🧵 Drug vs Disease — When Side Effects Mimic the Diagnosis👇
Is it the disease—or the drug? Many “flares” are actually medication effects. Here’s a clinic-ready guide to the most common drug–disease confusions, what to check, and how to pivot fast. Save and share. #MedTwitter #RheumTwitter #FOAMed #IMTwitter #PrimaryCare #PatientSafety @IhabFathiSulima @DrAkhilX @Janetbirdope
Is it the disease—or the drug? Many “flares” are actually medication effects. Here’s a clinic-ready guide to the most common drug–disease confusions, what to check, and how to pivot fast. Save and share. #MedTwitter #RheumTwitter #FOAMed #IMTwitter #PrimaryCare #PatientSafety @IhabFathiSulima @DrAkhilX @Janetbirdope
Post 1
Big idea
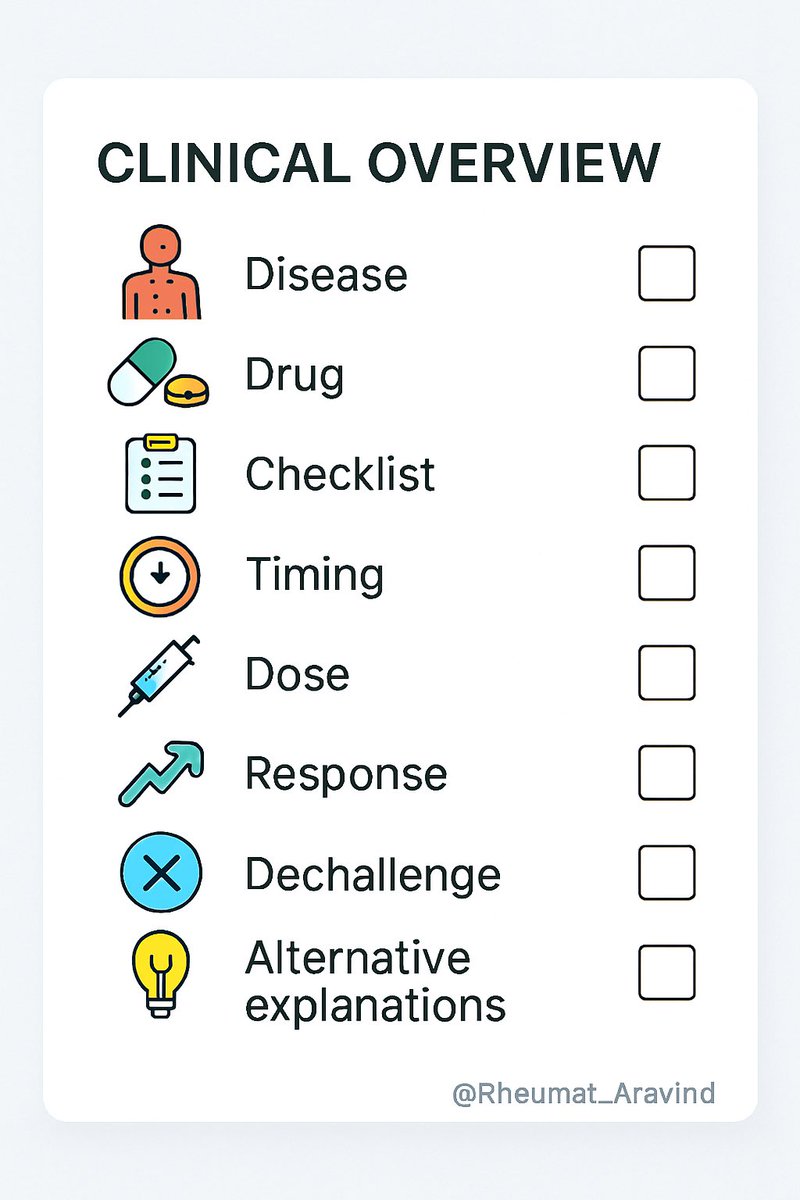
Before escalating therapy, ask: could the medication be causing or unmasking the symptom? Use this checklist: timing vs start/dose change, dose–response, dechallenge/rechallenge, and alternative explanations.
Big idea
Before escalating therapy, ask: could the medication be causing or unmasking the symptom? Use this checklist: timing vs start/dose change, dose–response, dechallenge/rechallenge, and alternative explanations.
Post 2
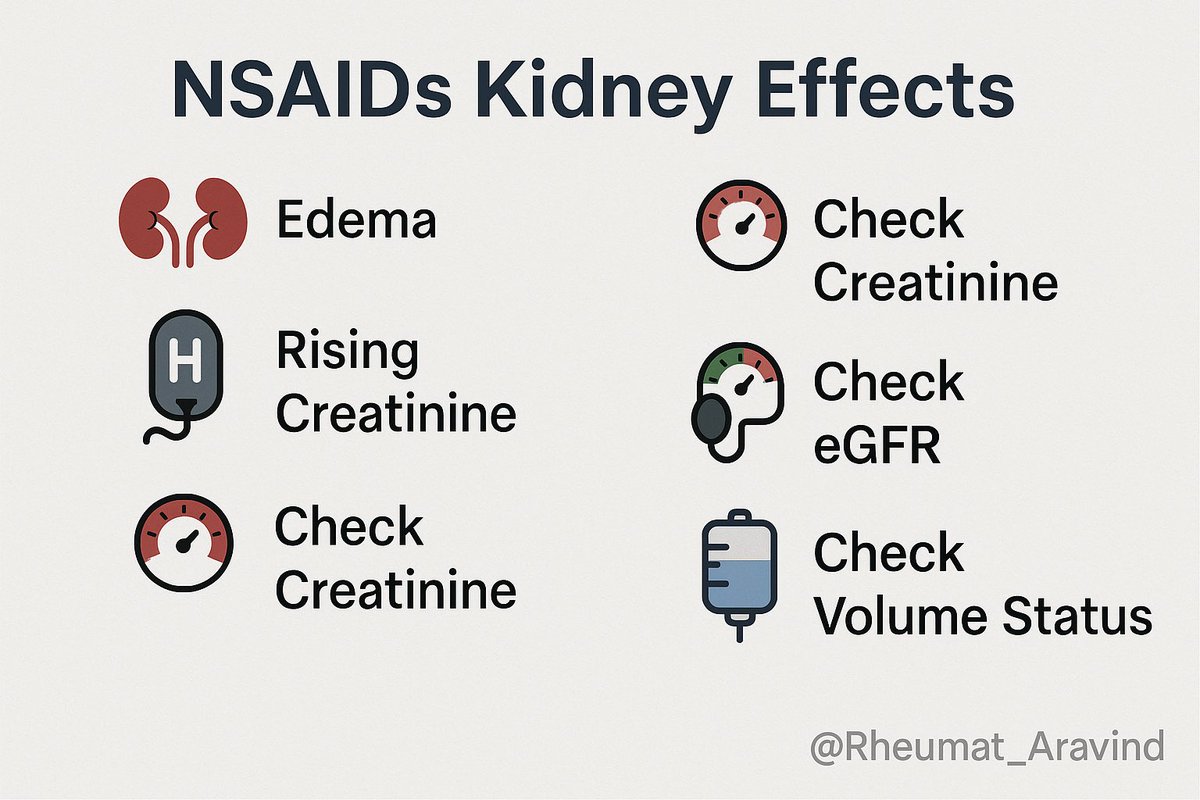
NSAIDs vs kidney/pressure
•Looks like: edema, rising creatinine, “worsening gout/OA pain”
•Could be: NSAID nephrotoxicity or hypertension
•Check: creatinine/eGFR, BP, volume status; step down NSAID, switch to topical or COX-2 cautiously; renal-safe analgesia plan.
NSAIDs vs kidney/pressure
•Looks like: edema, rising creatinine, “worsening gout/OA pain”
•Could be: NSAID nephrotoxicity or hypertension
•Check: creatinine/eGFR, BP, volume status; step down NSAID, switch to topical or COX-2 cautiously; renal-safe analgesia plan.
