How to get URL link on X (Twitter) App
https://twitter.com/jameshorowitzmd/status/1956094011770343557
 OHCA: Epi increases survival but no neuro recovery
OHCA: Epi increases survival but no neuro recovery

 In this study, 32 ♂ C57B/l6 🐭 (10 wks; 30 g) were exposed to 3 types of light (red, blue & ambient white). Light sources, equipped with blue & red filters, ensured illumination of ~1400 lux at the cages. A control group experienced ambient white, fluorescent lighting at 400 lux
In this study, 32 ♂ C57B/l6 🐭 (10 wks; 30 g) were exposed to 3 types of light (red, blue & ambient white). Light sources, equipped with blue & red filters, ensured illumination of ~1400 lux at the cages. A control group experienced ambient white, fluorescent lighting at 400 lux 

 Fact:
Fact:



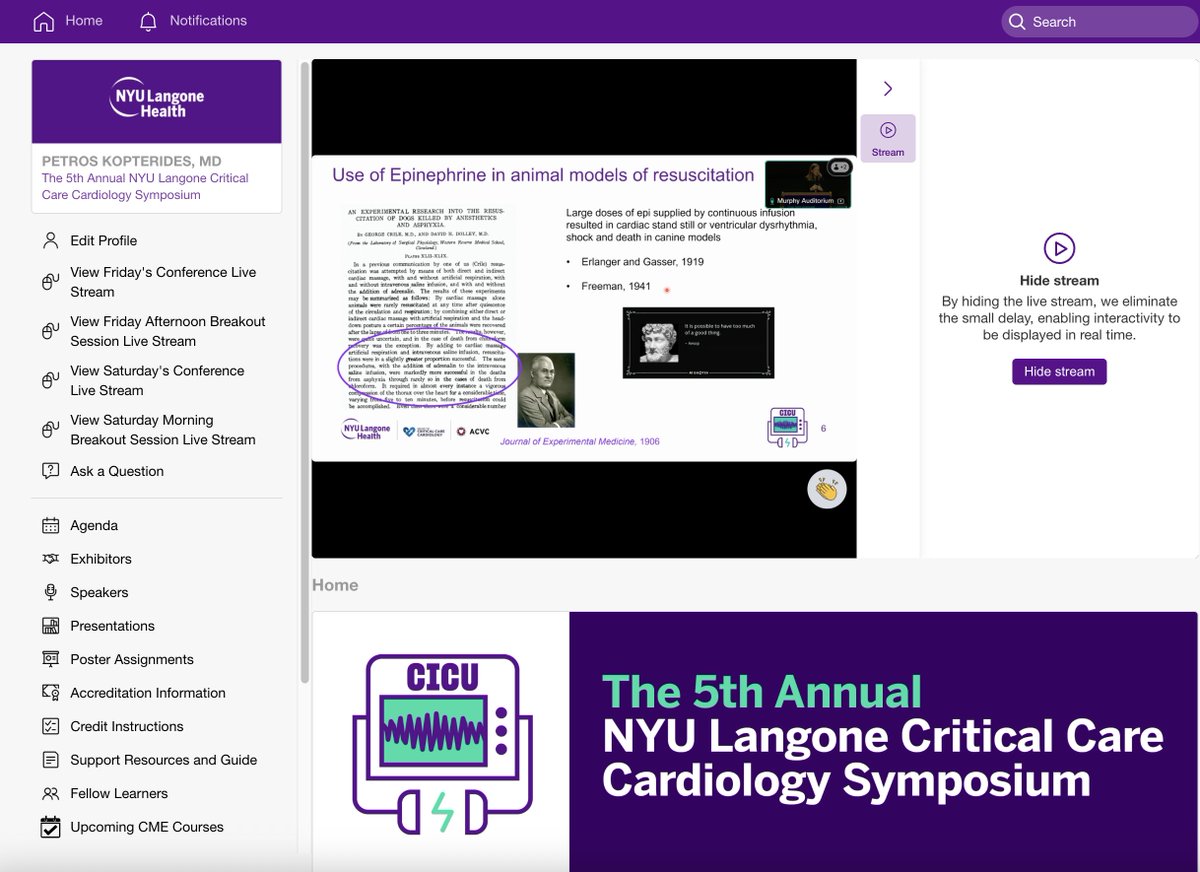
 In this aggressively diuresed population (560 mg iv furosemide -> urine output of 8425 mL over 72h), both worsening renal function & increases in tubular injury biomarkers were not associated with adverse outcomes; rather, there was a trend towards improved outcomes
In this aggressively diuresed population (560 mg iv furosemide -> urine output of 8425 mL over 72h), both worsening renal function & increases in tubular injury biomarkers were not associated with adverse outcomes; rather, there was a trend towards improved outcomes 

 A day later, the blood culture grows Gram (-) rods (eventually proven to be the same bug). The susceptibility profile is:
A day later, the blood culture grows Gram (-) rods (eventually proven to be the same bug). The susceptibility profile is: 

