left-sided filling pressures may be discordant. A patient may have a wedge of 8 mmHg and a CVP of 20 mmHg or the other way around…
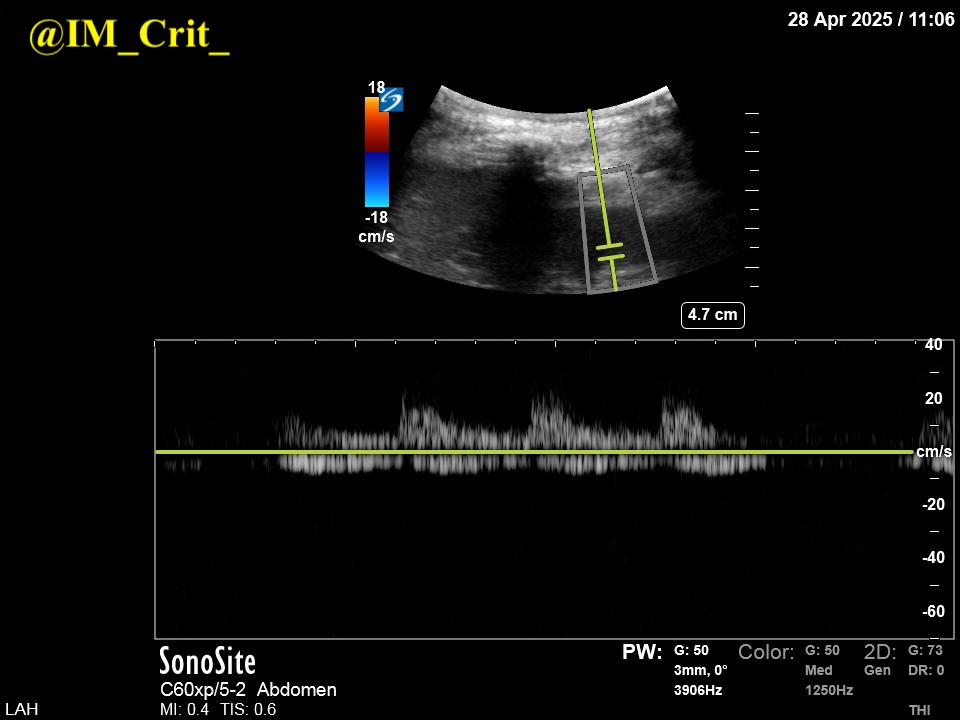
23. A patient can have venous congestion without any sign of peripheral edema. At all..
24. Patients on vasopressors can still receive diuretics for the right reason and with the appropriate monitoring!
25. When managing a patient with venous congestion: Diuretic drips are not more effective than diuretic boluses
Bonus info: there is no magical ingredient in bumetanide (Bumex in 🇺🇸)!
Bonus info: there is no magical ingredient in bumetanide (Bumex in 🇺🇸)!
27. The right ventricle is not important until it is!
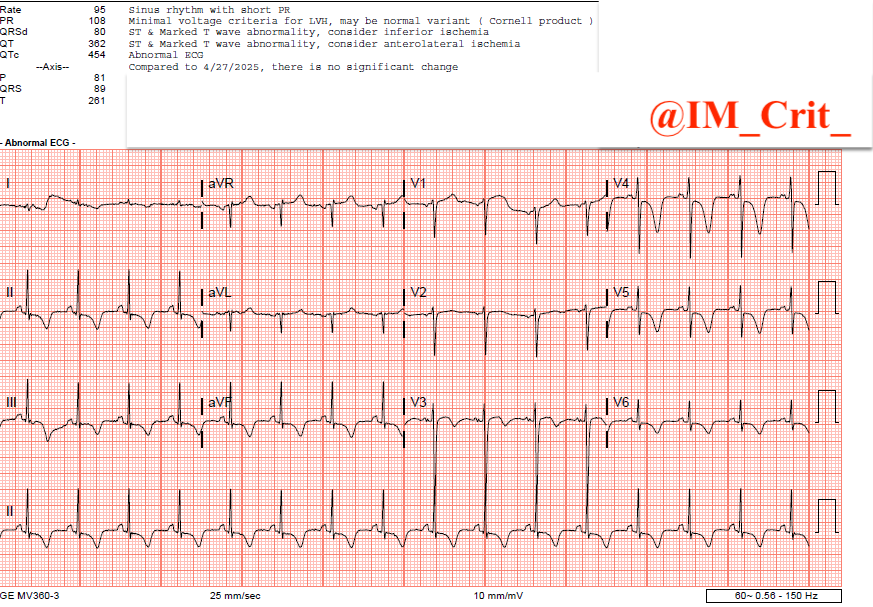
28. LV outflow tract obstruction (LVOTO) should be suspected in any patient with shock refractory to vasopressors/inotropes, especially if you dial up the inotropes and the patient gets worse!
29. LVOTO and stress-cardiomyopathy are quite common in Critical Care; more common than you think! Please use #pocus
30. Hemodynamic monitors do not improve patient outcomes; sensible therapeutic interventions based on a combination of data points (including the ones provided by monitors) can improve outcomes
#foamed #foamcc #meded #MedTwitter
Thanks for following!
Thanks for following!
• • •
Missing some Tweet in this thread? You can try to
force a refresh