Post 3
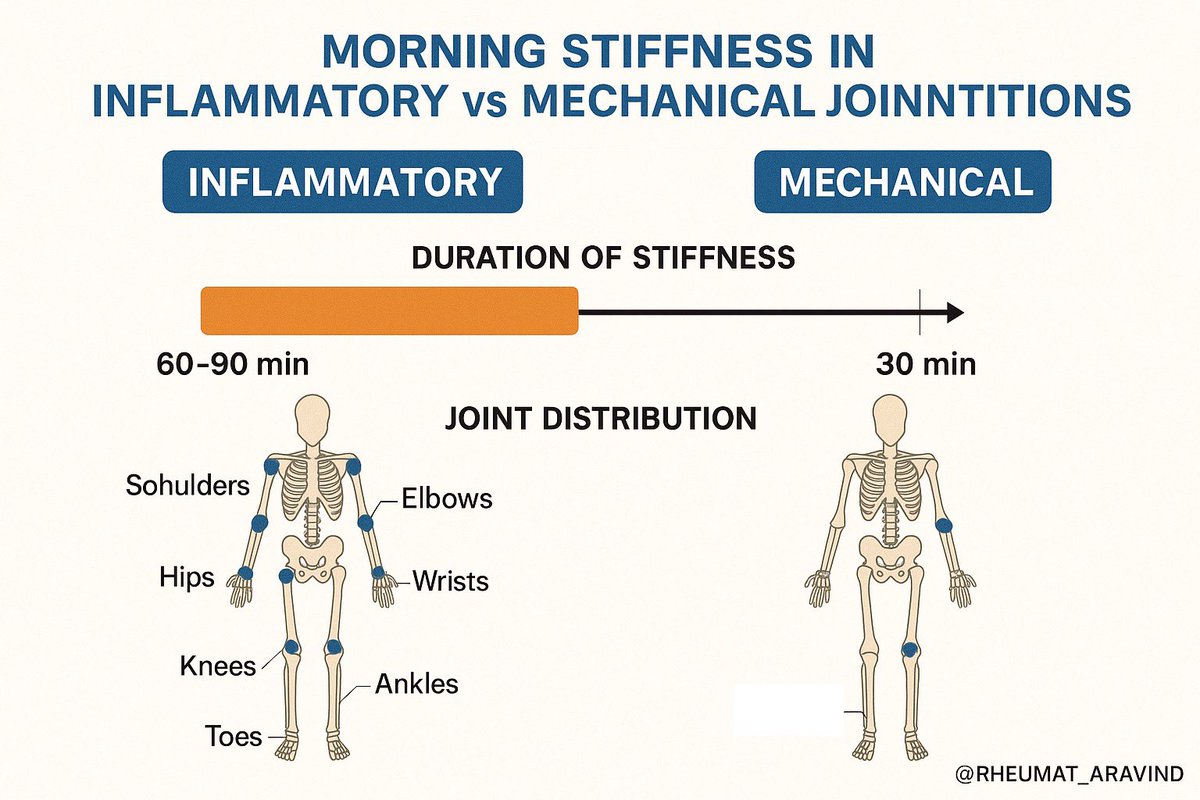
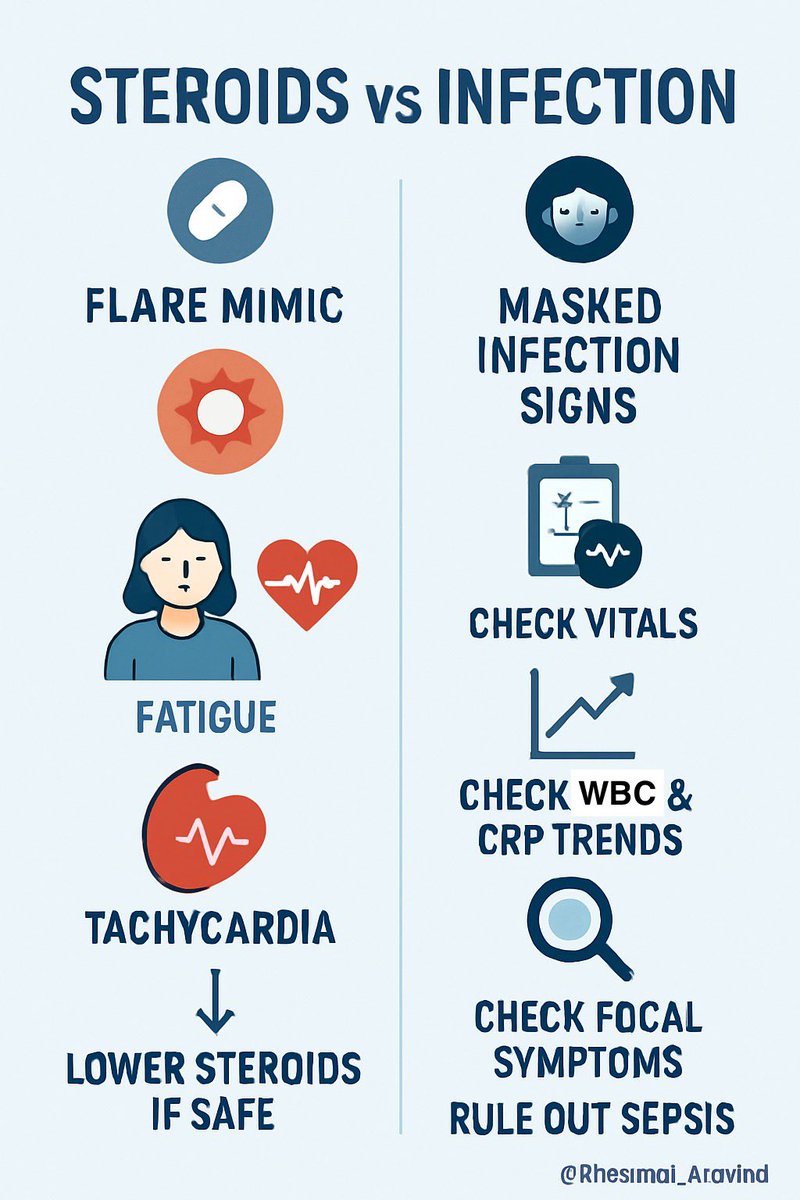
Steroids vs infection
•Looks like: “rheum flare” with fatigue, tachycardia
•Could be: masked infection on steroids
•Check: vitals, WBC, CRP trend (can be blunted), focal symptoms; lower steroid if safe; rule out sepsis before increasing.
Steroids vs infection
•Looks like: “rheum flare” with fatigue, tachycardia
•Could be: masked infection on steroids
•Check: vitals, WBC, CRP trend (can be blunted), focal symptoms; lower steroid if safe; rule out sepsis before increasing.
Post 4
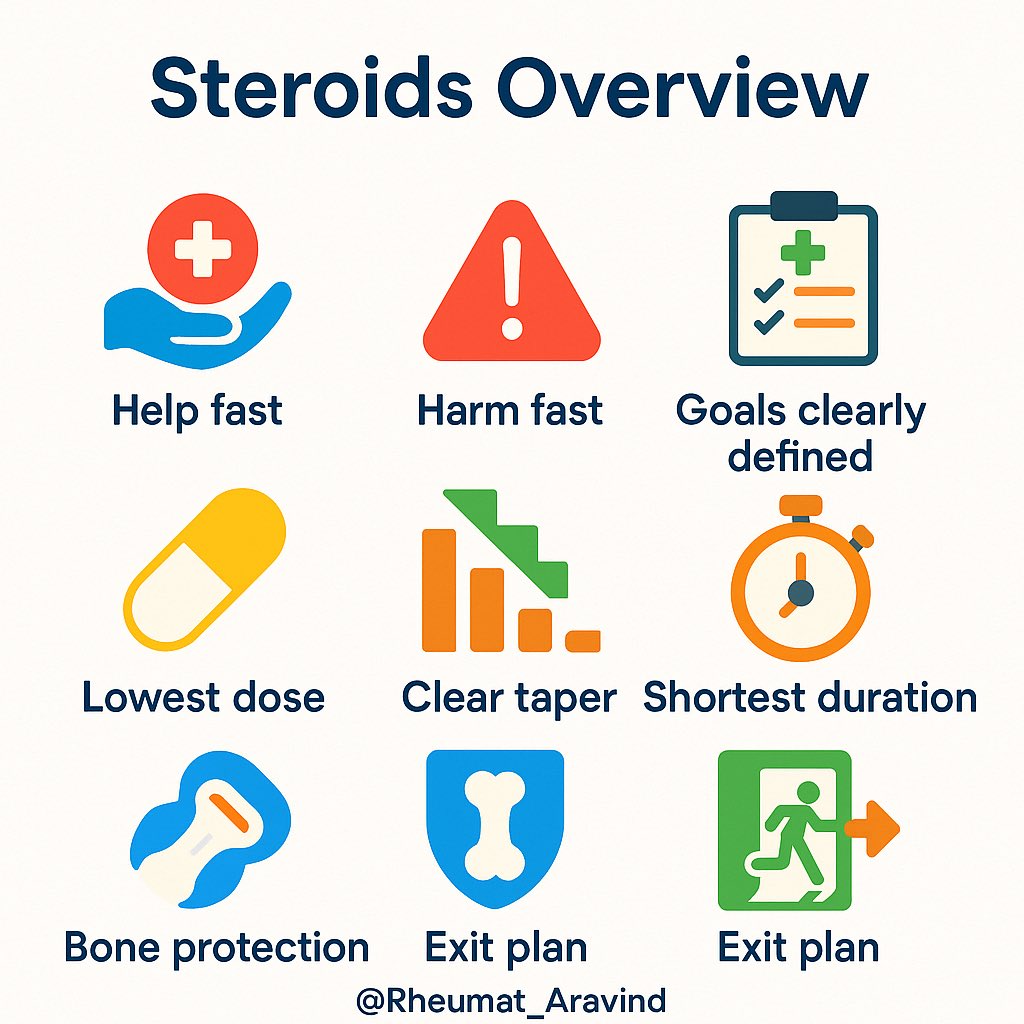
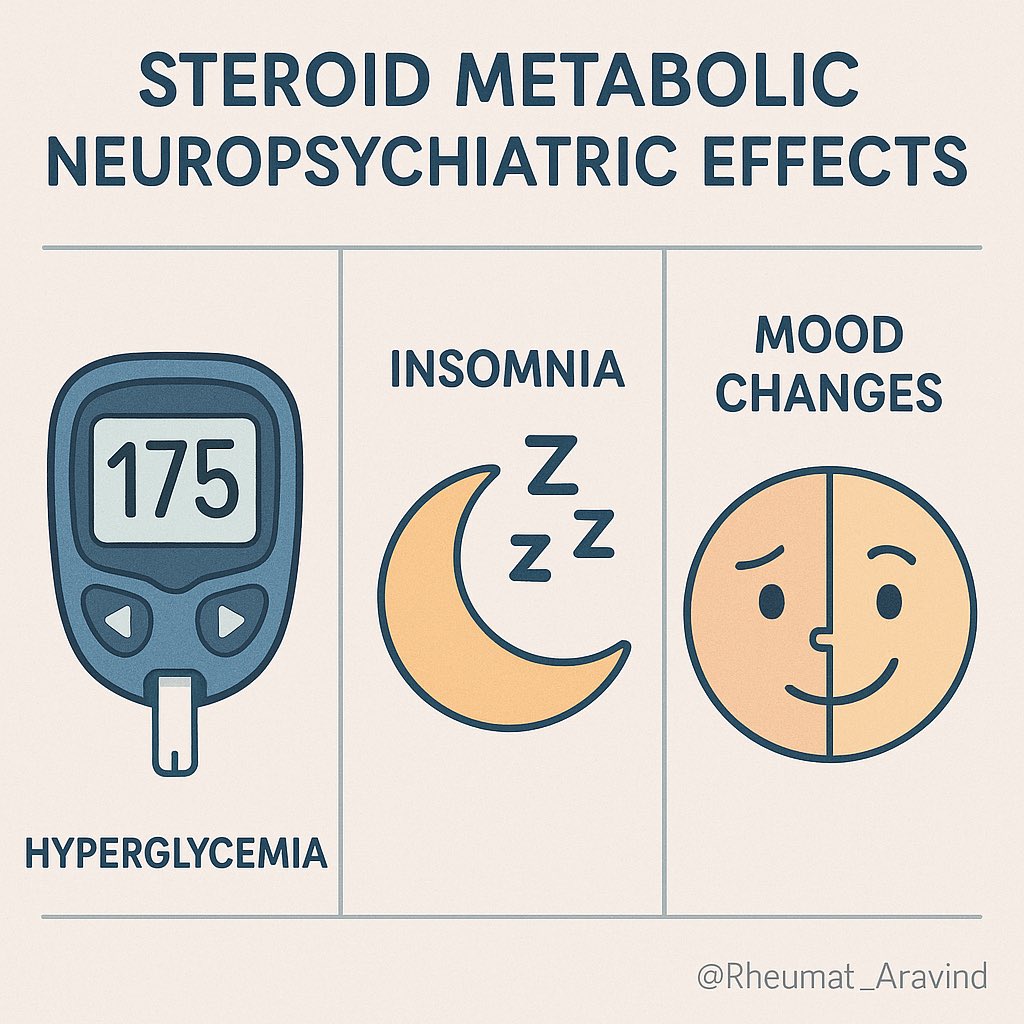
Steroids vs diabetes/mood/sleep
•Looks like: “new inflammatory pain, poor sleep, anxiety”
•Could be: steroid-induced hyperglycemia, insomnia, mood change
