Here’s a thread on 10 general medicine lessons reinforced in rheumatology 🧵
Tweet 1:
Rheumatology isn’t “super-specialised.”
It’s general medicine… but deeper.
Every principle we learnt in MBBS comes back in rheumatology.
#MedTwitter #Rheumatology @IhabFathiSulima @DrAkhilX @CelestinoGutirr @Janetbirdope @docchennai
Tweet 1:
Rheumatology isn’t “super-specialised.”
It’s general medicine… but deeper.
Every principle we learnt in MBBS comes back in rheumatology.
#MedTwitter #Rheumatology @IhabFathiSulima @DrAkhilX @CelestinoGutirr @Janetbirdope @docchennai
Tweet 2
🌡️ Fever of unknown origin
Clues to think beyond infection:
• Rash that comes & goes
• Cytopenias
• Very high ferritin
• Hepatosplenomegaly
• Serositis
Sometimes, fever is inflammation wearing a disguise.
🌡️ Fever of unknown origin
Clues to think beyond infection:
• Rash that comes & goes
• Cytopenias
• Very high ferritin
• Hepatosplenomegaly
• Serositis
Sometimes, fever is inflammation wearing a disguise.
Tweet 3
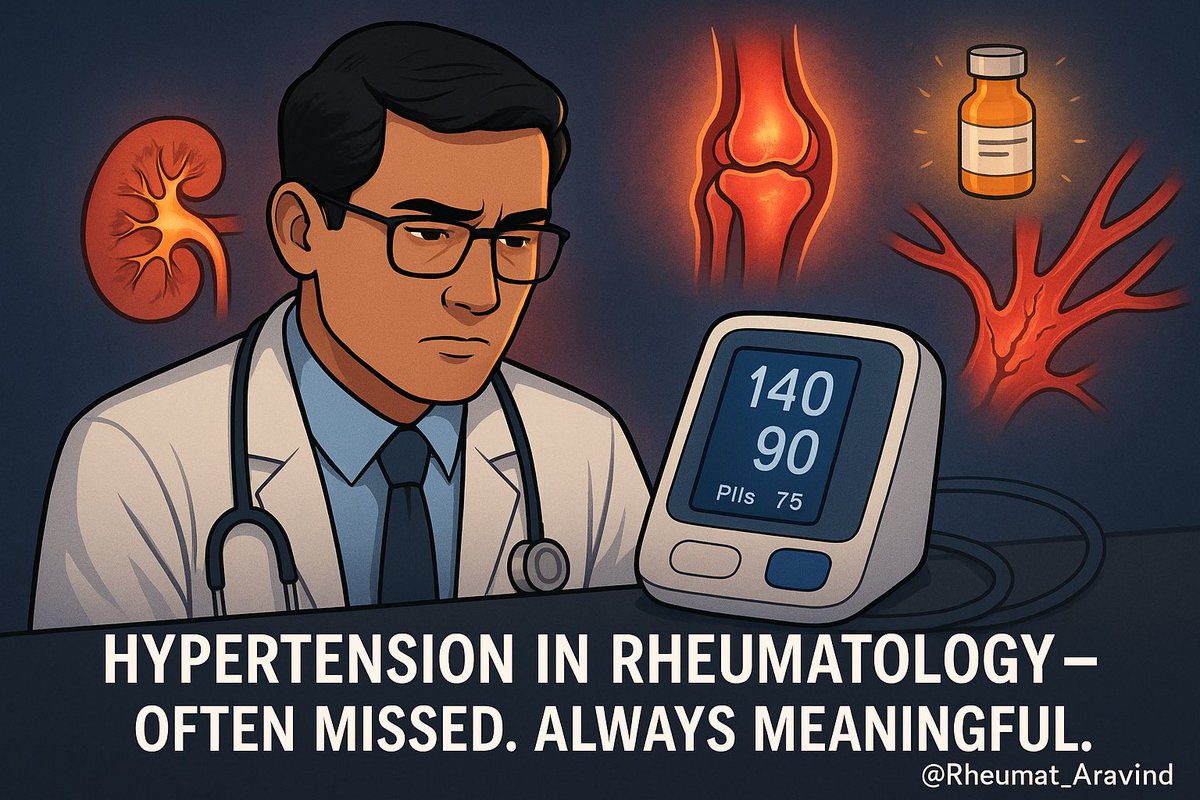
🫀 Severe hypertension in a 20-something?
Always feel the pulses.
Bruits, unequal BP in arms → large vessel vasculitis.
Sudden crisis in systemic sclerosis → renal emergency.
Not all BP rises are “essential.”
🫀 Severe hypertension in a 20-something?
Always feel the pulses.
Bruits, unequal BP in arms → large vessel vasculitis.
Sudden crisis in systemic sclerosis → renal emergency.
Not all BP rises are “essential.”
Tweet 4
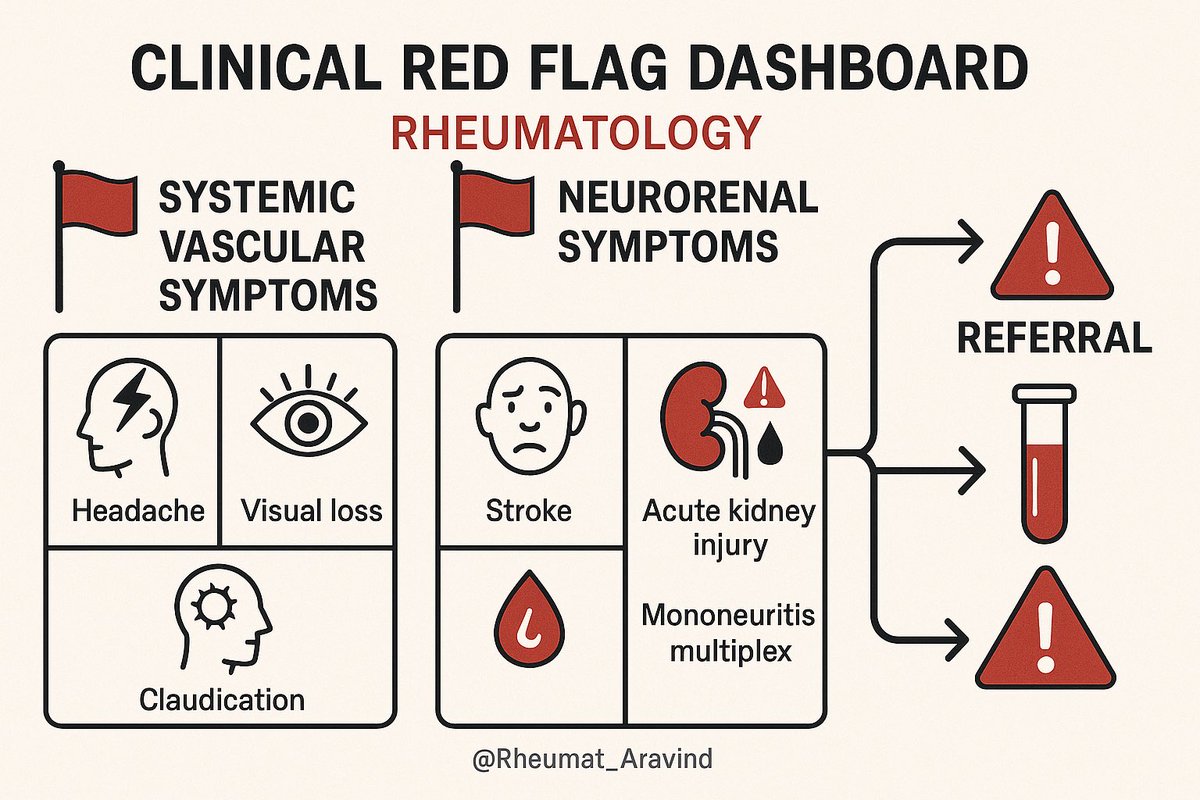
🧠 Headache that’s new-onset, with jaw pain & raised ESR in >50 yrs = red flag.
