A COVID infection, particularly in women, may lead to blood vessels aging around five years!
➡️ Blood vessels gradually become stiffer with age, but the new study suggests that COVID could accelerate this process. Researchers say this is important since people with stiffer blood vessels face a higher risk of cardiovascular disease, including stroke and heart attack. 1/
➡️ Blood vessels gradually become stiffer with age, but the new study suggests that COVID could accelerate this process. Researchers say this is important since people with stiffer blood vessels face a higher risk of cardiovascular disease, including stroke and heart attack. 1/

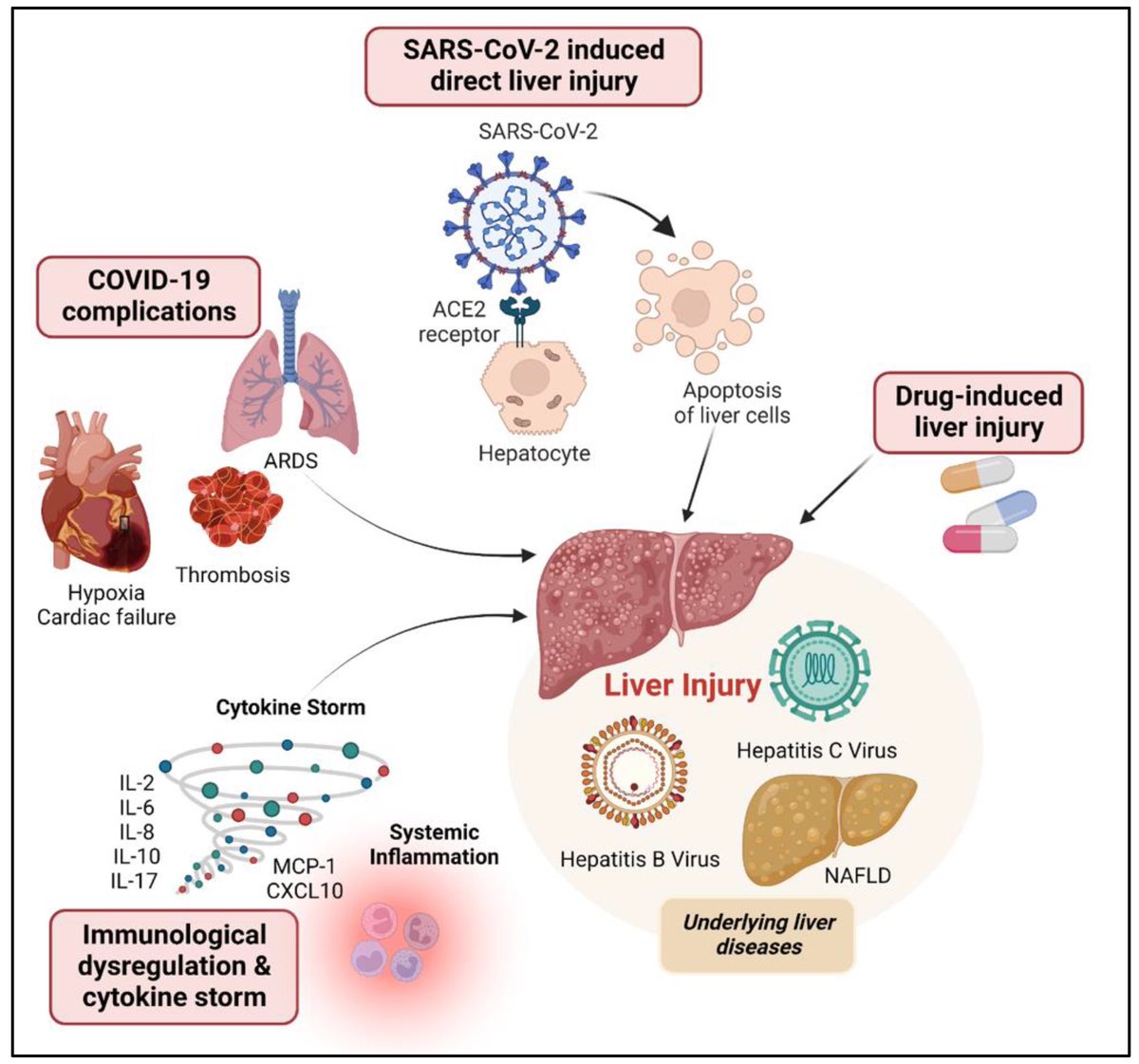
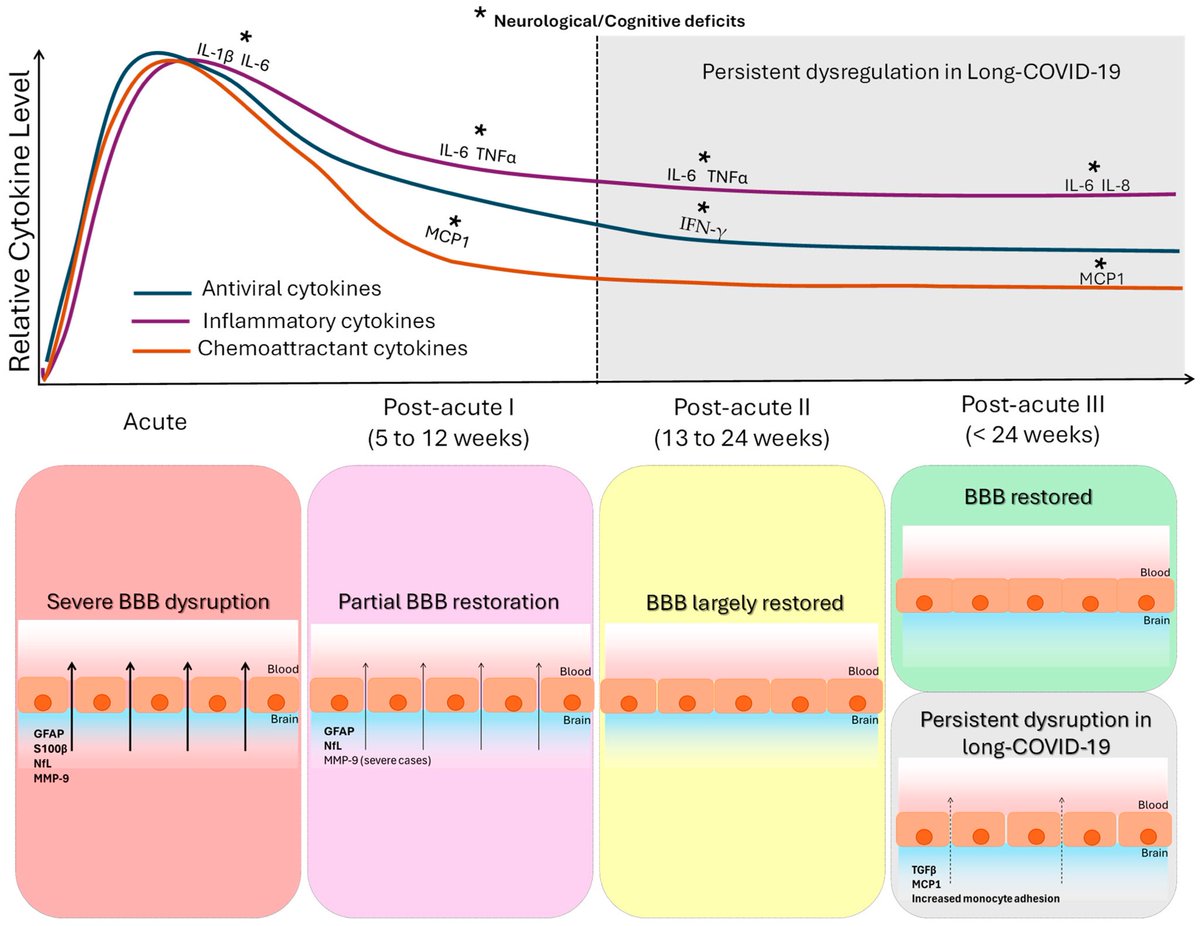
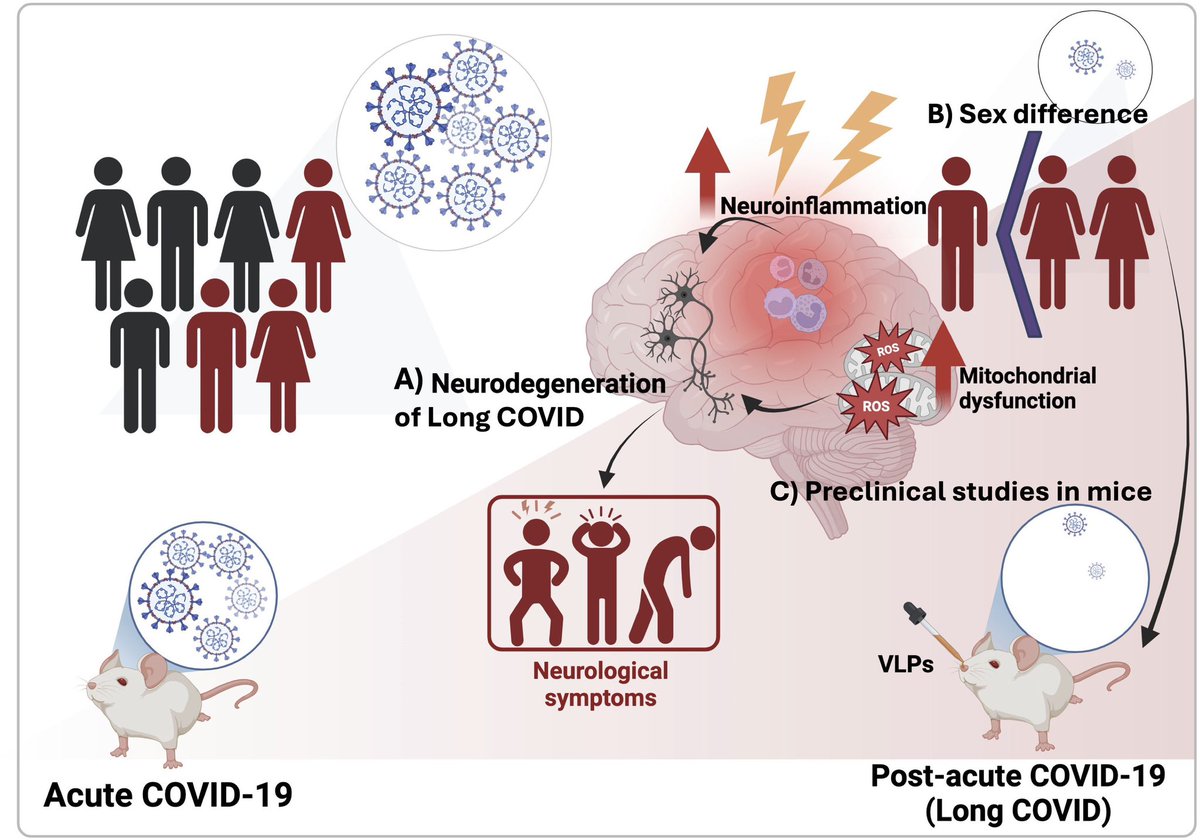
Since the pandemic, we have learned that many people who have had COVID are left with symptoms that can last for months or even years. However, we are still learning what's happening in the body to create these symptoms. 2/ 

It is known that COVID can directly affect blood vessels. This may result in what we call early vascular aging, meaning that your blood vessels are older than your chronological age and you are more susceptible to heart disease.