•Check: fasting/random glucose, sleep/mood screen; morning dosing, taper where possible, brief sleep aids, consider steroid-sparing plan.
Steroids vs diabetes/mood/sleep
•Looks like: “new inflammatory pain, poor sleep, anxiety”
•Could be: steroid-induced hyperglycemia, insomnia, mood change
•Check: fasting/random glucose, sleep/mood screen; morning dosing, taper where possible, brief sleep aids, consider steroid-sparing plan.
Post 5
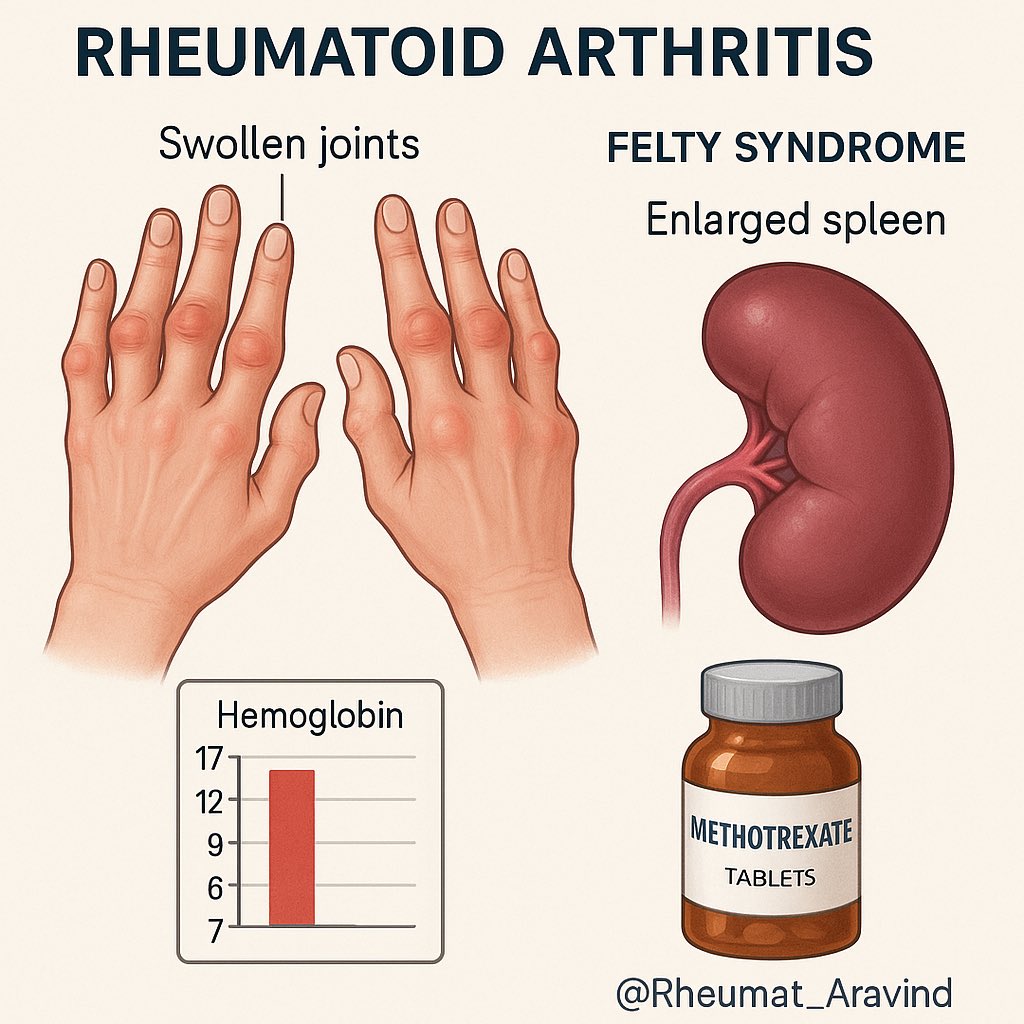
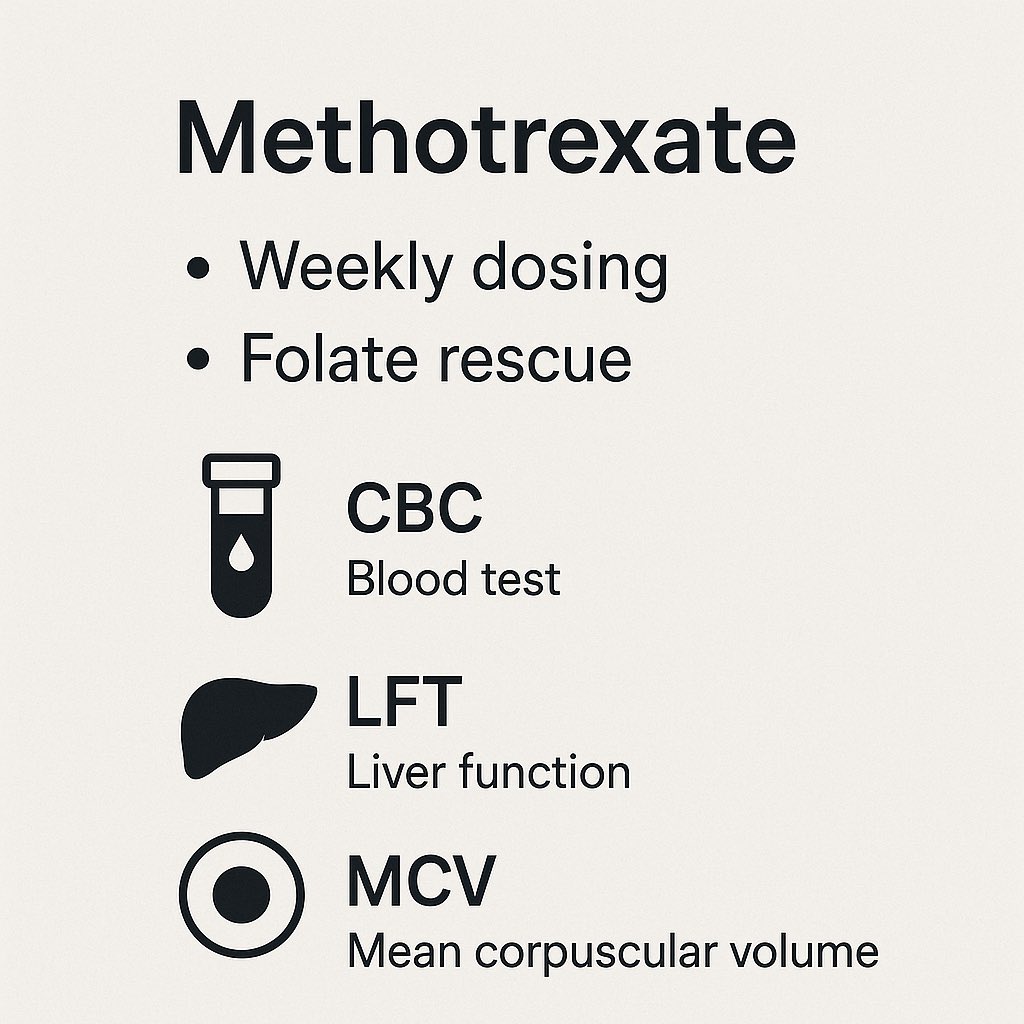
Methotrexate vs disease fatigue
•Looks like: persistent fatigue, nausea, mouth soreness “despite control”
•Could be: MTX intolerance or cytopenia
•Check: CBC, LFTs, MCV; confirm weekly dosing; optimize folate/folinic acid; consider SC MTX or switch.
Methotrexate vs disease fatigue