Giant Cell Arteritis is a race against blindness.
Treatment should start before biopsy, not after.
🧠 Headache that’s new-onset, with jaw pain & raised ESR in >50 yrs = red flag.
Giant Cell Arteritis is a race against blindness.
Treatment should start before biopsy, not after.
Tweet 5
🫁 Chronic cough despite antibiotics & anti-TB?
Think interstitial lung disease, pulmonary hypertension, or alveolar hemorrhage.
TB is common—but overdiagnosis is even more common.
🫁 Chronic cough despite antibiotics & anti-TB?
Think interstitial lung disease, pulmonary hypertension, or alveolar hemorrhage.
TB is common—but overdiagnosis is even more common.
Tweet 6
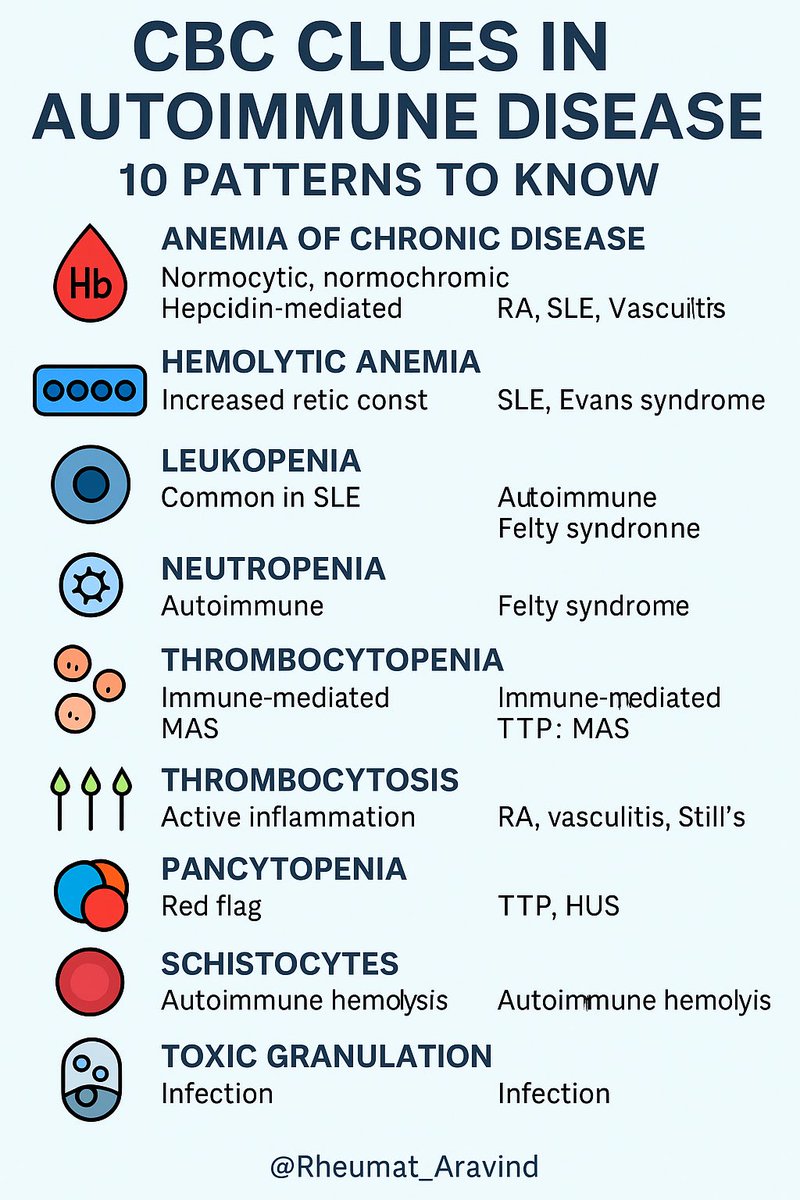
🩸 Anemia = not just “low Hb.”
