What if your patient’s biggest struggle isn’t the thought, but the tension in their body?
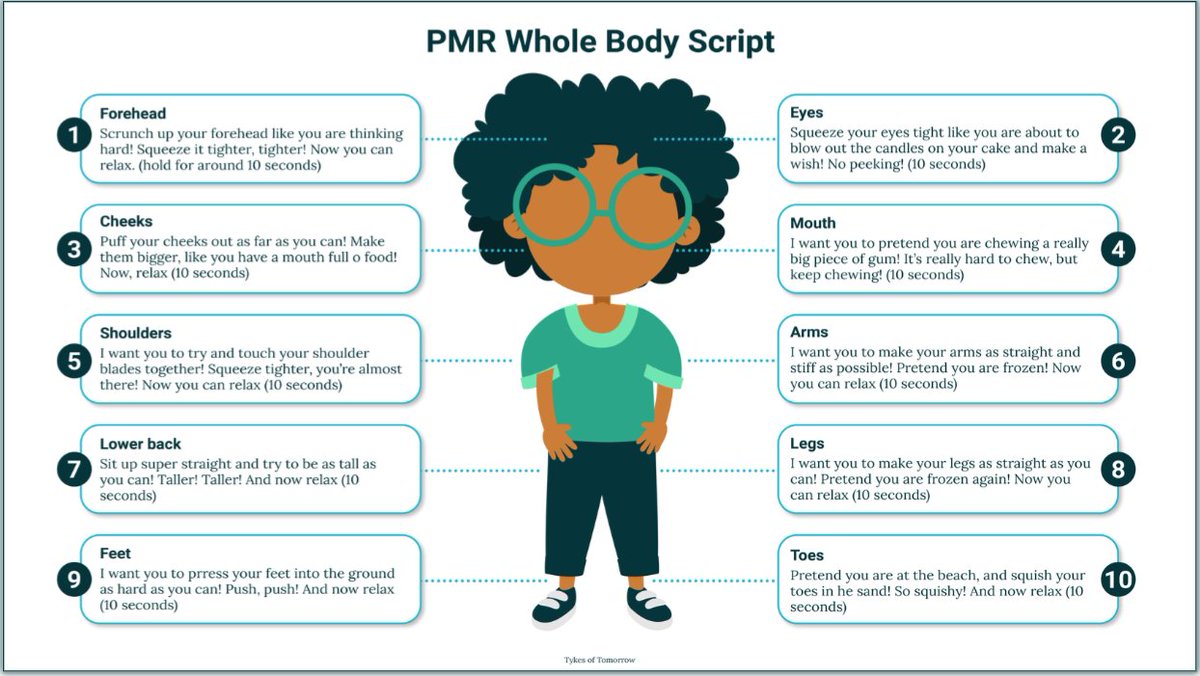
Progressive Muscle Relaxation (PMR) helps interrupt that cycle, reducing arousal and reinforcing regulation.
Here’s how PMR can support patients with chronic anxiety and tension, and how clinicians can integrate it in practice. 👇🧵
Progressive Muscle Relaxation (PMR) helps interrupt that cycle, reducing arousal and reinforcing regulation.
Here’s how PMR can support patients with chronic anxiety and tension, and how clinicians can integrate it in practice. 👇🧵
When dysregulation hits, the body often reacts before the mind.
Tension builds → signals threat.
Release → signals safety.
PMR retrains patients to notice tension early, release it, and send calming cues through their nervous system.
Tension builds → signals threat.
Release → signals safety.
PMR retrains patients to notice tension early, release it, and send calming cues through their nervous system.
The science of PMR
Patients activate the parasympathetic nervous system by intentionally tensing and releasing muscles, which is the body’s “rest and digest” mode.
Over time, this builds interoceptive awareness, helping patients recognise stress signals before they become overwhelmed.
Patients activate the parasympathetic nervous system by intentionally tensing and releasing muscles, which is the body’s “rest and digest” mode.
Over time, this builds interoceptive awareness, helping patients recognise stress signals before they become overwhelmed.
Chronic tension keeps the body on alert
For many patients, anxiety and trauma leave the body in a constant state of muscular tension.