If that is happening, we need to identify who is at risk at an early stage to prevent heart attacks and strokes. 3/
If that is happening, we need to identify who is at risk at an early stage to prevent heart attacks and strokes. 3/

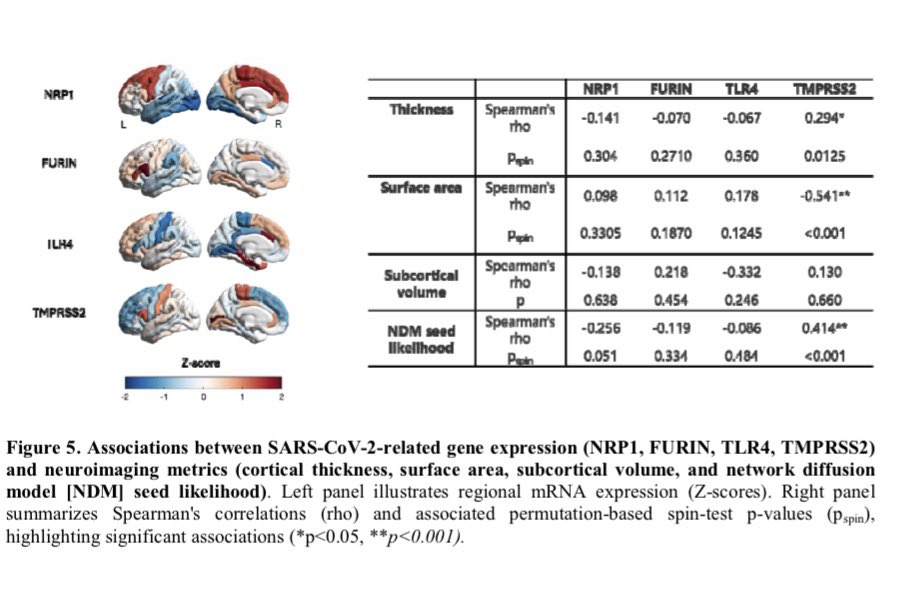
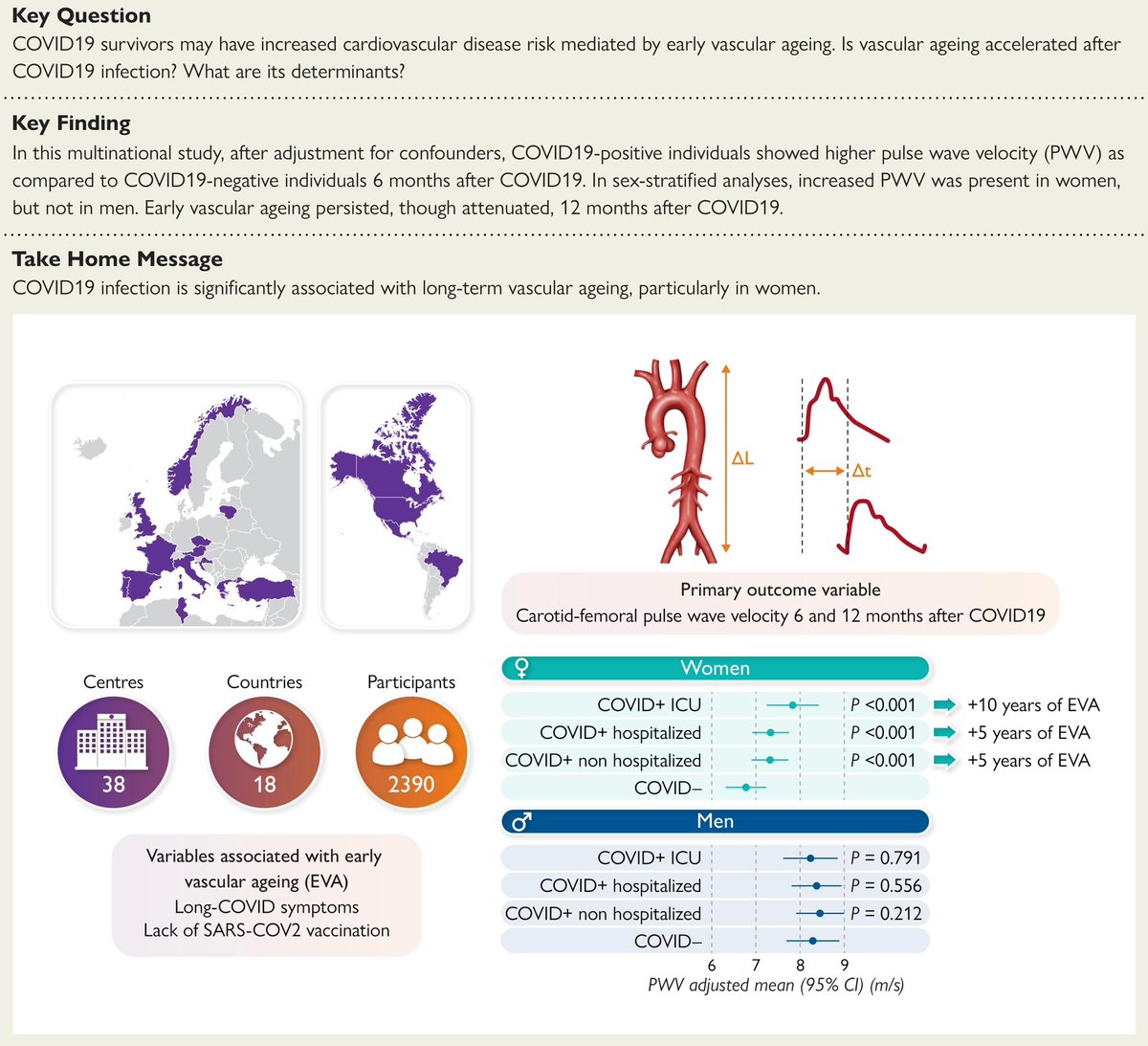
The study included 2,390 people from 16 different countries who were recruited between September 2020 to February 2022.
They were categorized according to whether they had never had COVID, had recent COVID but were not hospitalized, hospitalized for COVID on a general ward or hospitalized for COVID in an intensive care unit. 4/
They were categorized according to whether they had never had COVID, had recent COVID but were not hospitalized, hospitalized for COVID on a general ward or hospitalized for COVID in an intensive care unit. 4/
Researchers assessed each person's vascular age with a device that measures how quickly a wave of blood pressure travels between the carotid artery(in the neck) and femoral arteries (in the legs), a measure called carotid-femoral pulse wave velocity (PWV).
The higher this measurement, the stiffer the blood vessels and the higher the vascular age of a person. Measurements were taken six months after COVID infection and again after 12 months. 5/
The higher this measurement, the stiffer the blood vessels and the higher the vascular age of a person. Measurements were taken six months after COVID infection and again after 12 months. 5/
The researchers found that all three groups of patients who had been infected with COVID, including those with mild COVID, had stiffer arteries, compared to those who had not been infected.