•Looks like: persistent fatigue, nausea, mouth soreness “despite control”
•Could be: MTX intolerance or cytopenia
•Check: CBC, LFTs, MCV; confirm weekly dosing; optimize folate/folinic acid; consider SC MTX or switch.
Post 6
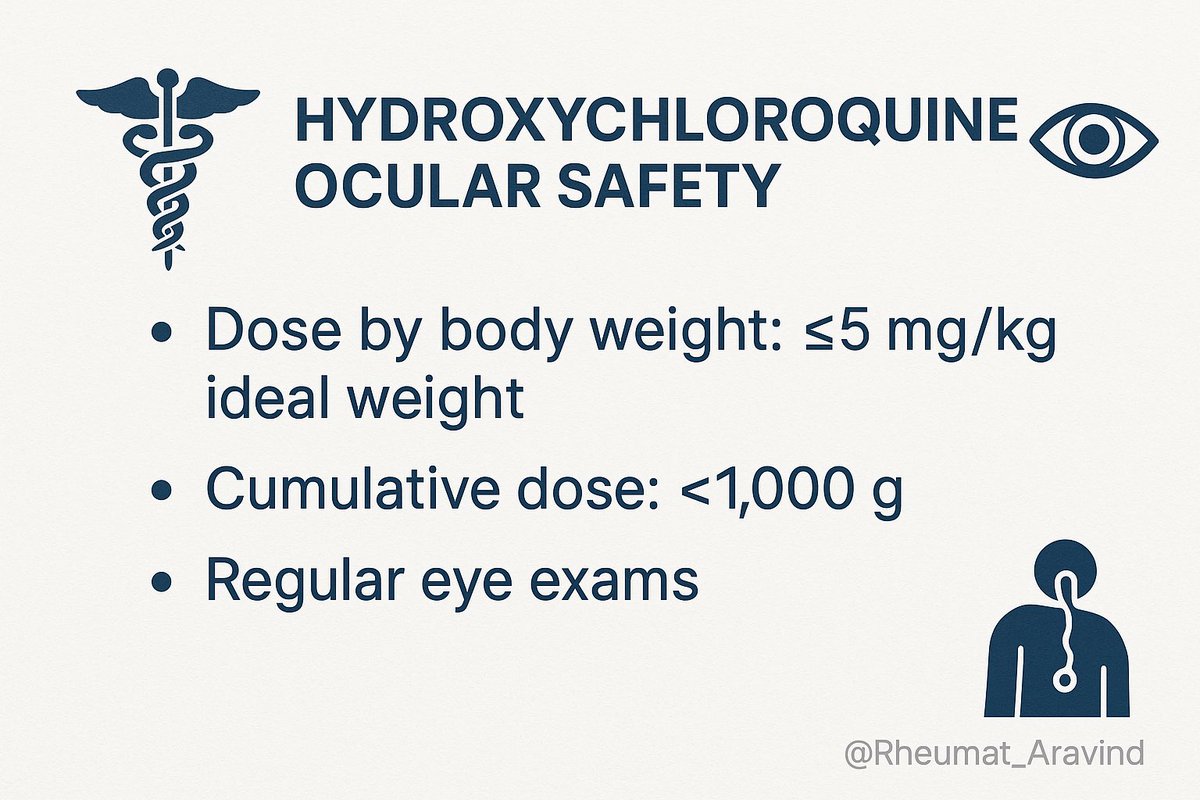
Hydroxychloroquine vs vision complaints
•Looks like: “ocular flare” or headache
•Could be: HCQ toxicity (rare early but risk accumulates)
•Check: dose by actual body weight, cumulative dose, baseline/periodic ocular exams; if visual symptoms, urgent ophthalmology.
Hydroxychloroquine vs vision complaints
•Looks like: “ocular flare” or headache
•Could be: HCQ toxicity (rare early but risk accumulates)
•Check: dose by actual body weight, cumulative dose, baseline/periodic ocular exams; if visual symptoms, urgent ophthalmology.
