Which antidepressants work most effectively, and which barely beat placebo?
The largest meta-analysis (Cipriani et al., 2018) compared 21 antidepressants in 116,477 patients, revealing striking differences in efficacy and tolerability.
Here’s how this data can transform your prescribing practice 🧵👇
The largest meta-analysis (Cipriani et al., 2018) compared 21 antidepressants in 116,477 patients, revealing striking differences in efficacy and tolerability.
Here’s how this data can transform your prescribing practice 🧵👇

Most ‘Effective’ Antidepressants (Head-to-Head)
In the largest network meta-analysis to date, the following antidepressants consistently outperformed others in head-to-head comparisons for efficacy (odds ratio range: 1.19–1.96):
● Agomelatine
● Amitriptyline
● Escitalopram
● Mirtazapine
● Paroxetine
These consistently outperformed others.
Note: Just because a drug ranks high in efficacy doesn’t mean it’s the best choice for every patient.
In the largest network meta-analysis to date, the following antidepressants consistently outperformed others in head-to-head comparisons for efficacy (odds ratio range: 1.19–1.96):
● Agomelatine
● Amitriptyline
● Escitalopram
● Mirtazapine
● Paroxetine
These consistently outperformed others.
Note: Just because a drug ranks high in efficacy doesn’t mean it’s the best choice for every patient.

The Numbers Behind Antidepressant’s Efficacy
Odds ratios (OR) provide a clearer picture.
● Amitriptyline: OR = 2.13 (113% higher odds vs. placebo)
● Reboxetine: OR = 1.37 (37% higher odds)
All drugs beat the placebo, but not equally.
Higher OR = greater efficacy.
Odds ratios (OR) provide a clearer picture.
● Amitriptyline: OR = 2.13 (113% higher odds vs. placebo)
● Reboxetine: OR = 1.37 (37% higher odds)
All drugs beat the placebo, but not equally.
Higher OR = greater efficacy.