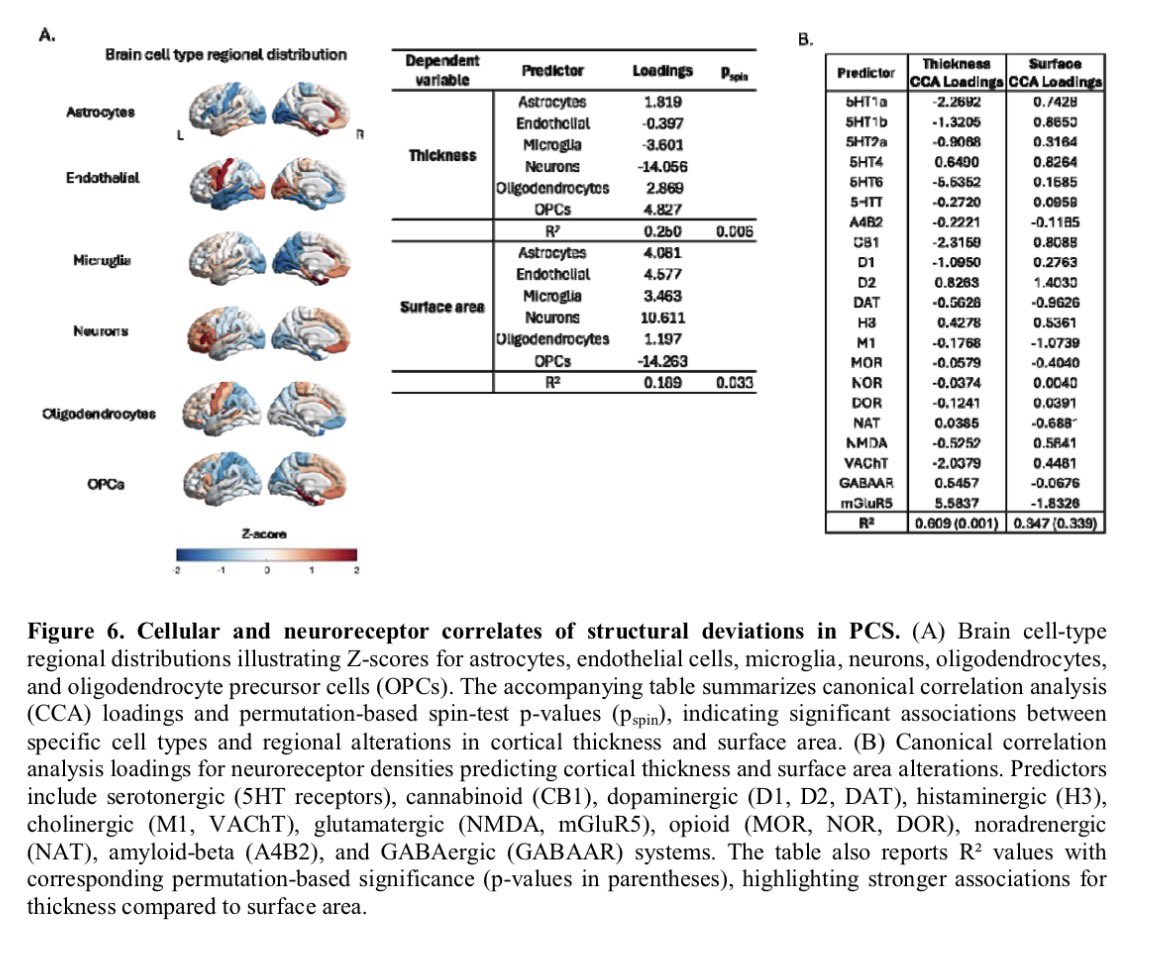
The effect was greater in women than in men and in people who experienced the persistent symptoms of #longCOVID, such as shortness of breath and fatigue. 6/

The effect was greater in women than in men and in people who experienced the persistent symptoms of #longCOVID, such as shortness of breath and fatigue. 6/
The average increase in PWV in women who had mild COVID was 0.55 meters per second, 0.60 in women hospitalized with COVID, and 1.09 for women treated in intensive care.