 This is not an uncommon scenario: a "low" expired tidal volumes (Vt) makes the staff worried during NIV initiated for hypoxemic respiratory failure but a "high" Vt (even if accurately measured) is left unabated...
This is not an uncommon scenario: a "low" expired tidal volumes (Vt) makes the staff worried during NIV initiated for hypoxemic respiratory failure but a "high" Vt (even if accurately measured) is left unabated...
 This guideline update focuses only on immunocompetent adult patients with a standard diagnosis of CAP
This guideline update focuses only on immunocompetent adult patients with a standard diagnosis of CAP


 is one of the least debatable ones. Time is life in sepsis!
is one of the least debatable ones. Time is life in sepsis! 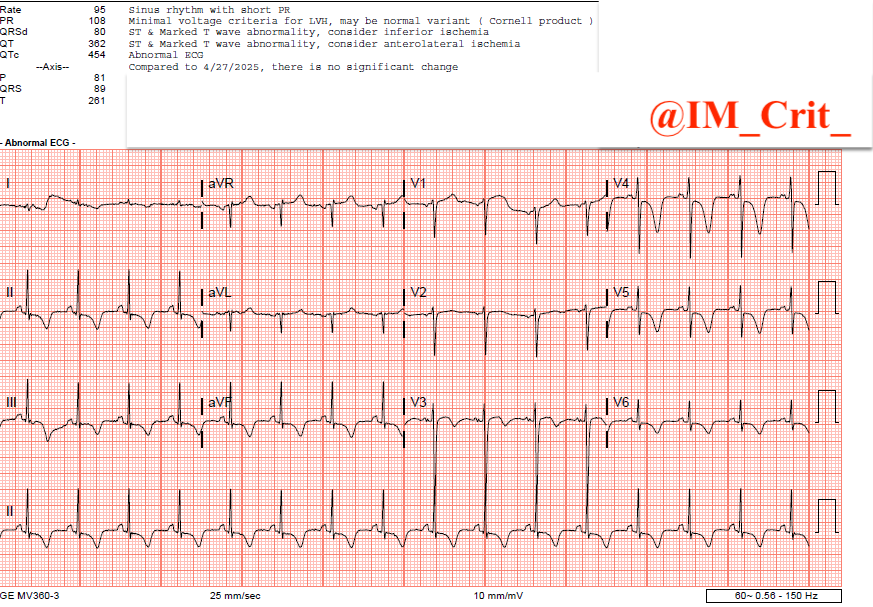
https://twitter.com/IM_Crit_/status/1916606026742170070
 I repeated #POCUS; no significant changes:
I repeated #POCUS; no significant changes:

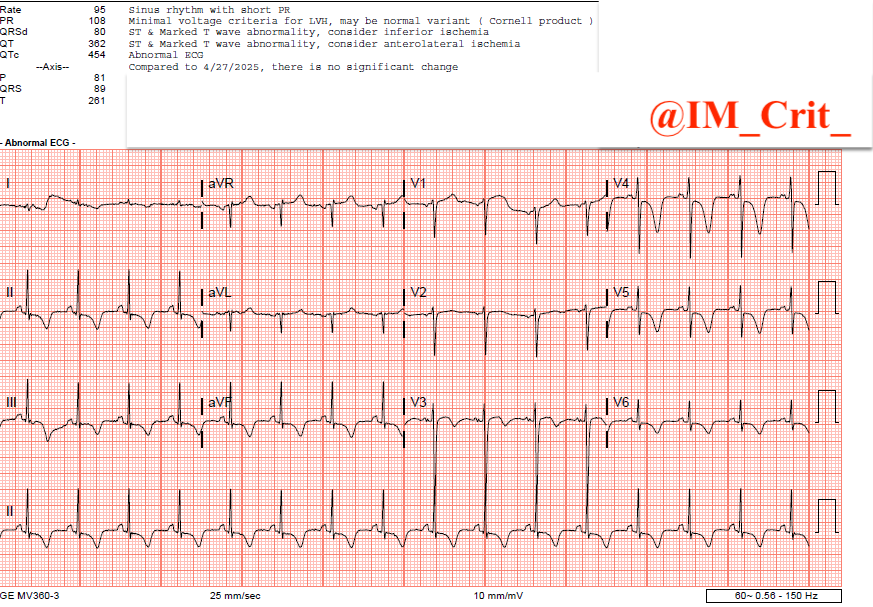
 It's unfortunately hard to pretend you didn't see it, so you get an ECG praying that it will not show what you saw on the monitor... 😊
It's unfortunately hard to pretend you didn't see it, so you get an ECG praying that it will not show what you saw on the monitor... 😊

 in the same vessel, if there is anatomical reason/venous thrombosis etc that limits the available options. I have even placed a 3rd line (Swan sheath) in the RIJ at the same time but the more of venous real estate is occupied by catheter lumens,
in the same vessel, if there is anatomical reason/venous thrombosis etc that limits the available options. I have even placed a 3rd line (Swan sheath) in the RIJ at the same time but the more of venous real estate is occupied by catheter lumens,
 Vasoplegic shock (VS) is common, contributing up to two-thirds of cases of shock admitted to the ICU
Vasoplegic shock (VS) is common, contributing up to two-thirds of cases of shock admitted to the ICU

 IR found severe L subclavian stenosis at the intersection of the clavicle & 2nd rib & upstream LUE extensive DVT. Performed successful image-guided LUE DVT mechanical thrombectomy & stenotic site angioplasty with near complete resolution of clot burden & improvement of stenosis
IR found severe L subclavian stenosis at the intersection of the clavicle & 2nd rib & upstream LUE extensive DVT. Performed successful image-guided LUE DVT mechanical thrombectomy & stenotic site angioplasty with near complete resolution of clot burden & improvement of stenosis

 The 1st fluid challenge resulted in a large ⬆️ in LV stroke volume (38 to 65 mL), whereas the 2nd was unsuccessful (65 to 69 mL). The mitral Doppler profile progressed from “abnormal relaxation” to “restriction to filling” consistent with a gradual ⬆️ in left cardiac pressures
The 1st fluid challenge resulted in a large ⬆️ in LV stroke volume (38 to 65 mL), whereas the 2nd was unsuccessful (65 to 69 mL). The mitral Doppler profile progressed from “abnormal relaxation” to “restriction to filling” consistent with a gradual ⬆️ in left cardiac pressures
