7 key differences in females with ADHD
Females present with a specific neurobehavioural profile that may contribute to an underdiagnosis and subsequent under-treatment.
Here’s what clinicians need to assess and look out for
🧵👇
Females present with a specific neurobehavioural profile that may contribute to an underdiagnosis and subsequent under-treatment.
Here’s what clinicians need to assess and look out for
🧵👇

1/ Under-recognised, different profile.
Girls/women with ADHD often present with internalising symptoms (low mood, anxiety, emotional lability), so they’re mislabelled with mood/personality disorders and referred late.
💡 Psych Scene Tip:
If chronic anxiety/low mood rides alongside lifelong disorganisation, time-blindness, and procrastination across settings (since <12), screen for ADHD before defaulting to mood/BPD labels.
Girls/women with ADHD often present with internalising symptoms (low mood, anxiety, emotional lability), so they’re mislabelled with mood/personality disorders and referred late.
💡 Psych Scene Tip:
If chronic anxiety/low mood rides alongside lifelong disorganisation, time-blindness, and procrastination across settings (since <12), screen for ADHD before defaulting to mood/BPD labels.
2/ Masking + compensation delay diagnosis.
Compliance, resilience, perfectionism, and high structure (supportive family/school) can temporarily “hide” impairment, until demands rise.
Expect later recognition at transitions (primary→secondary school, university, new job, parenthood). 
Compliance, resilience, perfectionism, and high structure (supportive family/school) can temporarily “hide” impairment, until demands rise.
Expect later recognition at transitions (primary→secondary school, university, new job, parenthood). 
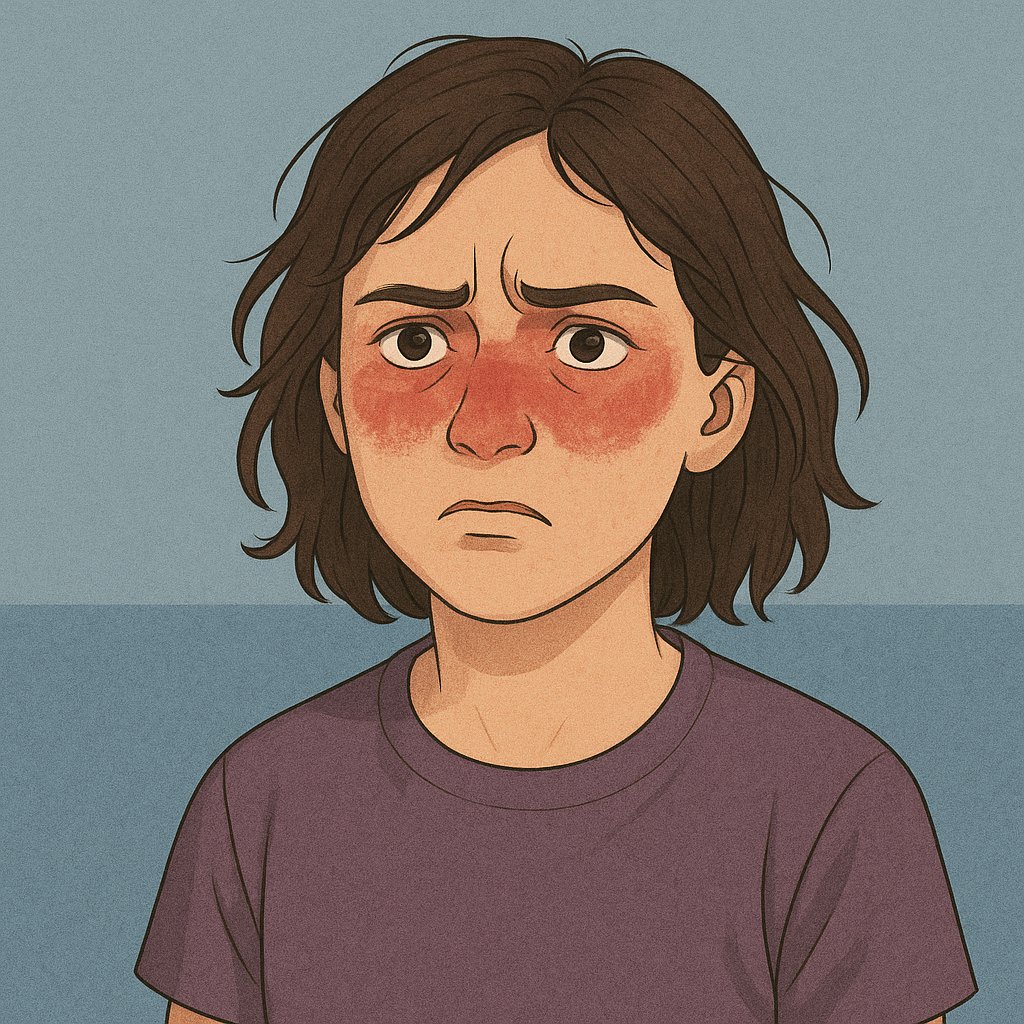
3/ Emotional dysregulation (ED) ≠ BPD by default
ED can be more common/severe in females with ADHD and overlaps with BPD; ED severity alone doesn’t distinguish the two.