Researchers say an increase of around 0.5 meters per second is "clinically relevant" and equivalent to aging around five years, with a 3% increased risk of cardiovascular disease in a 60-year-old woman. 7/
Researchers say an increase of around 0.5 meters per second is "clinically relevant" and equivalent to aging around five years, with a 3% increased risk of cardiovascular disease in a 60-year-old woman. 7/
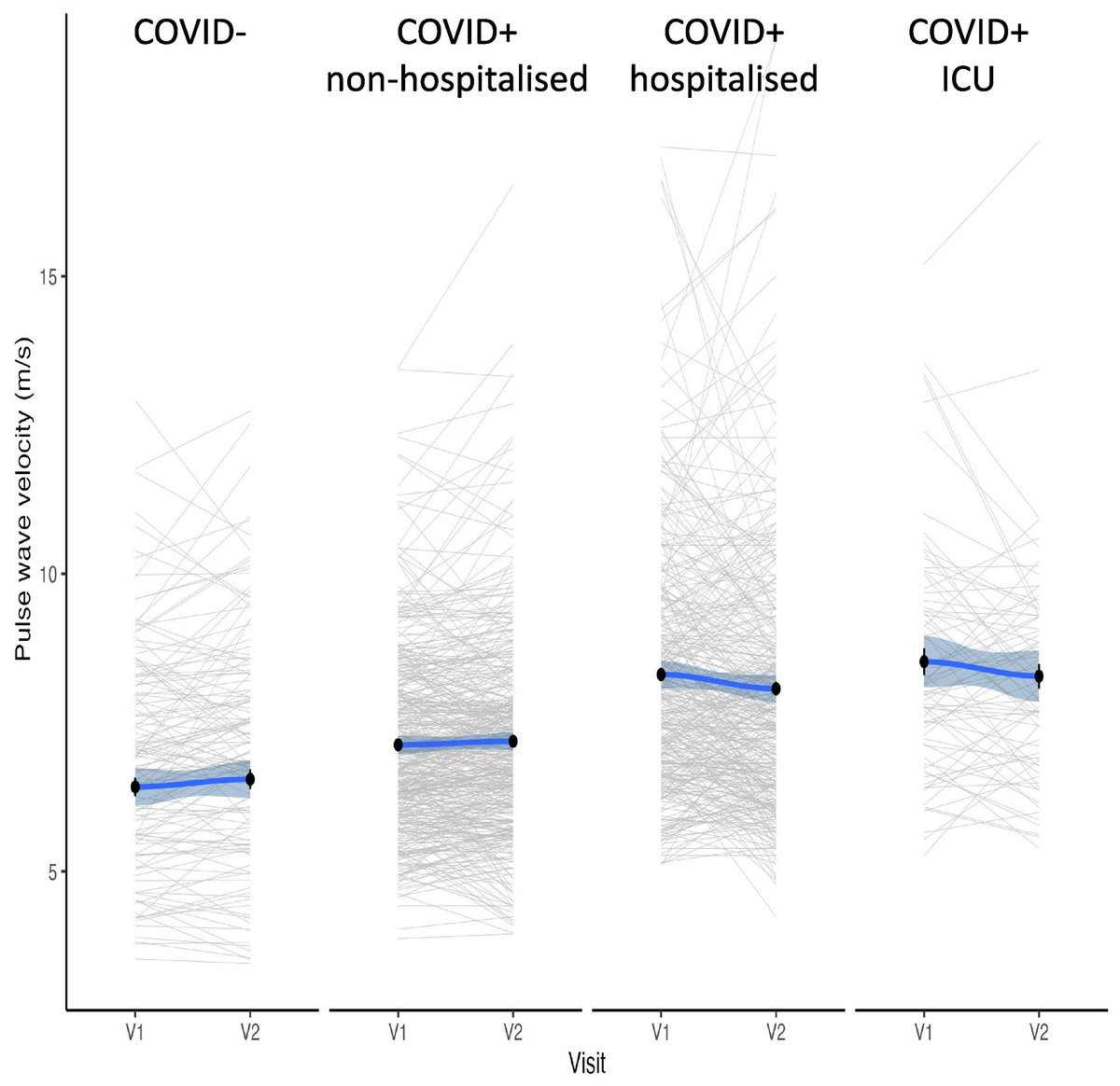
People who had been vaccinated against COVID generally had arteries that were less stiff than people who were unvaccinated. Over the longer term, the vascular aging associated with COVID infection seemed to stabilize or improve slightly. 8/8
academic.oup.com/eurheartj/adva…
academic.oup.com/eurheartj/adva…
• • •
Missing some Tweet in this thread? You can try to
force a refresh