🚨Health insurance plan with NO LIMITS?
That’s what Niva Bupa ReAssure 3.0 promises.
👉Unlimited cover
👉Day 1 coverage for 145 PEDs
👉OPD, global coverage
...and more
But is it really as limitless as it sounds?🤔
Let's break it down👇
#BeshakDecodes #review #notsponsored
That’s what Niva Bupa ReAssure 3.0 promises.
👉Unlimited cover
👉Day 1 coverage for 145 PEDs
👉OPD, global coverage
...and more
But is it really as limitless as it sounds?🤔
Let's break it down👇
#BeshakDecodes #review #notsponsored

🏥 First, what’s different about ReAssure 3.0?
It comes with an unlimited cover model - without bonus or restore benefits.
You can make multiple claims in a year, without worrying about exhausting your sum insured.
It comes with an unlimited cover model - without bonus or restore benefits.
You can make multiple claims in a year, without worrying about exhausting your sum insured.

🛏️ But unlimited cover ≠ unlimited room choices.
There are 4 variants, and the room rent limit varies across each:
• Classic: General room
• Select: Twin sharing room
• Elite: Any room (except Deluxe, Suite)
• Black: Any room
There are 4 variants, and the room rent limit varies across each:
• Classic: General room
• Select: Twin sharing room
• Elite: Any room (except Deluxe, Suite)
• Black: Any room
Choosing a higher room than eligible?
You’ll have to bear proportionate deductions.
beshak.org/insurance/heal…
You’ll have to bear proportionate deductions.
beshak.org/insurance/heal…
🩺 Key features across variants:
• All day-care treatments covered
• Pre-hospitalisation: 60 days
• Post-hospitalisation: 180 days
• Organ donor & domiciliary: covered up to SI
• Modern treatments: ₹1L limit (Classic/Select), no limit (Elite/Black)
• All day-care treatments covered
• Pre-hospitalisation: 60 days
• Post-hospitalisation: 180 days
• Organ donor & domiciliary: covered up to SI
• Modern treatments: ₹1L limit (Classic/Select), no limit (Elite/Black)
📍Lock the Clock:
Under Elite & Black variants, your age gets locked at entry for premium calculation - until you make a claim.
⚠️Premiums may still change based on external factors like inflation, etc.
Under Elite & Black variants, your age gets locked at entry for premium calculation - until you make a claim.
⚠️Premiums may still change based on external factors like inflation, etc.
⌛ Waiting periods:
• For specific illnesses: 24 months (can reduce to 12 months or increase to 36 months, with a rider)
• For PEDs: 36 months (can reduce to 24/12 months, with a rider)
• For specific illnesses: 24 months (can reduce to 12 months or increase to 36 months, with a rider)
• For PEDs: 36 months (can reduce to 24/12 months, with a rider)
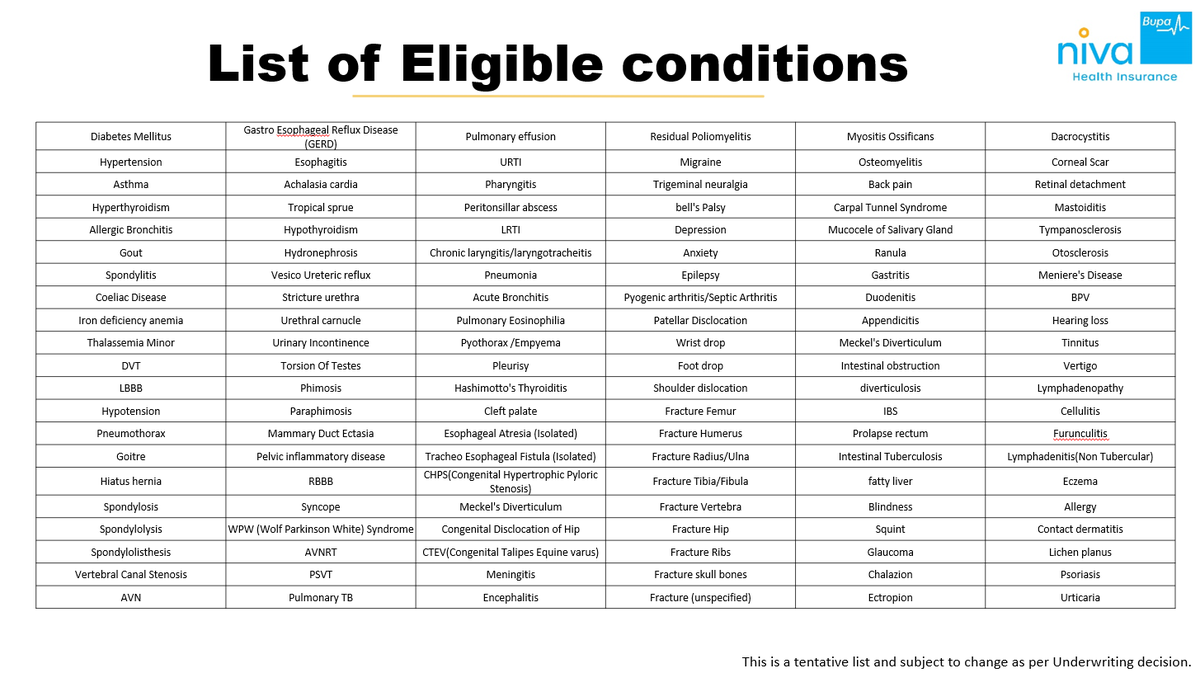
It also covers around 145 conditions covered from Day 1 if you choose to pay loading i.e. extra premium (check below image for the list of PEDs)
⚠️ Just note: Below list is tentative and final approval depends on underwriting.