💡 Psych Scene Tip: Take a developmental history and look for ADHD traits across settings.  
ED can be more common/severe in females with ADHD and overlaps with BPD; ED severity alone doesn’t distinguish the two.
💡 Psych Scene Tip: Take a developmental history and look for ADHD traits across settings.  
4/ Hyperactivity–impulsivity (H/I) looks different.
On average, girls show lower H/I severity than boys, with more subtle restlessness and impulsivity, which is one reason they’re missed. Meta-analyses and newer reviews converge on this signal. 
💡 Psych Scene Tip:
Screen for quiet hyperactivity: ask about leg-jiggling, hair-twirling, rapid speech, interrupting when excited, snap decisions, and “finding reasons to move” during long sits.
On average, girls show lower H/I severity than boys, with more subtle restlessness and impulsivity, which is one reason they’re missed. Meta-analyses and newer reviews converge on this signal. 
💡 Psych Scene Tip:
Screen for quiet hyperactivity: ask about leg-jiggling, hair-twirling, rapid speech, interrupting when excited, snap decisions, and “finding reasons to move” during long sits.
5/ Inattention: the giveaway.
Think “easily overwhelmed,” disorganised, task initiation problems, mental planning difficulties.
Item-level evidence highlights attentional symptoms as especially informative for detecting ADHD in females.
Think “easily overwhelmed,” disorganised, task initiation problems, mental planning difficulties.
Item-level evidence highlights attentional symptoms as especially informative for detecting ADHD in females.
6/ Hormones matter (across the lifespan).
Symptoms commonly fluctuate with the menstrual cycle and can change during pregnancy and perimenopause.
💡Psych Scene Tip: ask patients to track symptoms vs. cycle; consider timing meds/adjuncts accordingly.
Symptoms commonly fluctuate with the menstrual cycle and can change during pregnancy and perimenopause.
💡Psych Scene Tip: ask patients to track symptoms vs. cycle; consider timing meds/adjuncts accordingly.
7/ Comorbidities to actively screen for.
• Eating disorders: ADHD is linked to a higher risk across AN/BN/BED; effect sizes are clinically meaningful (bi-directional association). 
• Substance use: Elevated alcohol/cannabis risk; some data suggest females with ADHD (without other comorbidity) may have a higher risk than males. Ask early. 
• Eating disorders: ADHD is linked to a higher risk across AN/BN/BED; effect sizes are clinically meaningful (bi-directional association). 
• Substance use: Elevated alcohol/cannabis risk; some data suggest females with ADHD (without other comorbidity) may have a higher risk than males. Ask early. 
Clinician takeaway (save this):
Under-recognised internalising profiles + compensation → later diagnosis. Look for inattention/EF burden, subtle H/I, track hormones, and screen EDs/SUDs.
Under-recognised internalising profiles + compensation → later diagnosis. Look for inattention/EF burden, subtle H/I, track hormones, and screen EDs/SUDs.
From screening to nuanced management of female ADHD presentations, the Adult ADHD Clinical Training Program delivers case-based tools across diagnosis, pharmacotherapy, perinatal care, and ASD, click the link below to learn more:
psychscene.co/4fHBxLf
psychscene.co/4fHBxLf
• • •
Missing some Tweet in this thread? You can try to
force a refresh