Post 7
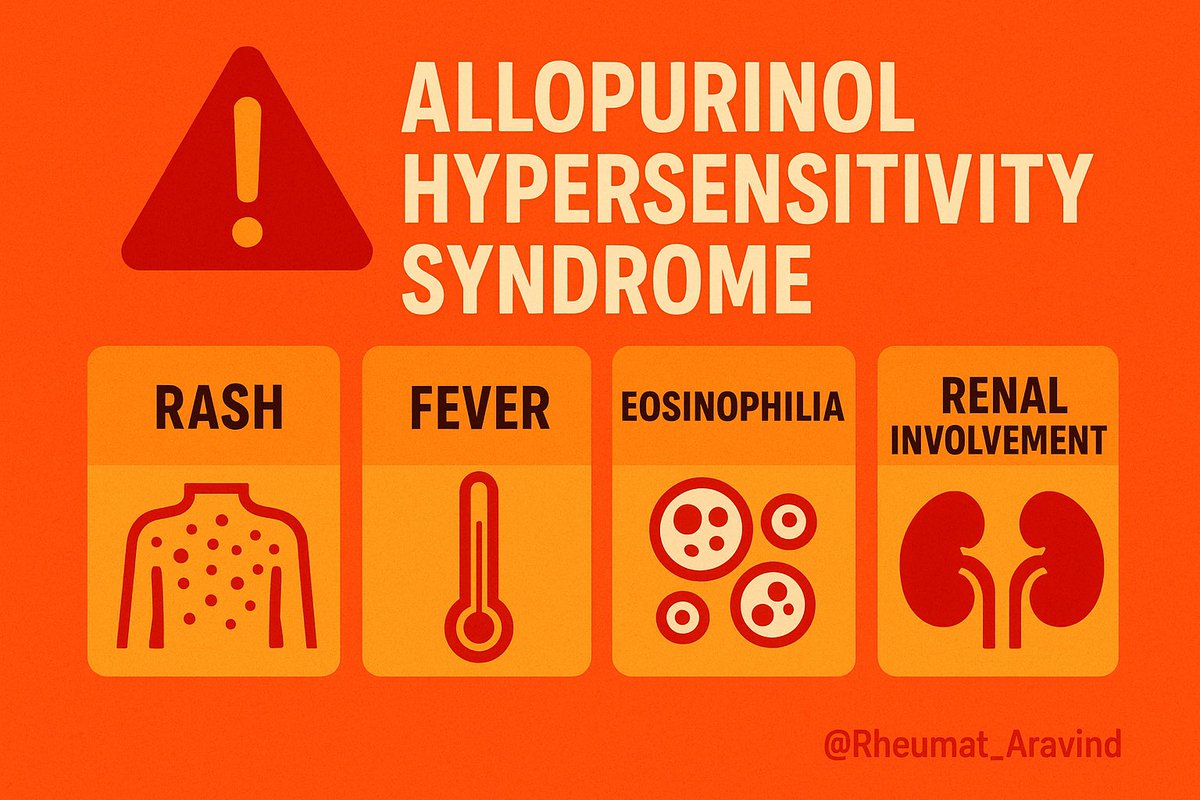
Allopurinol vs “gout rash”
•Looks like: flare plus rash after ULT start
•Could be: hypersensitivity (watch for fever, eosinophilia, renal involvement)
•Check: timeline to start, skin exam, labs; stop drug and escalate care if systemic features; consider HLA-B*58:01 in high-risk groups where recommended.
Allopurinol vs “gout rash”
•Looks like: flare plus rash after ULT start
•Could be: hypersensitivity (watch for fever, eosinophilia, renal involvement)
•Check: timeline to start, skin exam, labs; stop drug and escalate care if systemic features; consider HLA-B*58:01 in high-risk groups where recommended.
Post 8
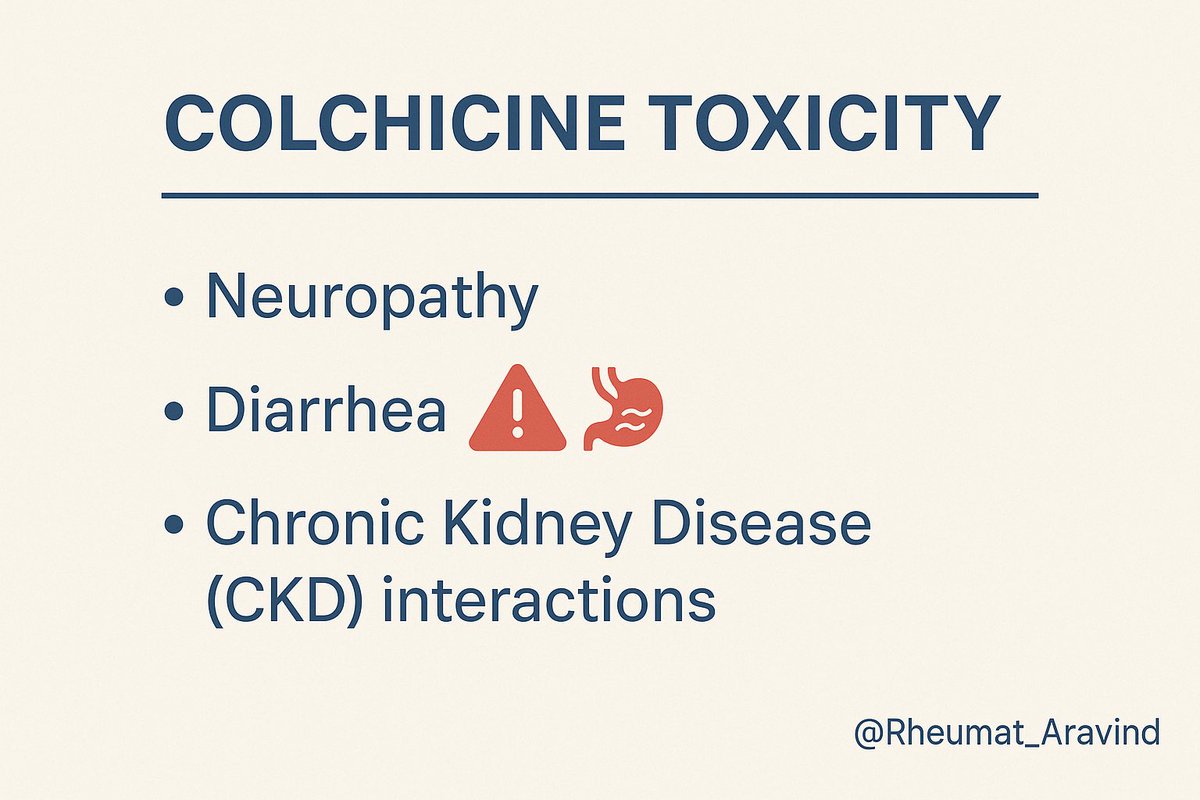
Colchicine vs neuropathy/diarrhea
•Looks like: “worsening enthesitis pain” with leg weakness
•Could be: colchicine toxicity (especially with CKD or interacting CYP3A4/P-gp drugs)
•Check: CK, neuro exam, meds for interactions; dose-adjust or stop; educate on early GI signs.
Colchicine vs neuropathy/diarrhea
•Looks like: “worsening enthesitis pain” with leg weakness
•Could be: colchicine toxicity (especially with CKD or interacting CYP3A4/P-gp drugs)
•Check: CK, neuro exam, meds for interactions; dose-adjust or stop; educate on early GI signs.