Well-Tolerated Antidepressants (Lower Dropout Rates)
Patients are more likely to stick with well-tolerated treatments.
Cipriani et al. (2018) found:
● Agomelatine, citalopram, escitalopram, fluoxetine, sertraline, and vortioxetine → better acceptability than many other antidepressants.
● Only agomelatine & fluoxetine had fewer dropouts than placebo.
● The others were not superior to placebo on this metric.
Patients are more likely to stick with well-tolerated treatments.
Cipriani et al. (2018) found:
● Agomelatine, citalopram, escitalopram, fluoxetine, sertraline, and vortioxetine → better acceptability than many other antidepressants.
● Only agomelatine & fluoxetine had fewer dropouts than placebo.
● The others were not superior to placebo on this metric.
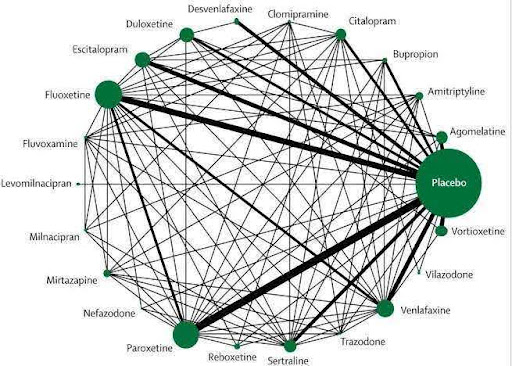
Balancing Efficacy and Tolerability
No drug is perfect. Clinicians must balance efficacy with tolerability:
● Amitriptyline: Highly effective but poorly tolerated.
● Escitalopram & Agomelatine: Offer a strong balance of both.
This is the cornerstone of personalised prescribing.
No drug is perfect. Clinicians must balance efficacy with tolerability:
● Amitriptyline: Highly effective but poorly tolerated.
● Escitalopram & Agomelatine: Offer a strong balance of both.
This is the cornerstone of personalised prescribing.
Best/Worst Overview
Efficacy leaders:
Agomelatine, Amitriptyline, Escitalopram, Mirtazapine, Paroxetine, Venlafaxine, Vortioxetine.
Tolerability leaders:
Agomelatine, Citalopram, Escitalopram, Fluoxetine, Sertraline, Vortioxetine.
Caution:
● Least efficacy— Fluoxetine, Fluvoxamine, Reboxetine, Trazodone.
● High dropout— Amitriptyline, Clomipramine, Duloxetine, Fluvoxamine, Reboxetine, Trazodone, Venlafaxine.
Efficacy leaders:
Agomelatine, Amitriptyline, Escitalopram, Mirtazapine, Paroxetine, Venlafaxine, Vortioxetine.
Tolerability leaders:
Agomelatine, Citalopram, Escitalopram, Fluoxetine, Sertraline, Vortioxetine.
Caution:
● Least efficacy— Fluoxetine, Fluvoxamine, Reboxetine, Trazodone.
● High dropout— Amitriptyline, Clomipramine, Duloxetine, Fluvoxamine, Reboxetine, Trazodone, Venlafaxine.
Why This Study Stands Out
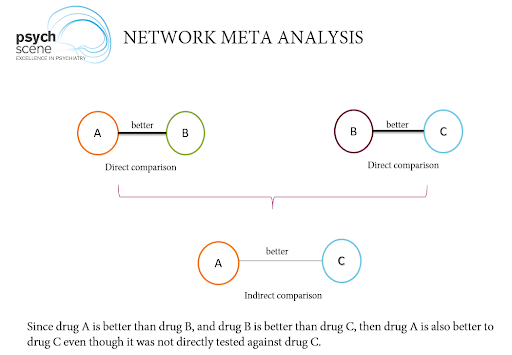
This network meta-analysis was groundbreaking, including:
● Data from 522 trials (published + unpublished).
● Direct and indirect comparisons of 21 drugs.
Strengths: Largest antidepressant dataset, reduced publication bias.
Limitations: Short trial durations (<12 weeks) and exclusion of treatment-resistant/psychotic depression.
This network meta-analysis was groundbreaking, including:
● Data from 522 trials (published + unpublished).
● Direct and indirect comparisons of 21 drugs.
Strengths: Largest antidepressant dataset, reduced publication bias.
Limitations: Short trial durations (<12 weeks) and exclusion of treatment-resistant/psychotic depression.
Practical Prescribing Tips
Use these insights to refine your practice:
● Prioritise efficacy leaders when maximising response.
● Choose tolerability leaders for side-effect-sensitive patients.
● Use shared decision-making to align choice with patient needs.
Use these insights to refine your practice:
● Prioritise efficacy leaders when maximising response.
● Choose tolerability leaders for side-effect-sensitive patients.
● Use shared decision-making to align choice with patient needs.
Personalised Treatment Improves Outcomes
STAR*D showed that after first-line antidepressant treatment:
●~47% respond (~1 in 2)
●~27–37% remit (~1 in 3, scale-dependent)
Balancing efficacy, tolerability, and patient preferences is key to improving outcomes.
Learn more about antidepressant medications and delve deep into their intricate mechanisms of action below 👇
STAR*D showed that after first-line antidepressant treatment:
●~47% respond (~1 in 2)
●~27–37% remit (~1 in 3, scale-dependent)
Balancing efficacy, tolerability, and patient preferences is key to improving outcomes.
Learn more about antidepressant medications and delve deep into their intricate mechanisms of action below 👇
Refine Your Prescribing Expertise
Our course, ‘Antidepressant Mechanisms & Management: Advanced Training for Psychiatrists’, equips you with the tools to refine your decision-making and improve patient outcomes.
Access the full course on The Academy.
psychscene.co/4jjdnZb
Our course, ‘Antidepressant Mechanisms & Management: Advanced Training for Psychiatrists’, equips you with the tools to refine your decision-making and improve patient outcomes.
Access the full course on The Academy.
psychscene.co/4jjdnZb
• • •
Missing some Tweet in this thread? You can try to
force a refresh