⚠️ Just note: Below list is tentative and final approval depends on underwriting.
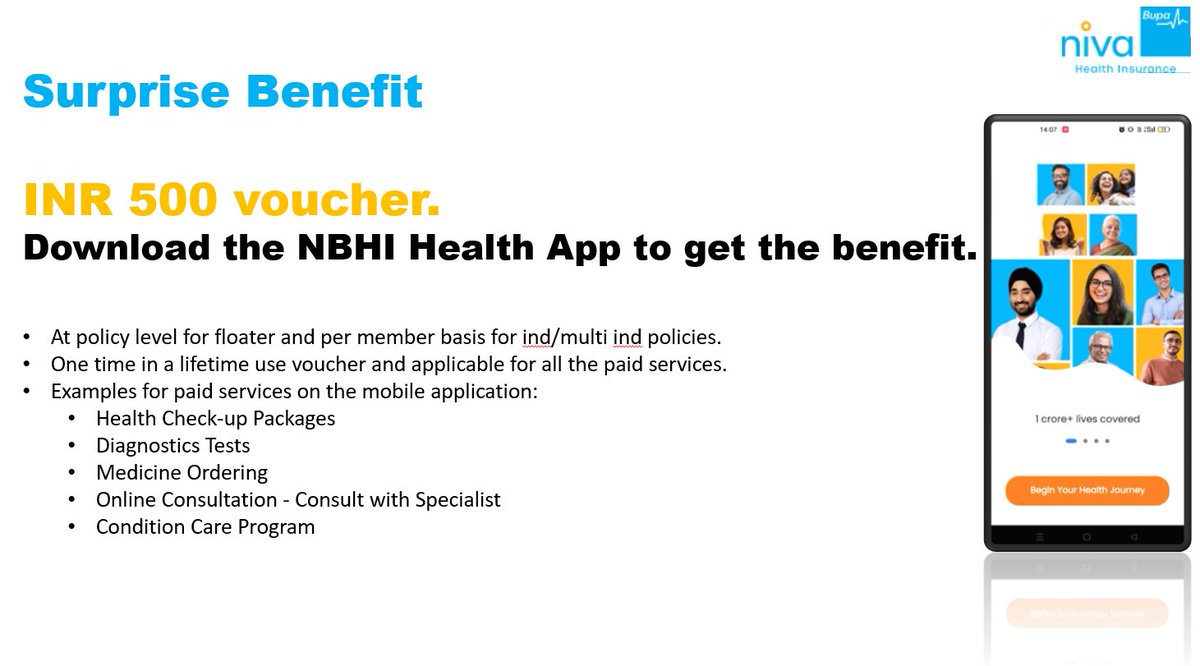
🧩 Then there’s Niva Bupa One - a membership offering:
✅ Priority claim handling
✅ Dedicated support
Interesting promise - we’ll need to see how it plays out during real claims.
✅ Priority claim handling
✅ Dedicated support
Interesting promise - we’ll need to see how it plays out during real claims.

💸 Copay & Deductible
There isn't any mandatory copay or deductible under the plan.
However, you can voluntarily opt for co-pay and deductible to lower your premium.
There isn't any mandatory copay or deductible under the plan.
However, you can voluntarily opt for co-pay and deductible to lower your premium.