Post 9
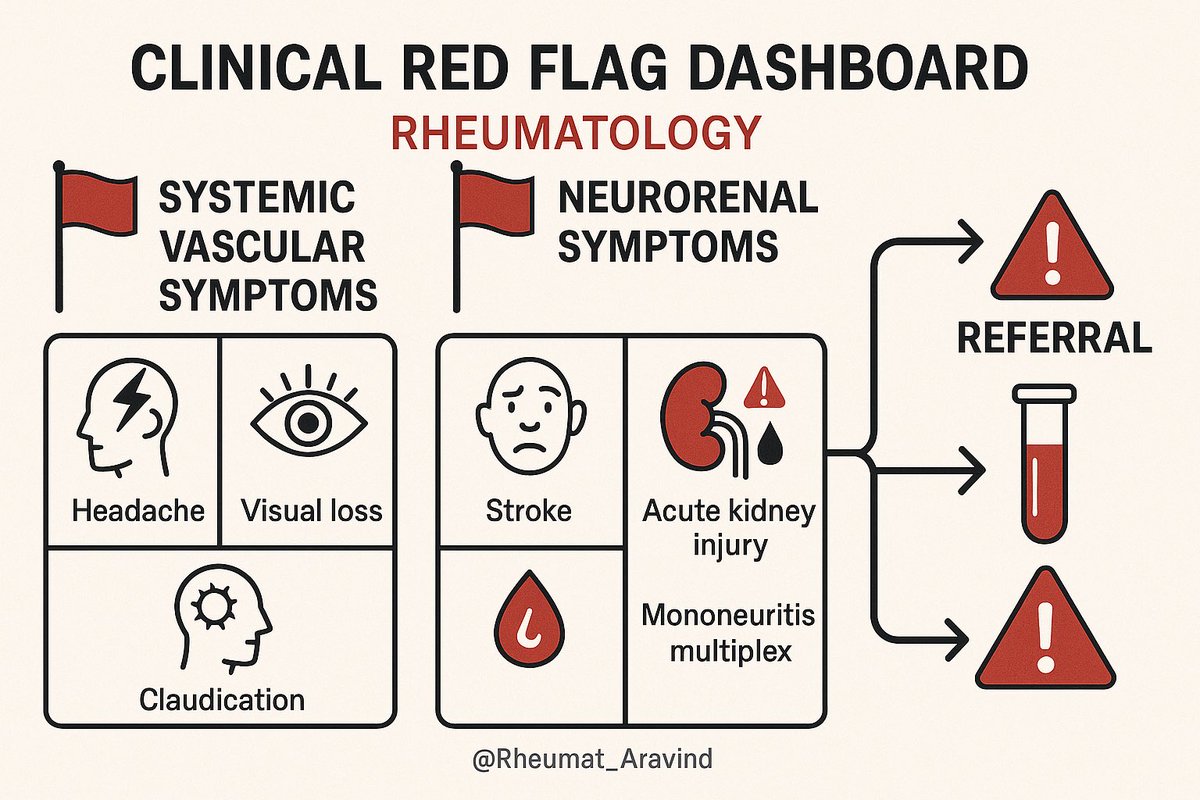
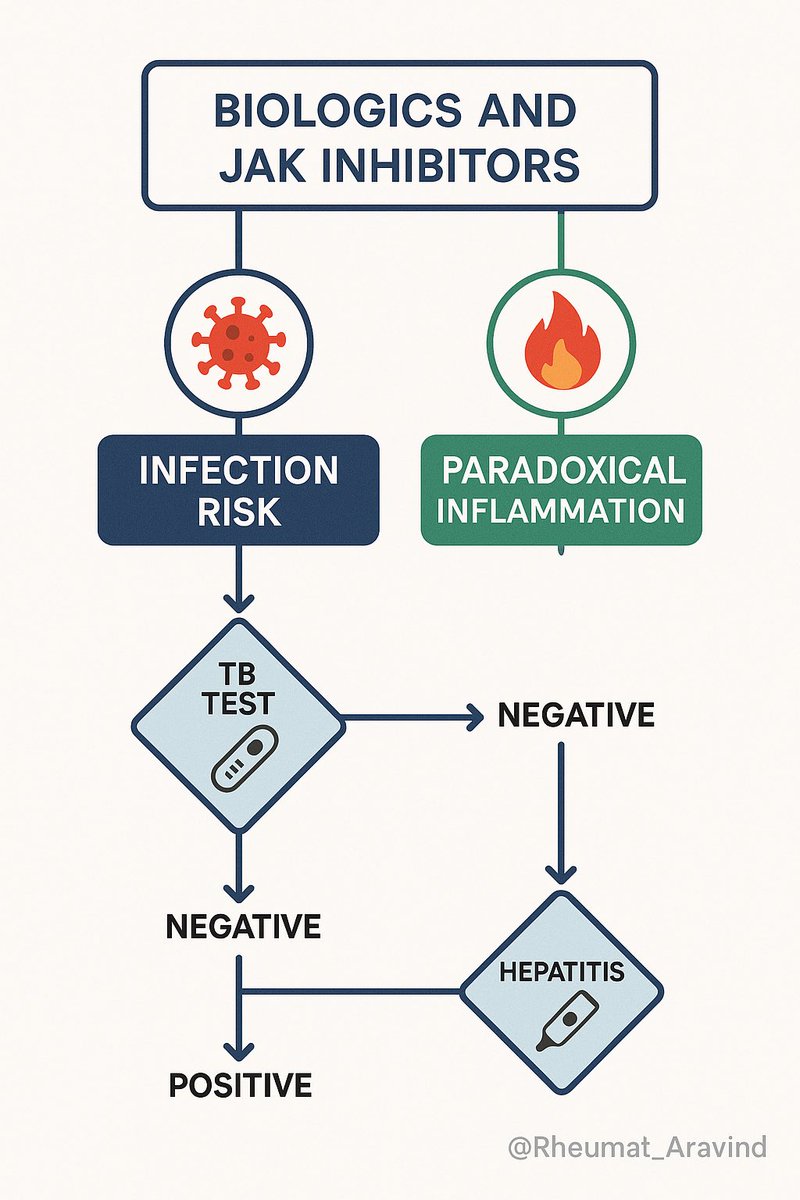
Biologics/JAKi vs infection or paradoxical inflammation
•Looks like: “psoriasis flare” on anti-TNF, “cough/fever” on therapy
•Could be: paradoxical skin disease; opportunistic infection
•Check: TB/hepatitis screening status, CRP, CXR if respiratory; dermatology/rheum plan—switch class if paradoxical.
Biologics/JAKi vs infection or paradoxical inflammation
•Looks like: “psoriasis flare” on anti-TNF, “cough/fever” on therapy
•Could be: paradoxical skin disease; opportunistic infection
•Check: TB/hepatitis screening status, CRP, CXR if respiratory; dermatology/rheum plan—switch class if paradoxical.
Post 10
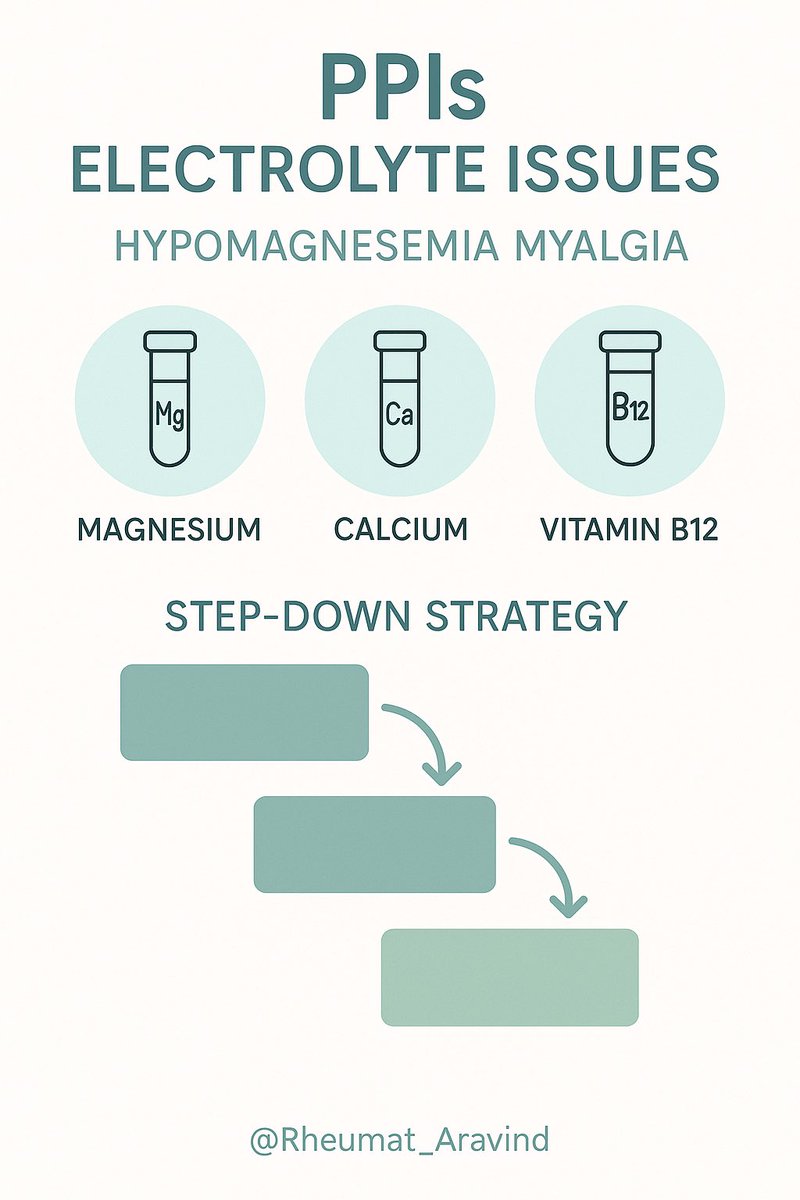
PPIs vs hypomagnesemia/myalgia
•Looks like: diffuse aches “not improving with DMARDs”
•Could be: electrolyte disturbance from chronic PPI
•Check: Mg2+, Ca2+, vitamin B12 if long-term; step-down strategy or alternate GI protection if appropriate.
PPIs vs hypomagnesemia/myalgia
•Looks like: diffuse aches “not improving with DMARDs”
•Could be: electrolyte disturbance from chronic PPI
•Check: Mg2+, Ca2+, vitamin B12 if long-term; step-down strategy or alternate GI protection if appropriate.