• Microcytic → celiac overlap?
• Normocytic → chronic inflammation?
• Hemolytic → autoimmune?
Every Hb drop is telling you a story.
🩸 Anemia = not just “low Hb.”
• Microcytic → celiac overlap?
• Normocytic → chronic inflammation?
• Hemolytic → autoimmune?
Every Hb drop is telling you a story.
Tweet 7
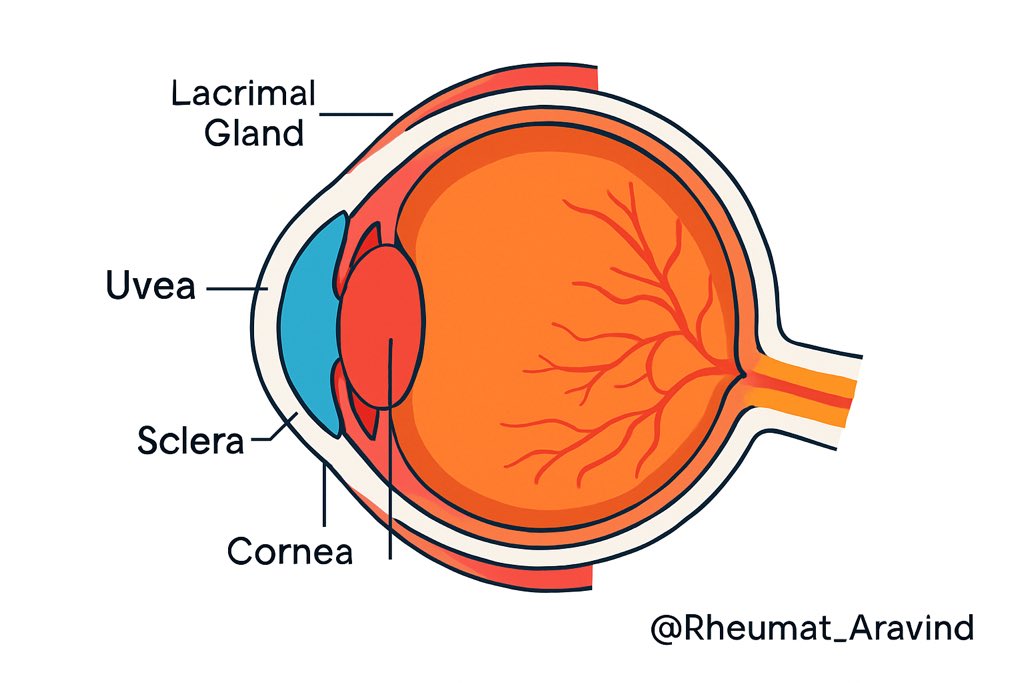
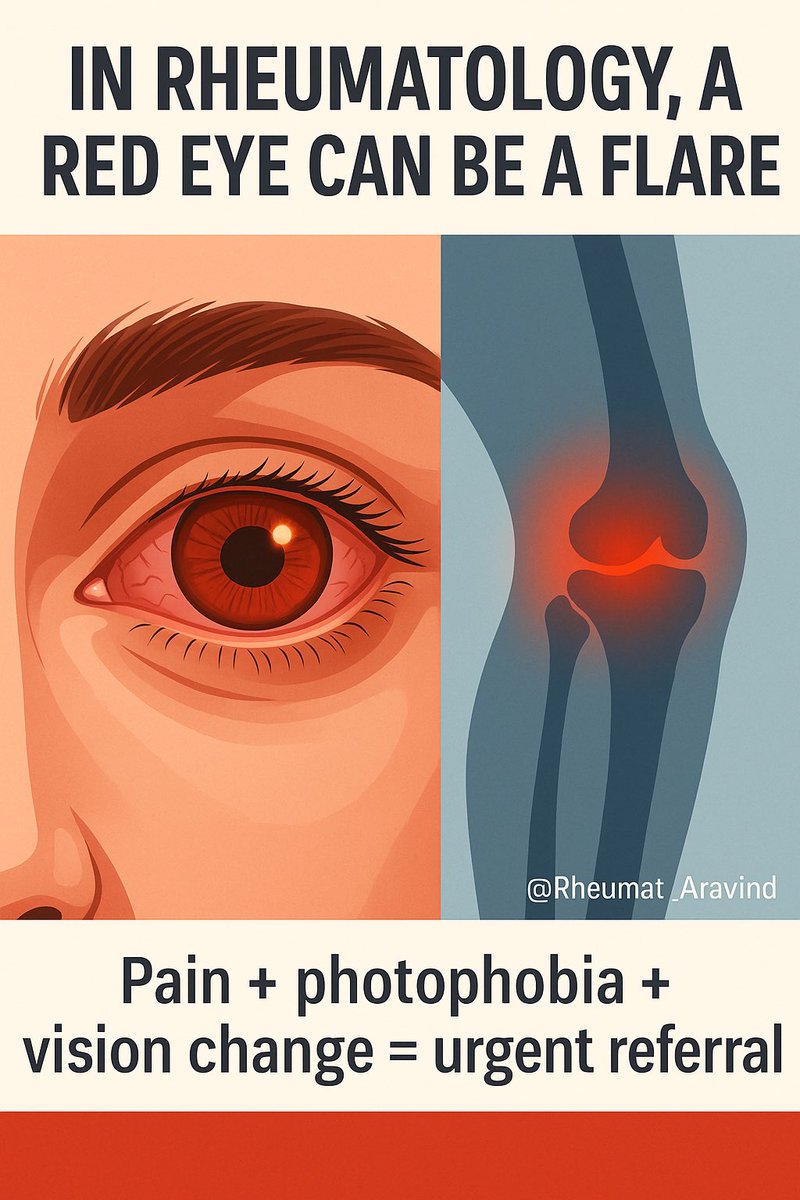
👁️ Painful, recurrent red eye?
Often mislabeled “allergic conjunctivitis.”
Could be uveitis, episcleritis, or scleritis.
The eye sometimes diagnoses the joint before the joint hurts.
👁️ Painful, recurrent red eye?
Often mislabeled “allergic conjunctivitis.”
Could be uveitis, episcleritis, or scleritis.
The eye sometimes diagnoses the joint before the joint hurts.
