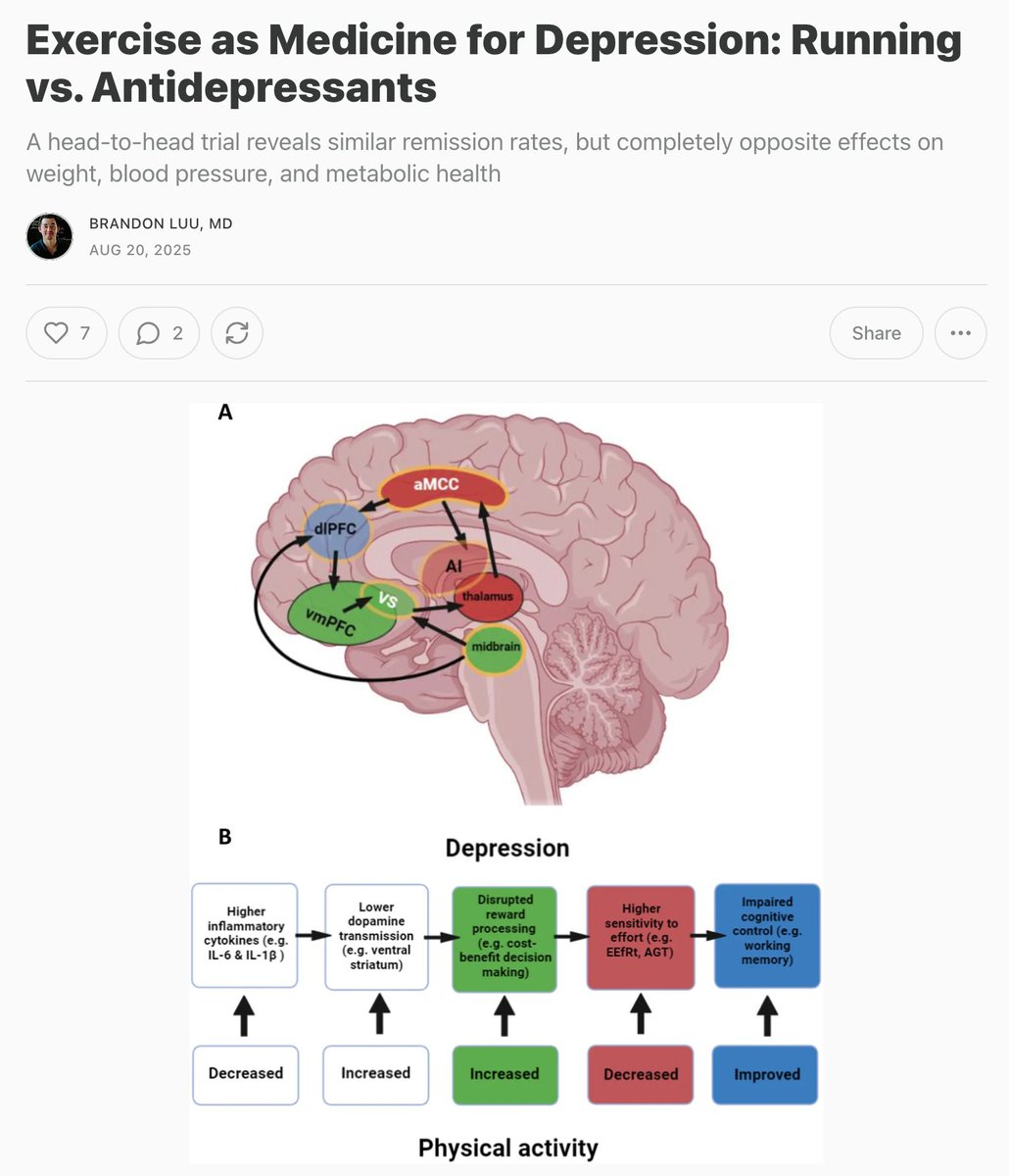
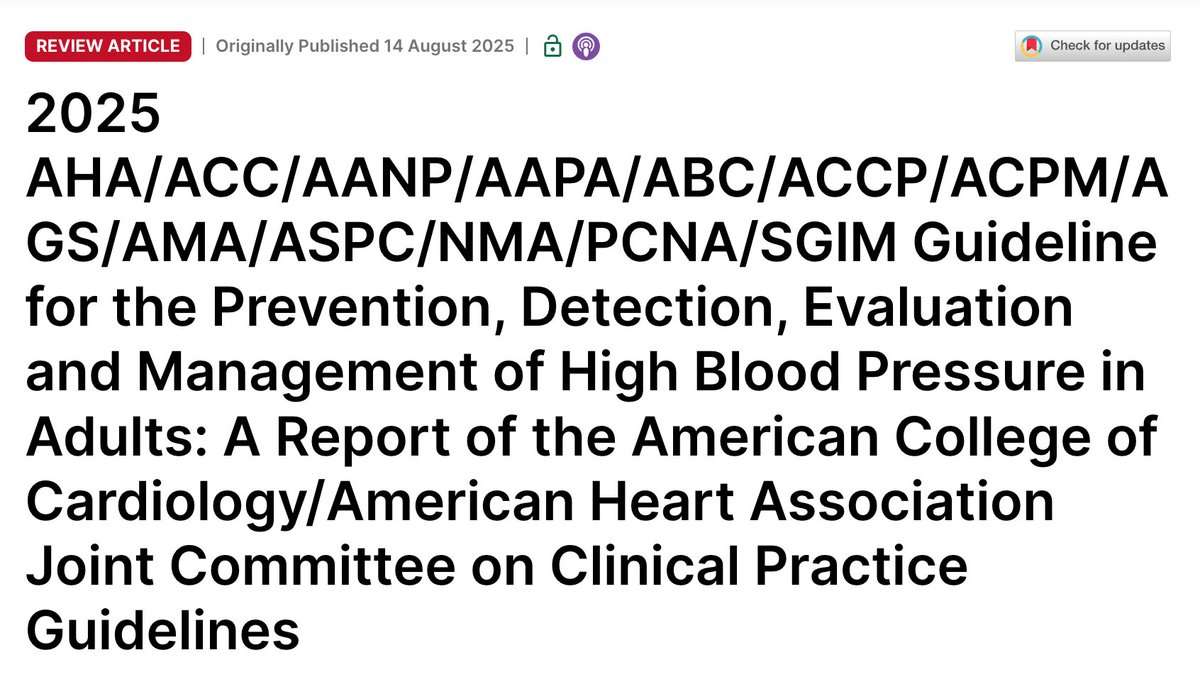
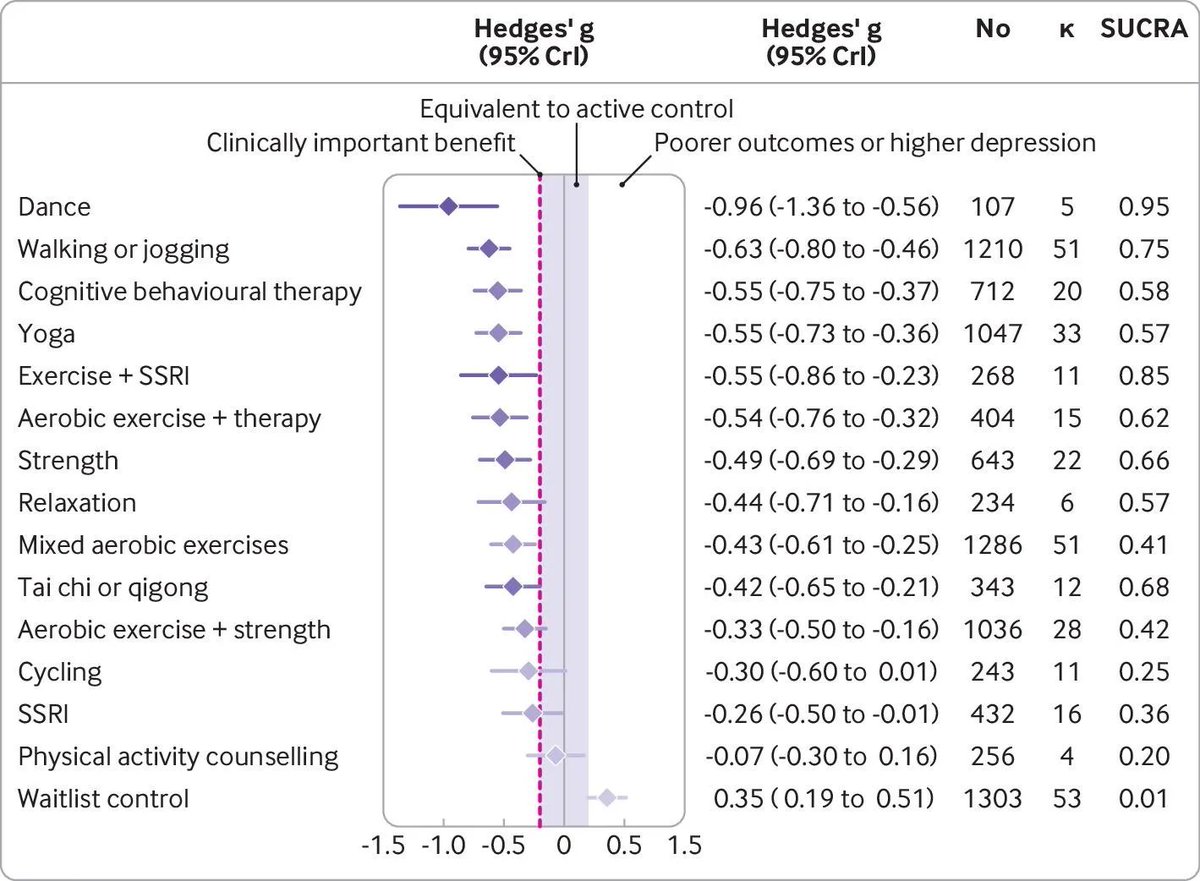
🏃 Head-to-head trial: Running therapy matches antidepressants (SSRIs) for depression remission
The catch: SSRIs worsened every metabolic marker measured
Running improved them all 🧵1/8
The catch: SSRIs worsened every metabolic marker measured
Running improved them all 🧵1/8

The MOTAR trial setup: 45 patients took escitalopram 10-20mg daily, 96 chose supervised running (45min outdoor sessions 2-3x/week)
Both groups allowed psychotherapy
After 16 weeks, mental health outcomes were identical, but metabolic health diverged dramatically /2