Post 11
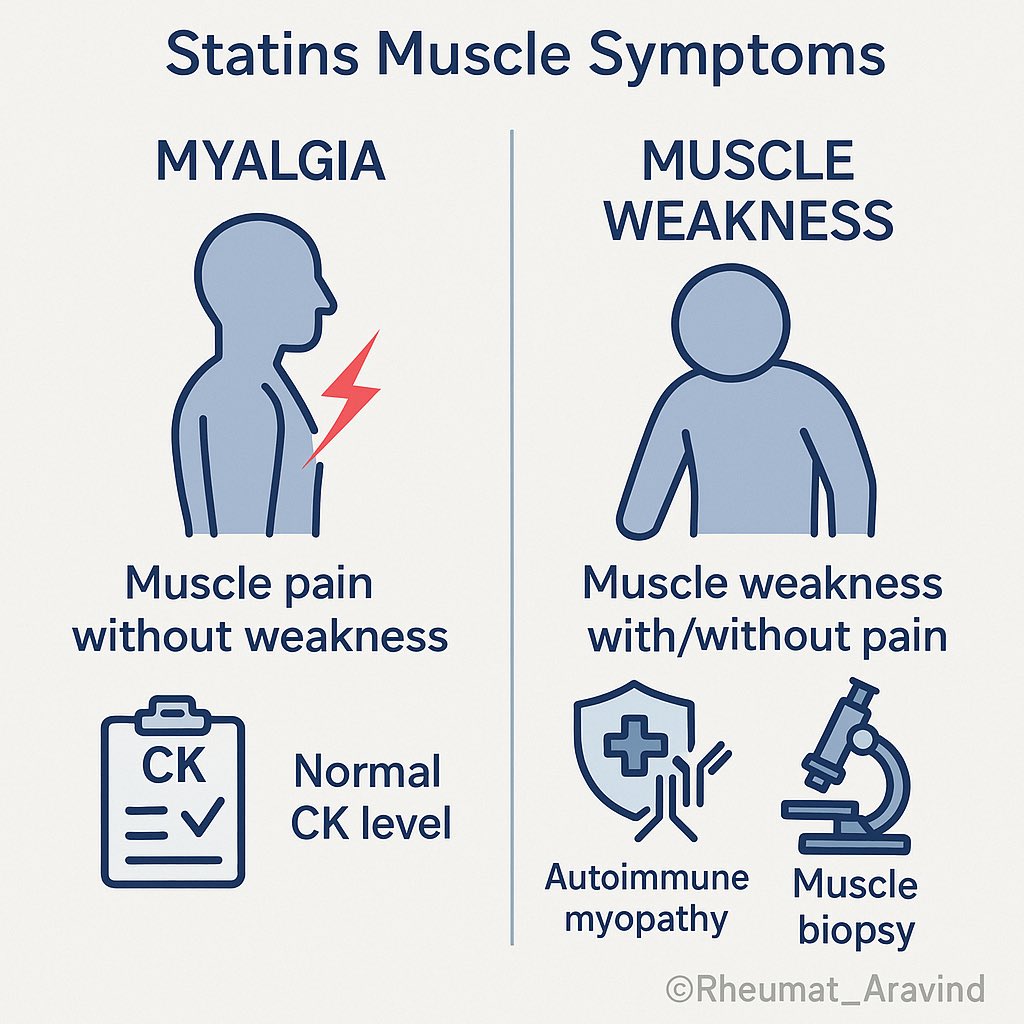
Statins vs myopathy vs myositis
•Looks like: “polymyalgia” or proximal weakness
•Could be: statin myopathy or rare statin-associated autoimmune myopathy
•Check: CK, pattern (pain vs weakness), temporal relation; stop statin trial, consider alternate lipid therapy; if severe weakness/high CK, evaluate for SAAM.
Statins vs myopathy vs myositis
•Looks like: “polymyalgia” or proximal weakness
•Could be: statin myopathy or rare statin-associated autoimmune myopathy
•Check: CK, pattern (pain vs weakness), temporal relation; stop statin trial, consider alternate lipid therapy; if severe weakness/high CK, evaluate for SAAM.
Post 12
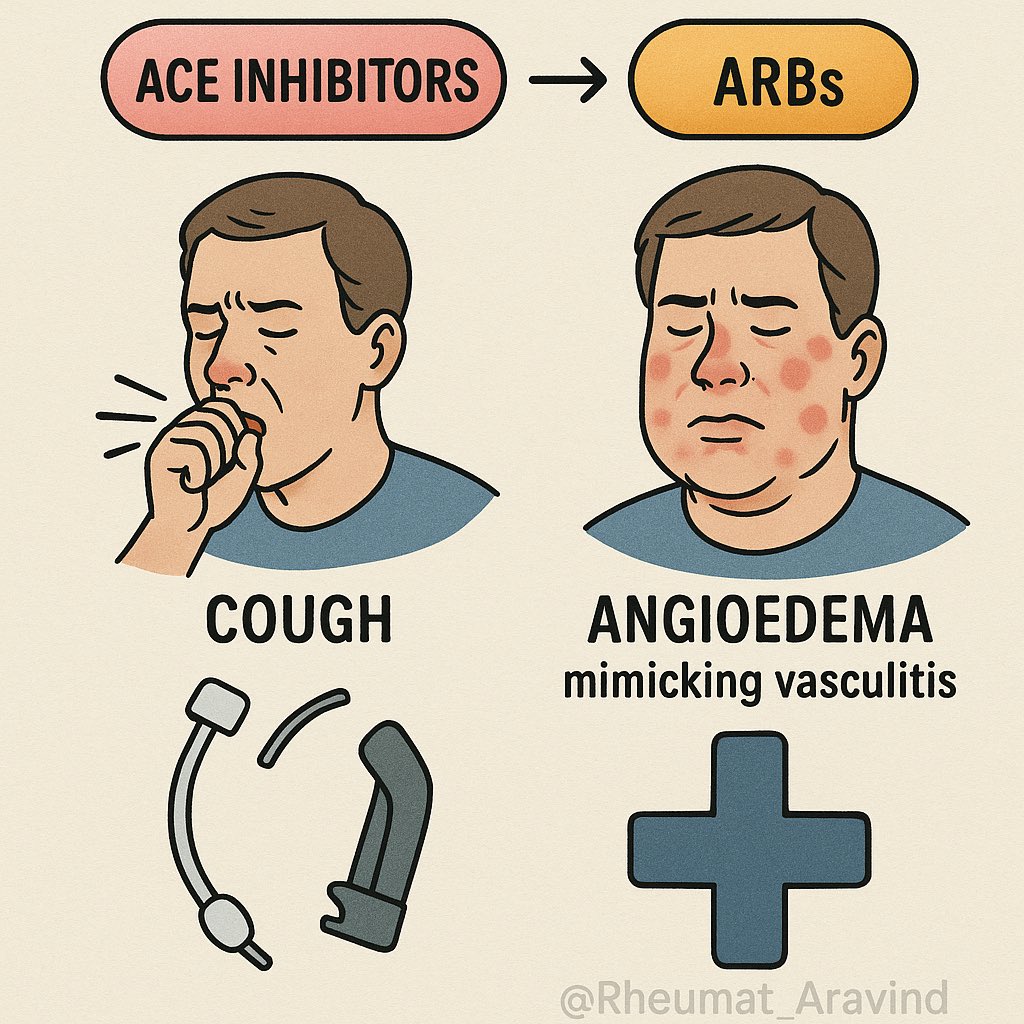
ACEi/ARBs vs cough/angioedema mimicking vasculitis
•Looks like: chronic cough/airway symptoms
•Could be: ACEi cough or rare angioedema
•Check: drug list and timing; switch class; reassess before extensive vasculitis workup.
ACEi/ARBs vs cough/angioedema mimicking vasculitis
•Looks like: chronic cough/airway symptoms
•Could be: ACEi cough or rare angioedema
•Check: drug list and timing; switch class; reassess before extensive vasculitis workup.