Tweet 8
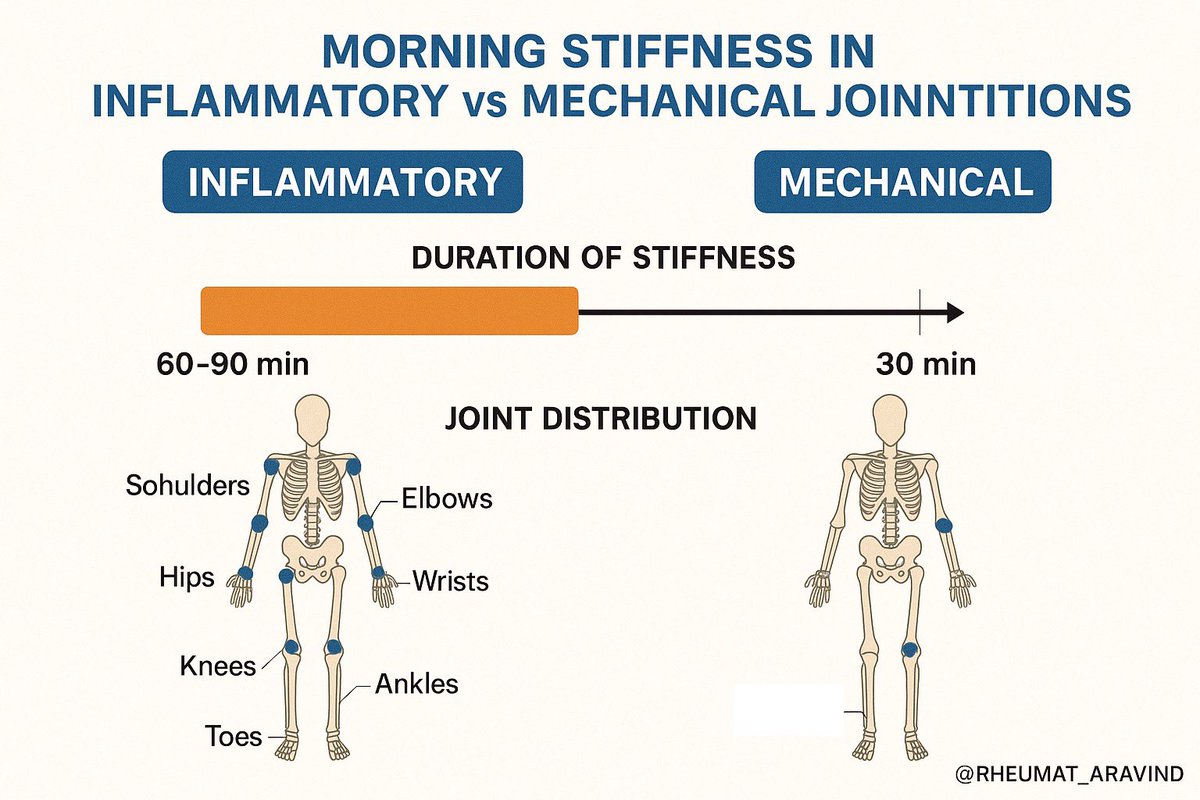
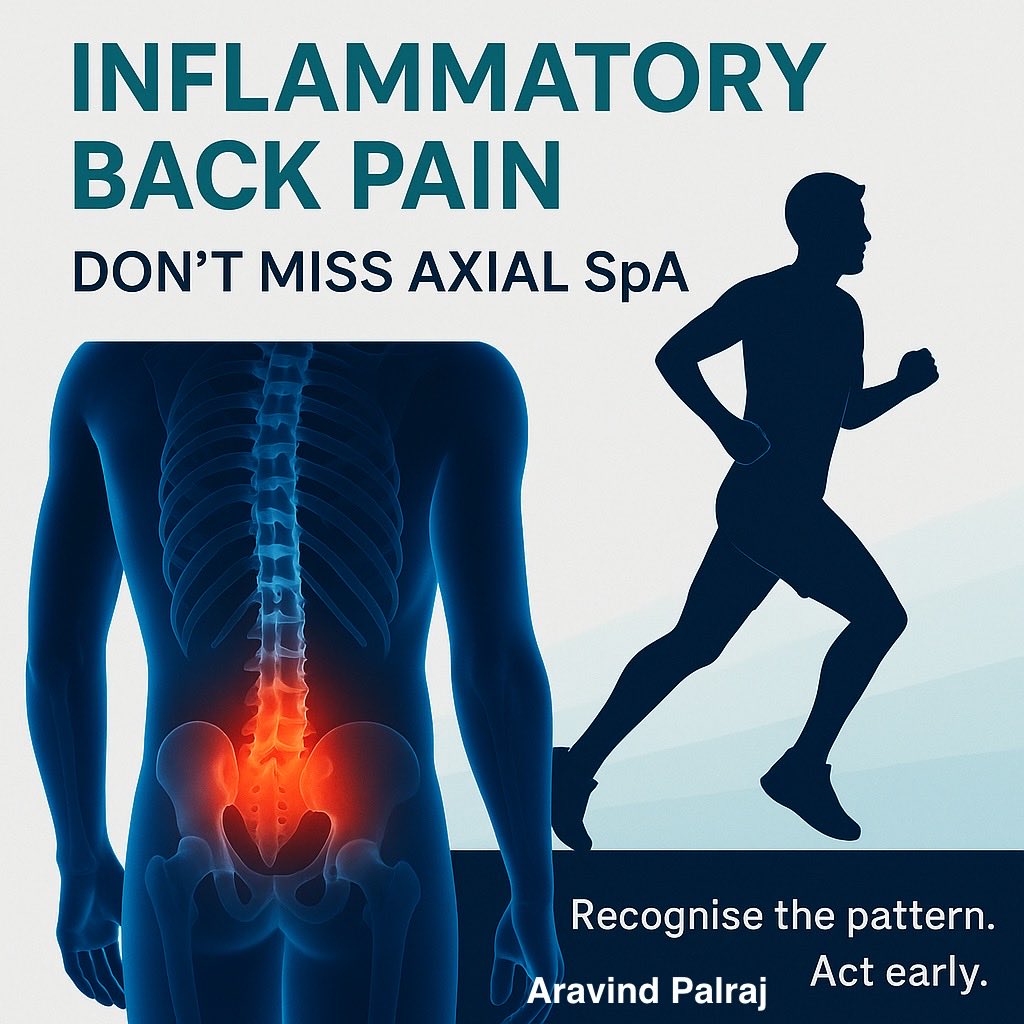
🦴 Back pain in the young:
• Insidious onset
• Morning stiffness >30 min
• Improves with activity
That’s inflammatory back pain.
Average delay in diagnosis = 7–10 years.
🦴 Back pain in the young:
• Insidious onset
• Morning stiffness >30 min
• Improves with activity
That’s inflammatory back pain.
Average delay in diagnosis = 7–10 years.
Tweet 9
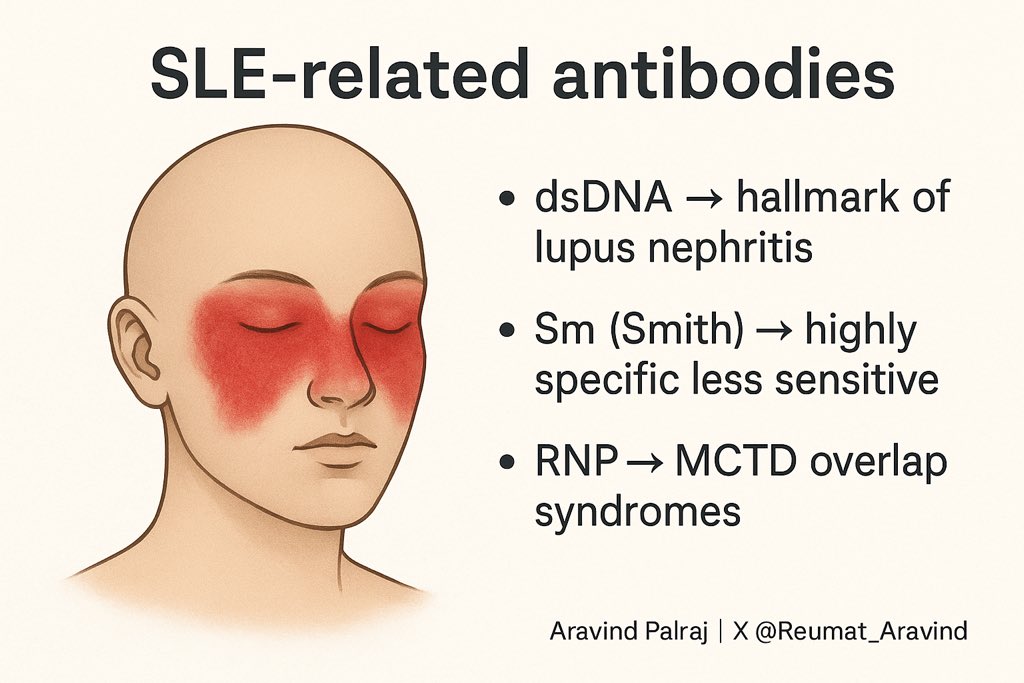
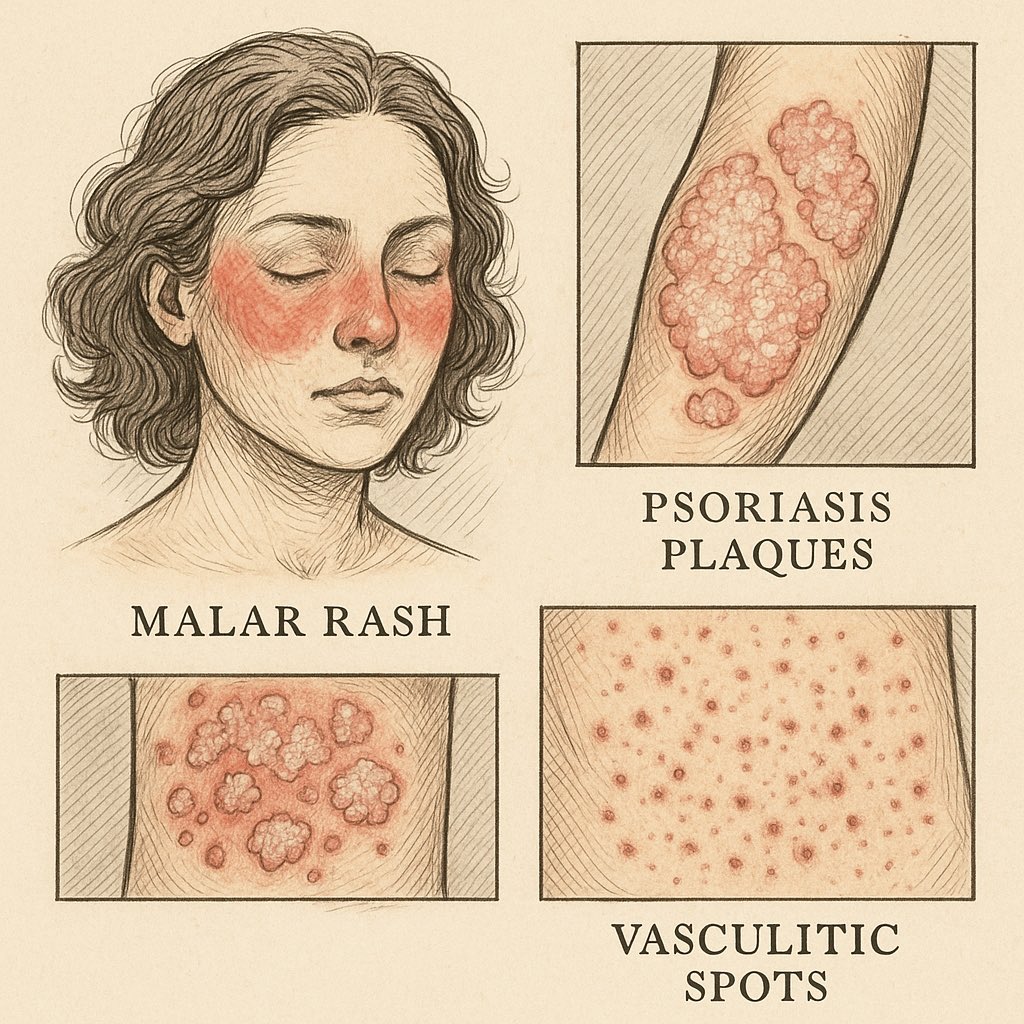
🖐️ The skin is a map:
• Heliotrope rash → dermatomyositis
• Malar rash → lupus
• Digital ulcers → systemic sclerosis
• Vasculitic lesions → systemic vasculitis
Look at the skin. It whispers secrets.