Both groups allowed psychotherapy
After 16 weeks, mental health outcomes were identical, but metabolic health diverged dramatically /2

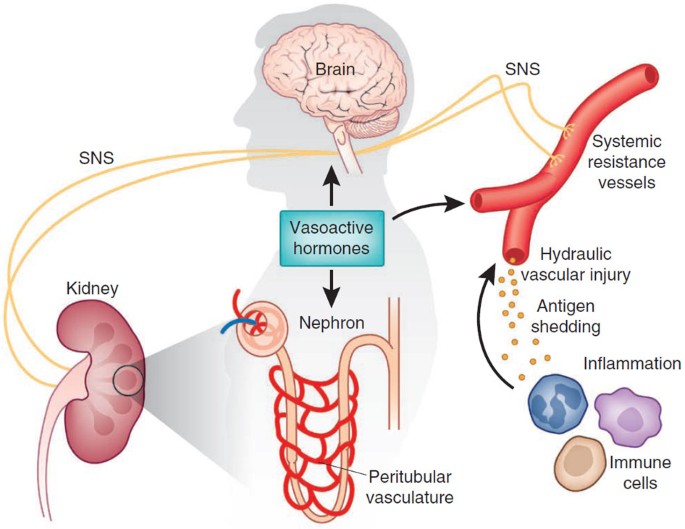
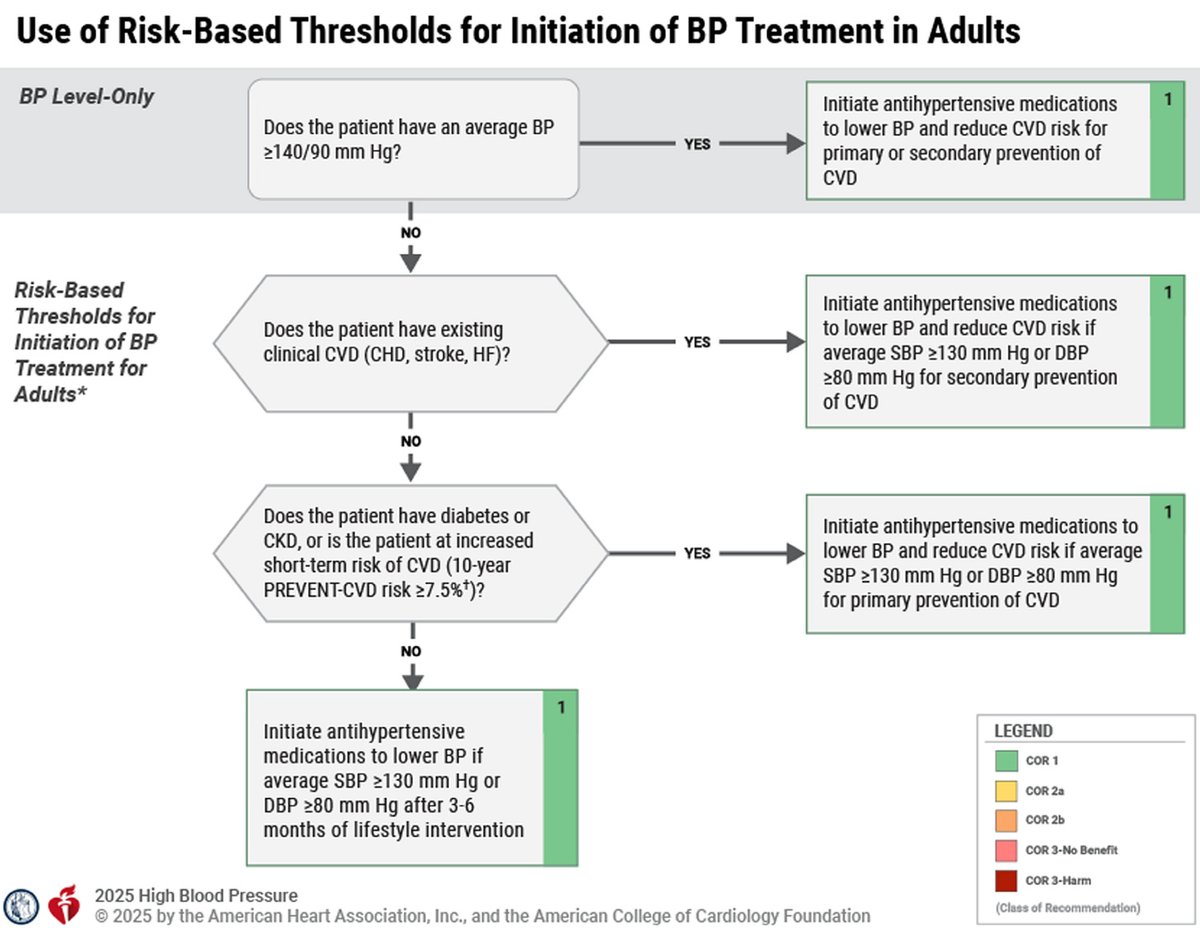
SSRI group gained 7.3 pounds, waist +1.5cm, blood pressure rose 3.8/1.9 mmHg Heart rate variability reduced -14.4ms (worse stress response) Inflammation marker CRP increased +1.5mg/L
The pills that fixed mood were harming metabolism /3
The pills that fixed mood were harming metabolism /3

Running group lost weight (-0.6kg), trimmed waist circumference (-1.6cm), dropped BP (-2.5/-2.9 mmHg)