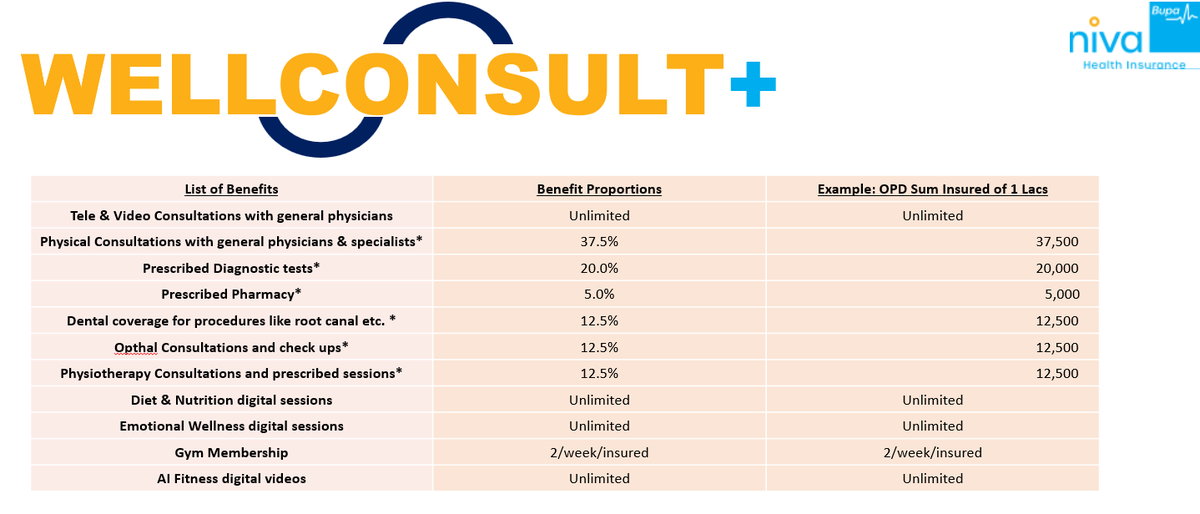
There are 10 benefits available under the OPD cover.
⚠️ If you claim via reimbursement, you’ll have to bear 20% of the approved claim amount as co-pay.
⚠️ If you claim via reimbursement, you’ll have to bear 20% of the approved claim amount as co-pay.
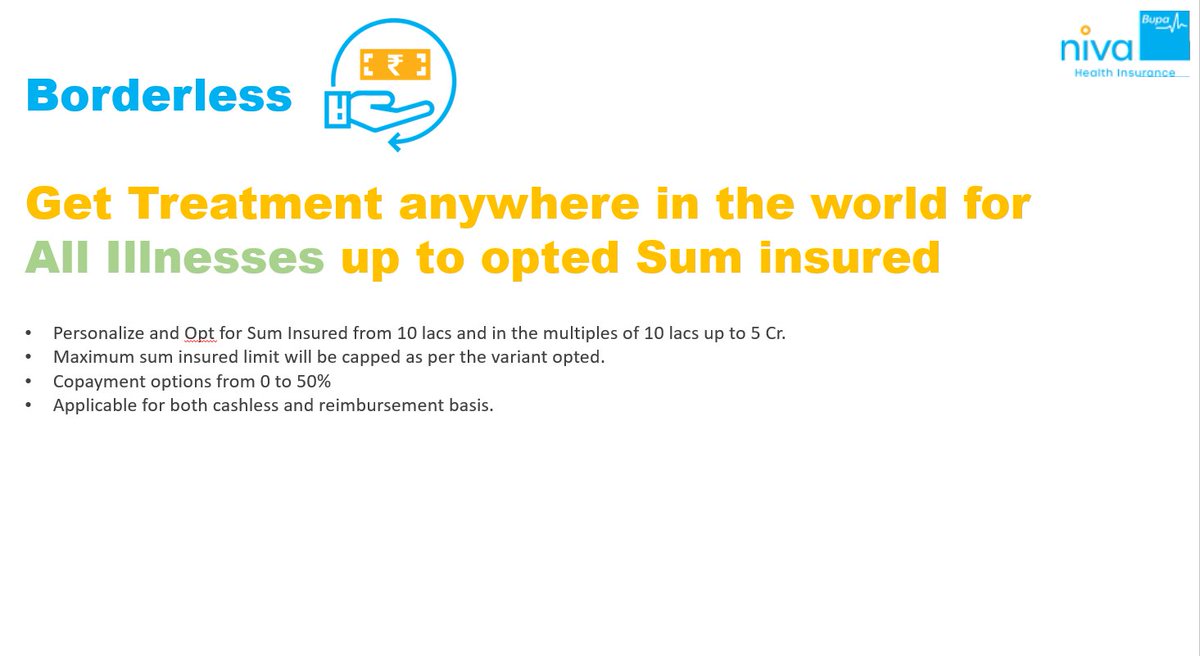
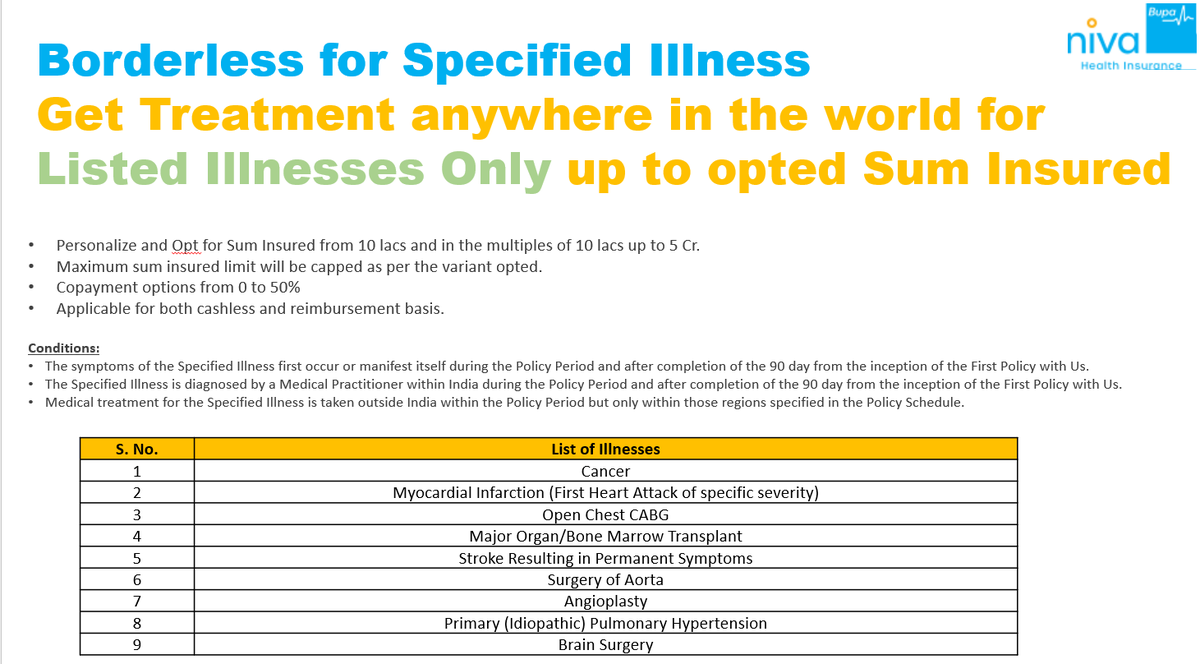
🌍 Want global coverage? You’ve got 2 options:
1️⃣ Borderless: Covers all illnesses globally
2️⃣ Borderless Select: Covers listed illnesses (like cancer, angioplasty, etc.)

1️⃣ Borderless: Covers all illnesses globally
2️⃣ Borderless Select: Covers listed illnesses (like cancer, angioplasty, etc.)
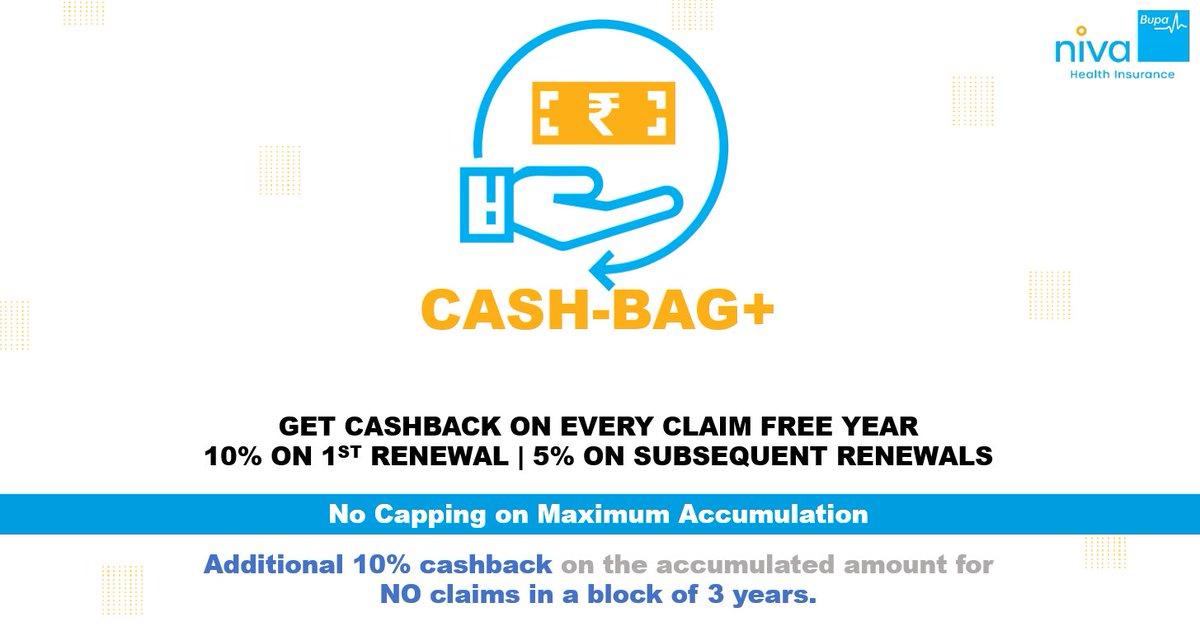
There's also an add-on that gives you a cashback for every year that you don’t make a claim under the plan. 💰 