🖐️ The skin is a map:
• Heliotrope rash → dermatomyositis
• Malar rash → lupus
• Digital ulcers → systemic sclerosis
• Vasculitic lesions → systemic vasculitis
Look at the skin. It whispers secrets.
Tweet 10
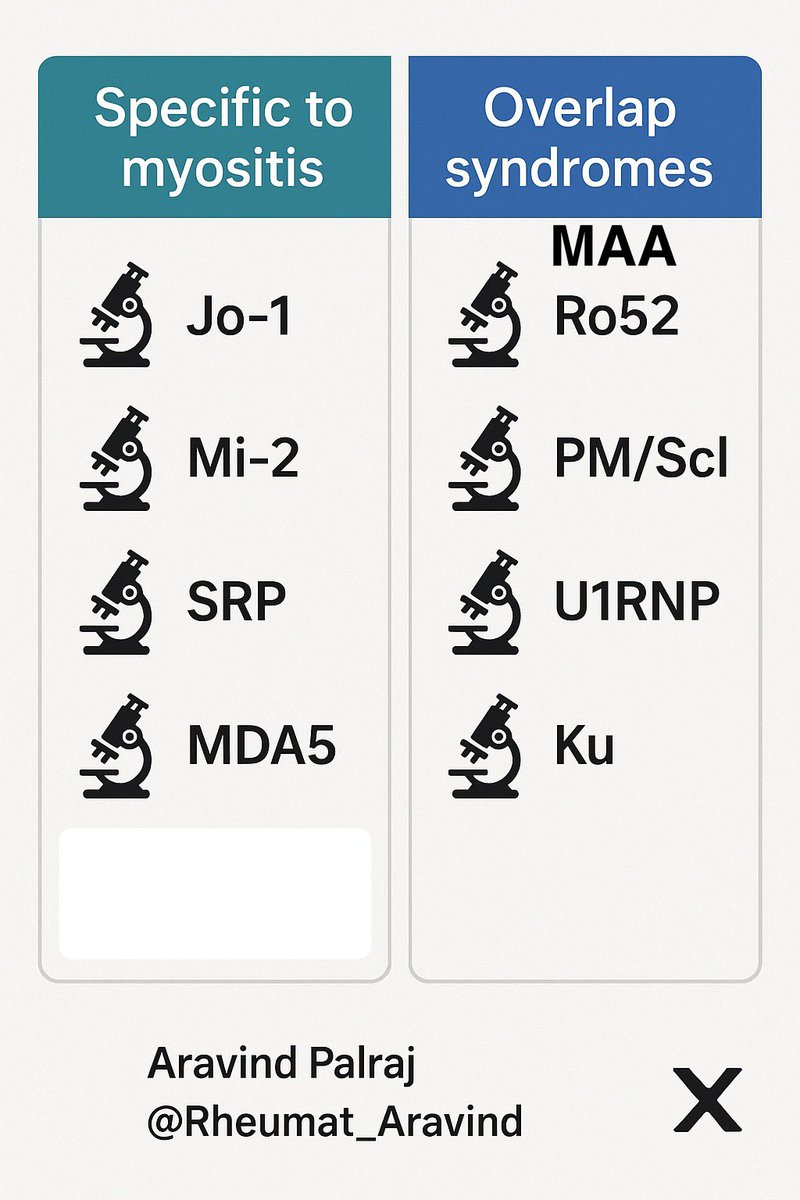
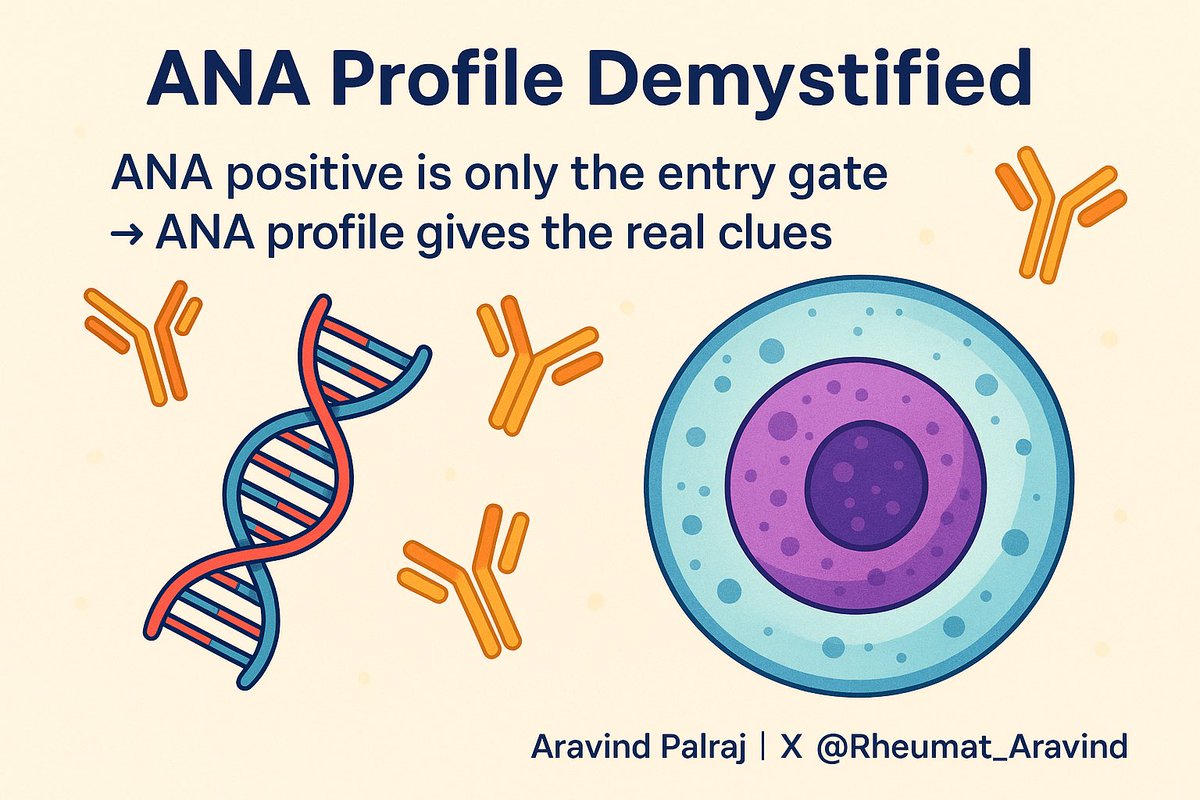
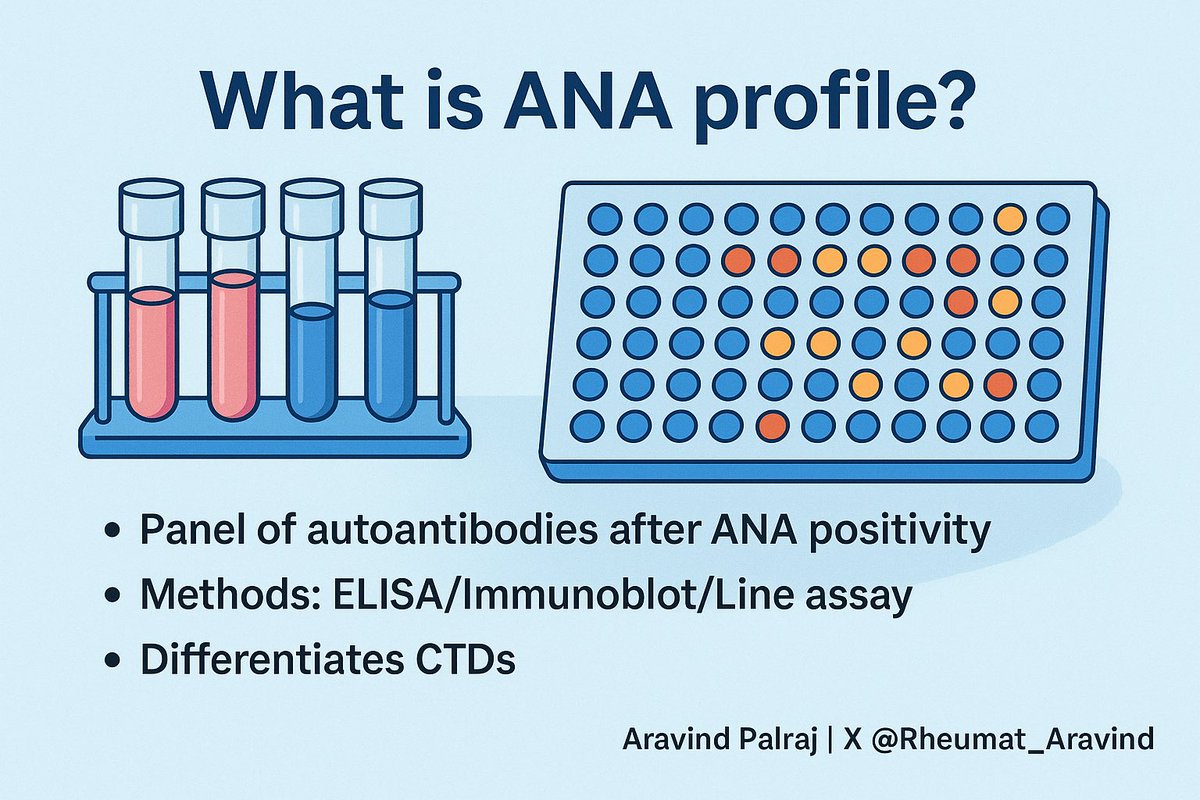
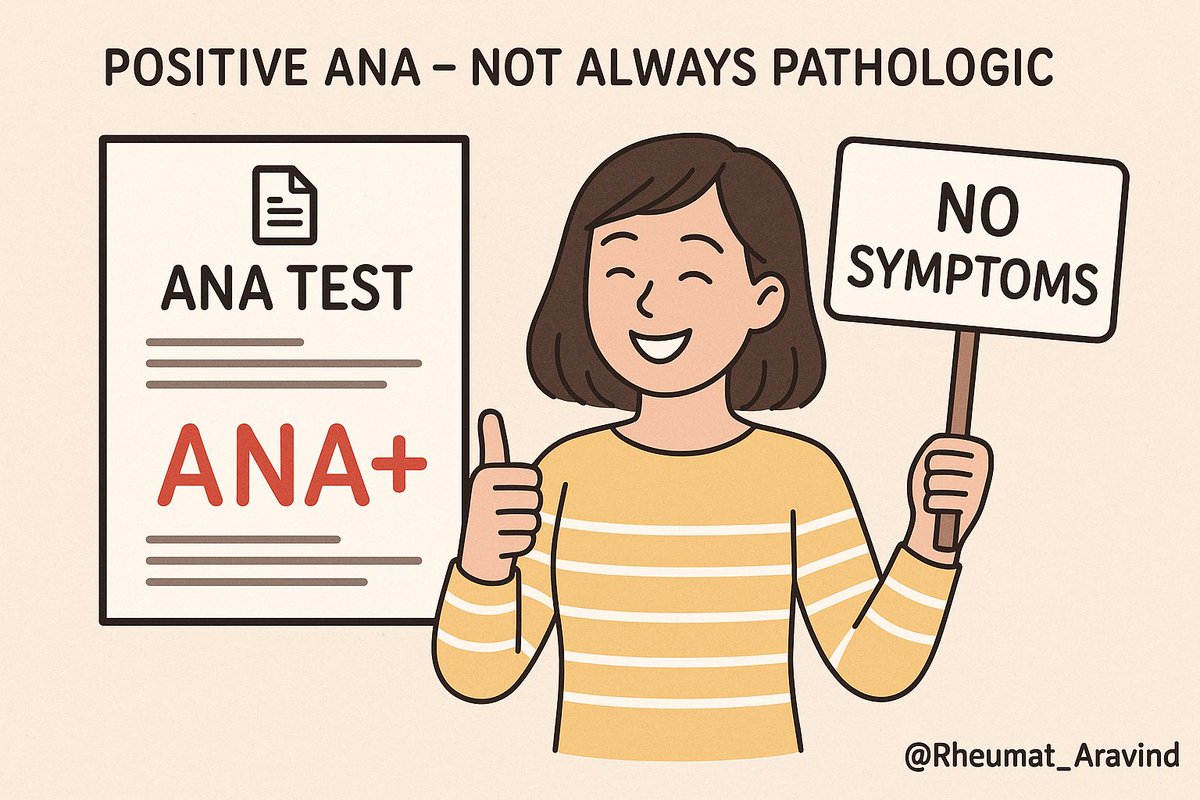
🧪 Positive ANA ≠ lupus.
ESR high ≠ infection.