This baseline hyperarousal sustains emotional reactivity.
PMR interrupts the loop, reducing somatic symptoms and lowering overall arousal.
For many patients, anxiety and trauma leave the body in a constant state of muscular tension.
This baseline hyperarousal sustains emotional reactivity.
PMR interrupts the loop, reducing somatic symptoms and lowering overall arousal.
Who benefits most from PMR?
Evidence shows PMR is effective across:
● BPD and complex PTSD
● Anxiety disorders
● Trauma survivors
● Chronic pain syndromes
● Sleep disturbances linked to hyperarousal
Evidence shows PMR is effective across:
● BPD and complex PTSD
● Anxiety disorders
● Trauma survivors
● Chronic pain syndromes
● Sleep disturbances linked to hyperarousal
Evidence in adolescents
A 2024 quasi-experimental study (Köse Kabakcıoğlu & Ayaz-Alkaya) showed PMR significantly reduced stress, anxiety, and depression in adolescents after 8 weeks of practice.
This reinforces PMR as a low-cost, low-risk intervention with broad applicability across patient groups.
A 2024 quasi-experimental study (Köse Kabakcıoğlu & Ayaz-Alkaya) showed PMR significantly reduced stress, anxiety, and depression in adolescents after 8 weeks of practice.
This reinforces PMR as a low-cost, low-risk intervention with broad applicability across patient groups.
Why it works in therapy
The therapeutic gain isn’t just relaxation, it’s contrast awareness.
By noticing the shift between tension and release, patients learn to detect subtle signs of stress early, turning awareness into regulation.
The therapeutic gain isn’t just relaxation, it’s contrast awareness.
By noticing the shift between tension and release, patients learn to detect subtle signs of stress early, turning awareness into regulation.
Clinical integration
Use PMR:
● Before exposure work (to reduce baseline arousal)
● After interpersonal conflict (to reset the body)
● In a crisis, as a grounding skill
● To improve sleep onset
Use PMR:
● Before exposure work (to reduce baseline arousal)
● After interpersonal conflict (to reset the body)
● In a crisis, as a grounding skill
● To improve sleep onset
A clinician’s framing tip
Present PMR as nervous system training, not just relaxation.
Patients are more likely to practise proactively if they see it as rewiring stress responses, rather than a “coping trick.”
Present PMR as nervous system training, not just relaxation.
Patients are more likely to practise proactively if they see it as rewiring stress responses, rather than a “coping trick.”
Why this matters
For patients who feel constantly “on edge,” PMR offers:
● A sense of bodily safety
● A portable, evidence-based tool
● A foundation for tolerating deeper therapy work
For patients who feel constantly “on edge,” PMR offers:
● A sense of bodily safety
● A portable, evidence-based tool
● A foundation for tolerating deeper therapy work
Why “noticing the contrast” works
Recognising the shift from tension to relaxation helps patients identify early signs of physical stress.
That body awareness becomes a powerful self-regulation tool.
Recognising the shift from tension to relaxation helps patients identify early signs of physical stress.
That body awareness becomes a powerful self-regulation tool.
From skill to framework
PMR is one example of how body-based strategies strengthen psychiatric care.
In DBT, skills like PMR sit alongside mindfulness, distress tolerance, and emotion regulation, which form an integrated system that clinicians can apply directly in practice.
PMR is one example of how body-based strategies strengthen psychiatric care.
In DBT, skills like PMR sit alongside mindfulness, distress tolerance, and emotion regulation, which form an integrated system that clinicians can apply directly in practice.
Want to help patients regulate faster and recover better?
In our CPD-accredited course, “Dialectical Behaviour Therapy (DBT) – A Practical Guide for Clinicians”, you will learn practical, neuroscience-informed DBT strategies, from emotional regulation to distress tolerance, that you can apply straight to your sessions.
psychscene.co/47JV37R
In our CPD-accredited course, “Dialectical Behaviour Therapy (DBT) – A Practical Guide for Clinicians”, you will learn practical, neuroscience-informed DBT strategies, from emotional regulation to distress tolerance, that you can apply straight to your sessions.
psychscene.co/47JV37R
• • •
Missing some Tweet in this thread? You can try to
force a refresh