Heart rate variability improved, resting pulse dropped -3.4bpm
Among adherent runners: VO₂max increased 2.9 ml/kg/min /4
Heart rate variability improved, resting pulse dropped -3.4bpm
Among adherent runners: VO₂max increased 2.9 ml/kg/min /4
The protocol:
Weeks 1-4 at 50-70% heart rate reserve (can speak full sentences)
Weeks 5-16 at 70-85% HRR (only short phrases possible) 10min warmup + 30min main effort + 5min cooldown /5
Weeks 1-4 at 50-70% heart rate reserve (can speak full sentences)
Weeks 5-16 at 70-85% HRR (only short phrases possible) 10min warmup + 30min main effort + 5min cooldown /5
Only 52% of runners completed ≥22 sessions vs 82% medication compliance
15% assigned to running never even started
Yet running STILL matched SSRI effectiveness despite low adherence
Imagine if we solved the adherence and motivation puzzle /6
15% assigned to running never even started
Yet running STILL matched SSRI effectiveness despite low adherence
Imagine if we solved the adherence and motivation puzzle /6
In summary, running therapy had similar remission rates for depression and anxiety while every metabolic marker improved in the opposite direction of SSRIs, adding to a growing body of research about the benefits of exercise on mental health /7 
• • •
Missing some Tweet in this thread? You can try to
force a refresh