Post 13
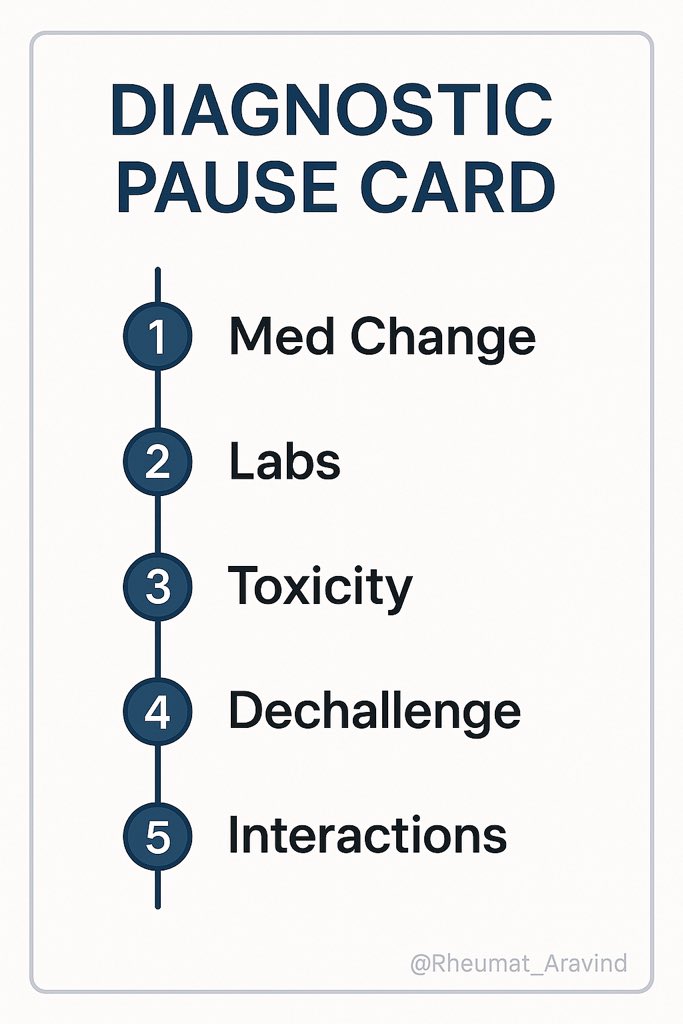
Diagnostic pause card
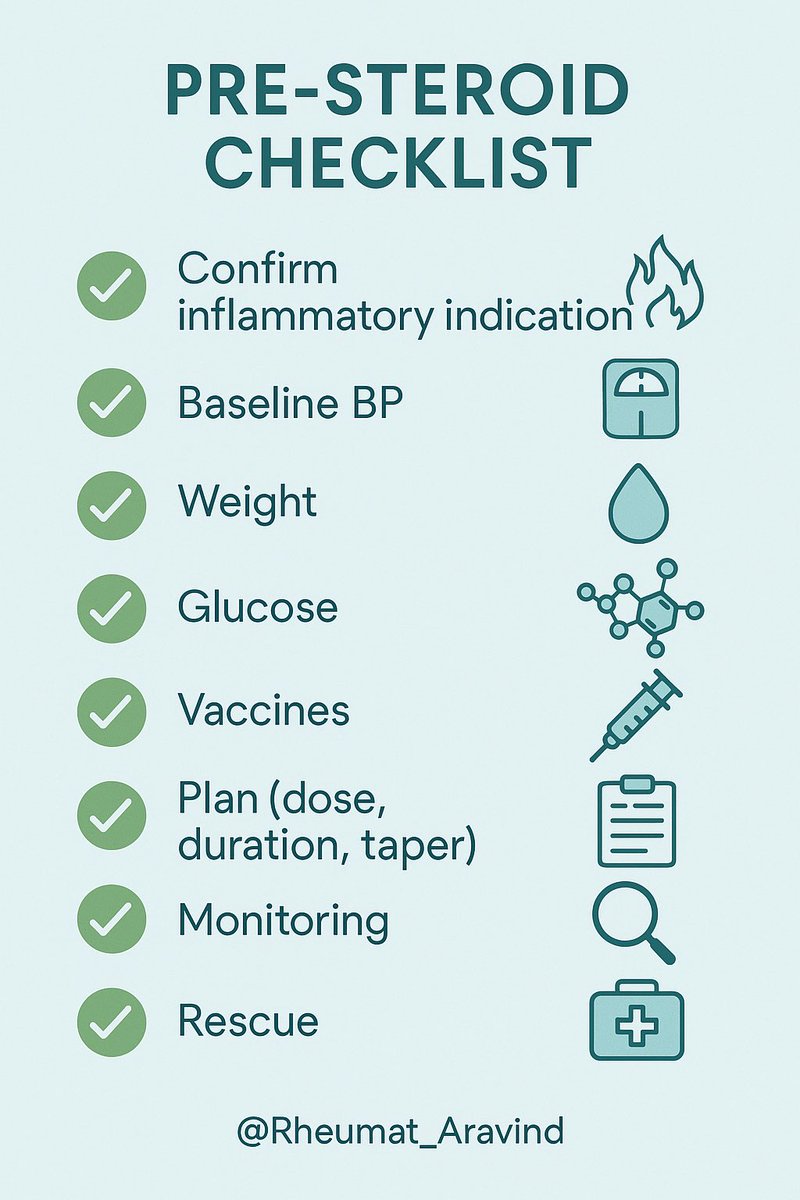
Before increasing immunosuppression, run the 5 checks:
1.Timeline to med change
2.Lab signal fits drug toxicity?
3.Dechallenge feasible?
4.Interactions/organ function reviewed?
5.A single test to clarify? (e.g., CK, UA, CXR)
Diagnostic pause card
Before increasing immunosuppression, run the 5 checks:
1.Timeline to med change
2.Lab signal fits drug toxicity?
3.Dechallenge feasible?
4.Interactions/organ function reviewed?
5.A single test to clarify? (e.g., CK, UA, CXR)
Post 14
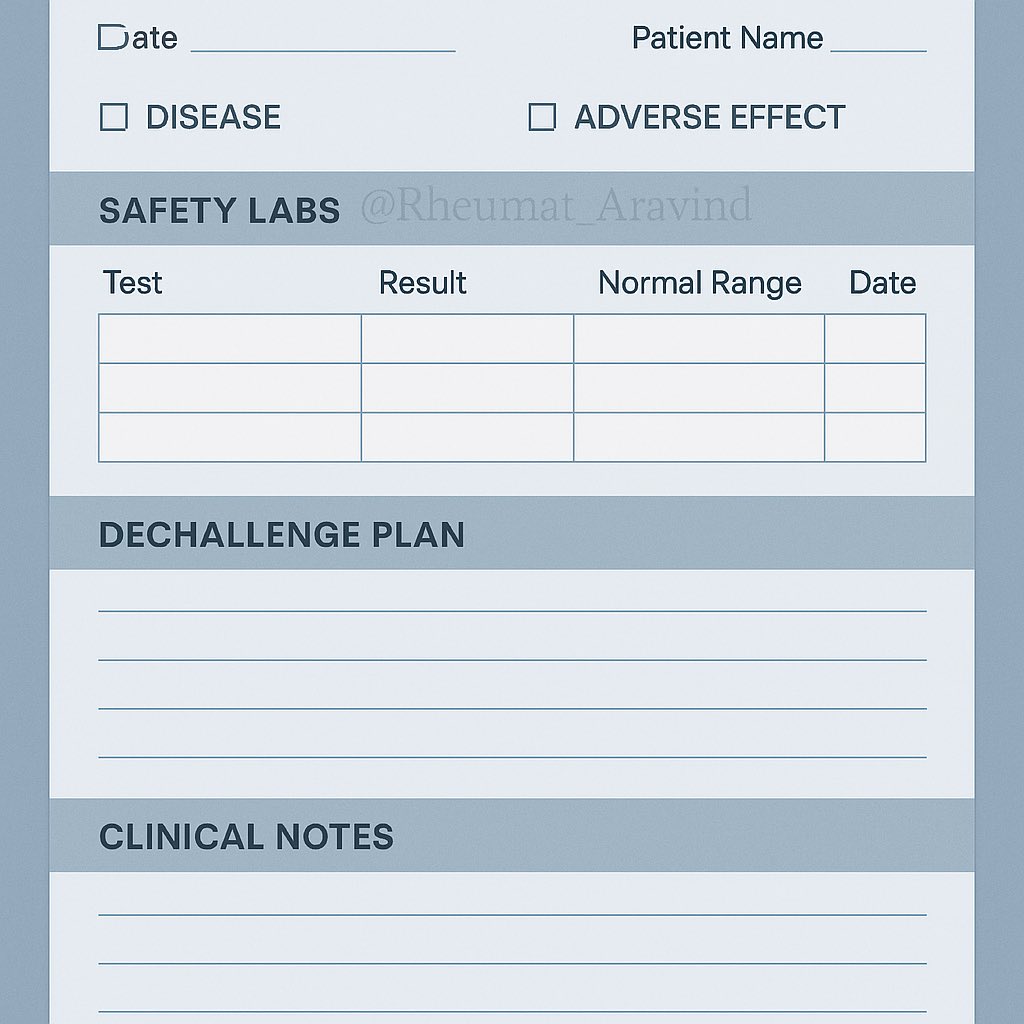
What to document
•Working differential (disease activity vs adverse effect)
•Safety labs and thresholds
•Proposed dechallenge/rechallenge plan
•Patient counseling and red-flag symptoms
•Exact follow-up date/window
What to document
•Working differential (disease activity vs adverse effect)
•Safety labs and thresholds
•Proposed dechallenge/rechallenge plan
•Patient counseling and red-flag symptoms
•Exact follow-up date/window
Post 15
Shareable takeaways
•Not every “flare” is the disease.
•Start low, go slow, review often.
•One quick lab or med switch can prevent months of overtreatment.
Shareable takeaways
•Not every “flare” is the disease.
•Start low, go slow, review often.
•One quick lab or med switch can prevent months of overtreatment.
• • •
Missing some Tweet in this thread? You can try to
force a refresh