Rheumatoid factor ≠ RA.
Tests don’t make diagnoses. Context does.
🧪 Positive ANA ≠ lupus.
ESR high ≠ infection.
Rheumatoid factor ≠ RA.
Tests don’t make diagnoses. Context does.
Tweet 11
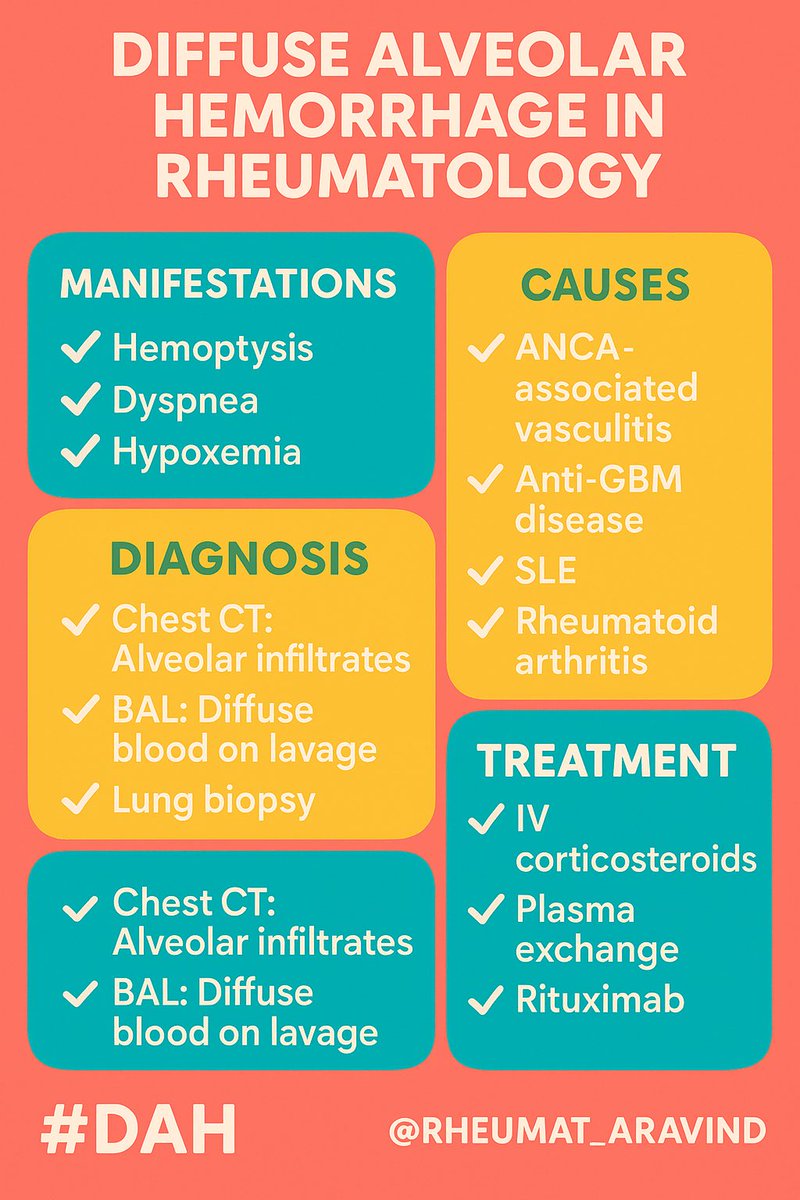
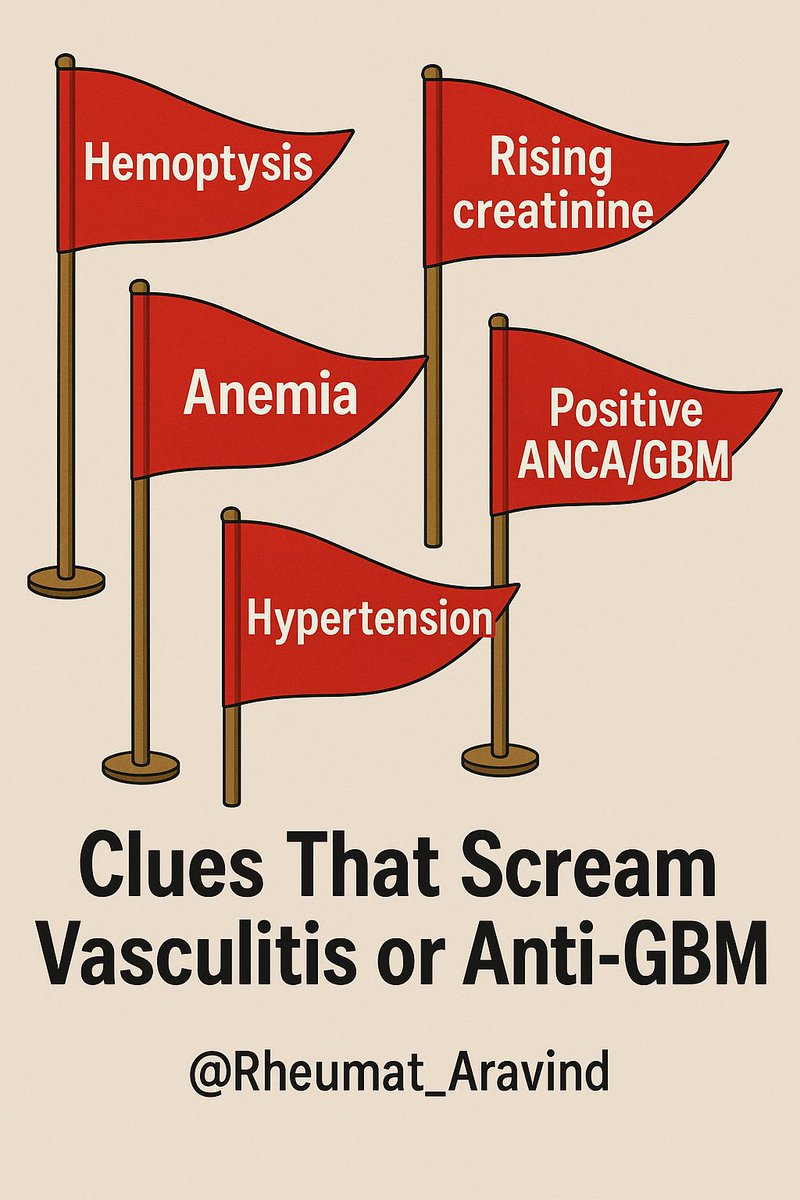
🫁 Hemoptysis + drop in Hb + bilateral infiltrates = not pneumonia.
Think diffuse alveolar hemorrhage.
Needs immunosuppression, not antibiotics.
🫁 Hemoptysis + drop in Hb + bilateral infiltrates = not pneumonia.
Think diffuse alveolar hemorrhage.
Needs immunosuppression, not antibiotics.