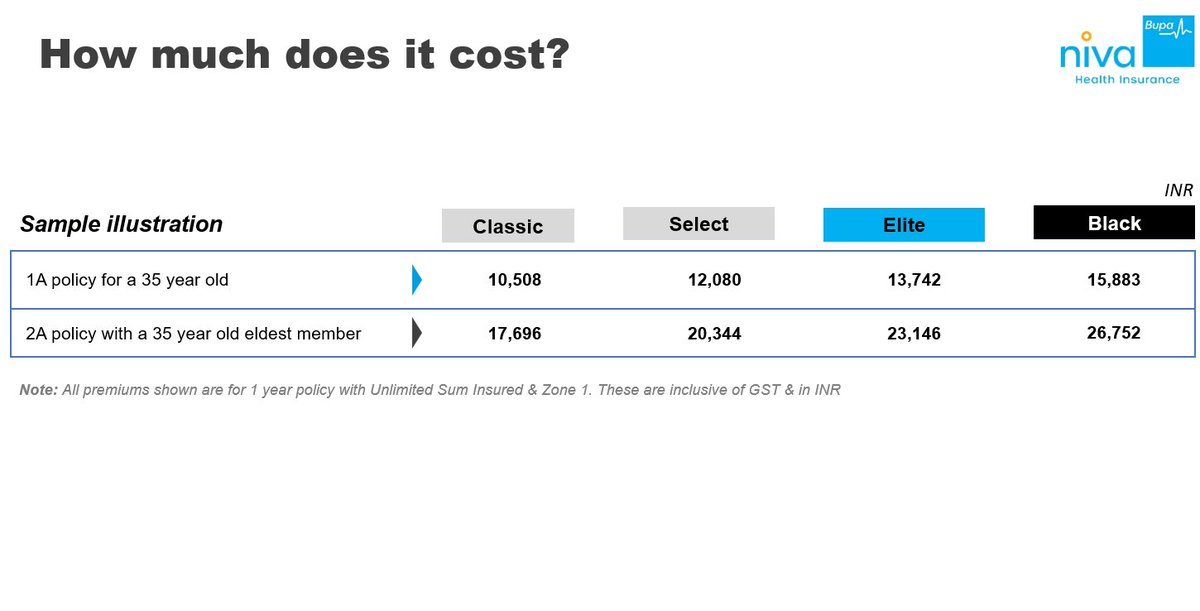
💸 And now, the big question - how expensive is the plan?
Here’s what the base premium looks like for a 35-year-old living in Zone 1 👇
Here’s what the base premium looks like for a 35-year-old living in Zone 1 👇
The detailed policy wording for ReAssure 3.0 is not yet publicly available.
As soon as it's released, we’ll update our Health Decoder tool with a complete breakdown of the plan’s features and fine print.
In the meantime, you can analyse & compare other plans already decoded on our website:
beshak.org/insurance/heal…
As soon as it's released, we’ll update our Health Decoder tool with a complete breakdown of the plan’s features and fine print.
In the meantime, you can analyse & compare other plans already decoded on our website:
beshak.org/insurance/heal…
Learned something new?
Let others make notes too.
Retweet the first tweet below and follow @BeshakIN for more :)
Let others make notes too.
Retweet the first tweet below and follow @BeshakIN for more :)
https://twitter.com/1281287883773505536/status/1960216866795958514
Thank you for your response.
For people who don't know, we are India's only independent research platform for insurance.
We help people find the right plans, experts - without getting influenced by insurers or their commissions
For people who don't know, we are India's only independent research platform for insurance.
We help people find the right plans, experts - without getting influenced by insurers or their commissions
• • •
Missing some Tweet in this thread? You can try to
force a refresh