Tweet 12
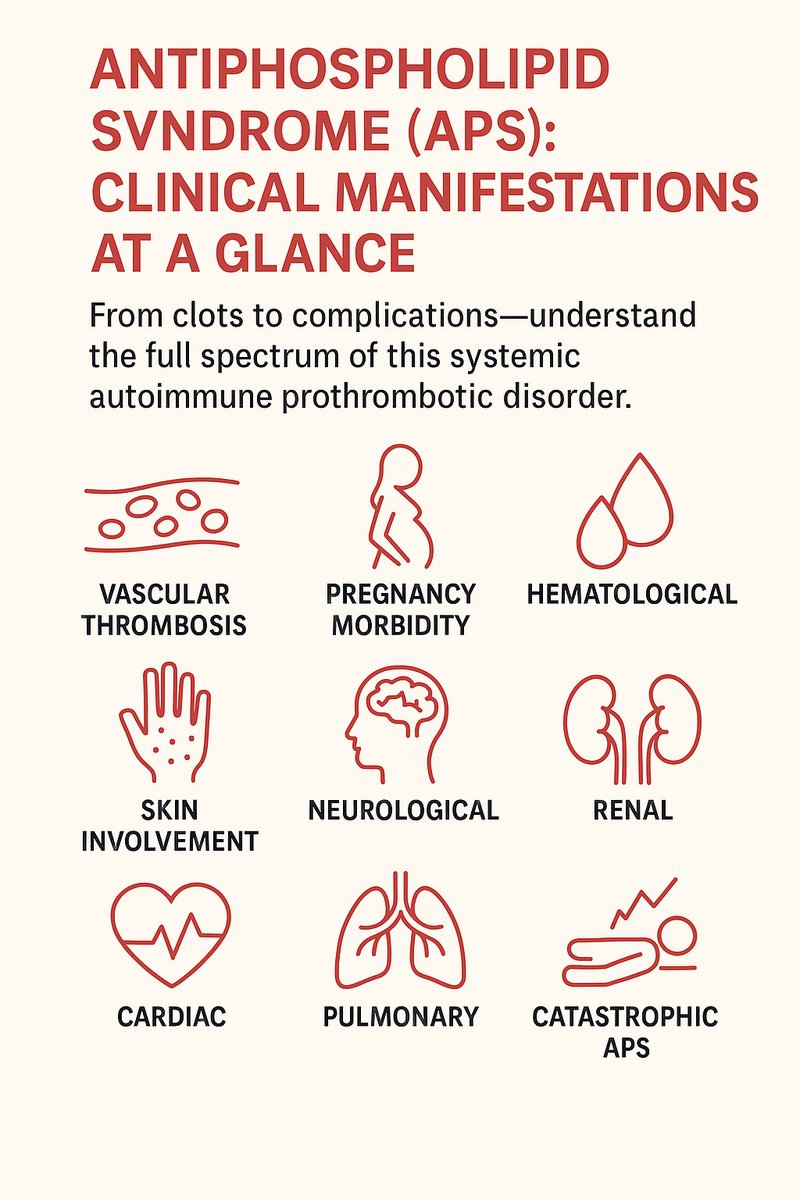
🦵 Leg swelling in a young woman on OCPs? DVT.
But if she also has miscarriages → think antiphospholipid syndrome.
Every clot deserves a deeper look.
🦵 Leg swelling in a young woman on OCPs? DVT.
But if she also has miscarriages → think antiphospholipid syndrome.
Every clot deserves a deeper look.
Tweet 13
🧴 Raynaud’s phenomenon
White → blue → red fingers on cold exposure.
In teenagers, often benign.
In adults, could be systemic sclerosis, MCTD, or lupus.
Don’t miss the systemic clue hiding in the fingertips.
🧴 Raynaud’s phenomenon
White → blue → red fingers on cold exposure.
In teenagers, often benign.
In adults, could be systemic sclerosis, MCTD, or lupus.
Don’t miss the systemic clue hiding in the fingertips.

Tweet 14
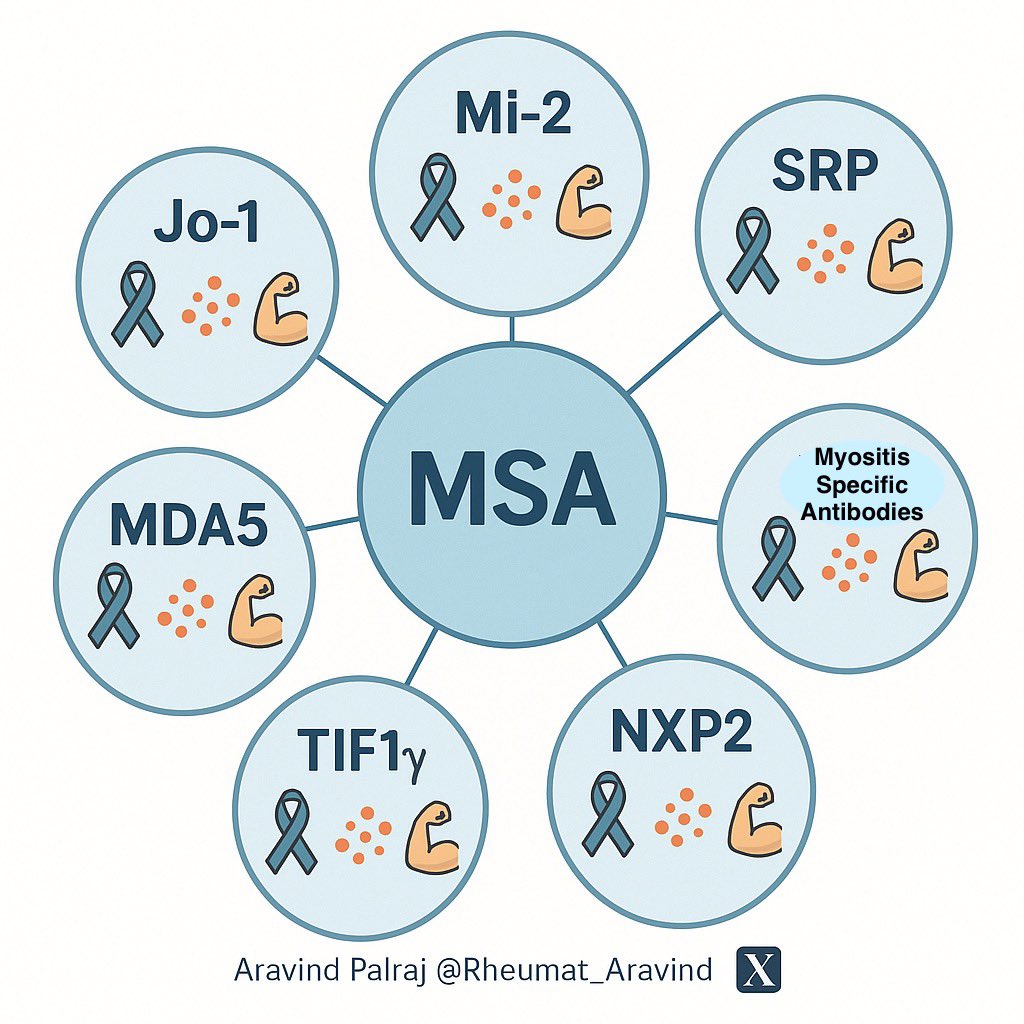
🧑🦽 Weakness isn’t always neuro.
If it’s proximal (difficulty combing hair, climbing stairs), check CK.
Could be myositis → treatable if caught early.
🧑🦽 Weakness isn’t always neuro.
If it’s proximal (difficulty combing hair, climbing stairs), check CK.
Could be myositis → treatable if caught early.

Tweet 15
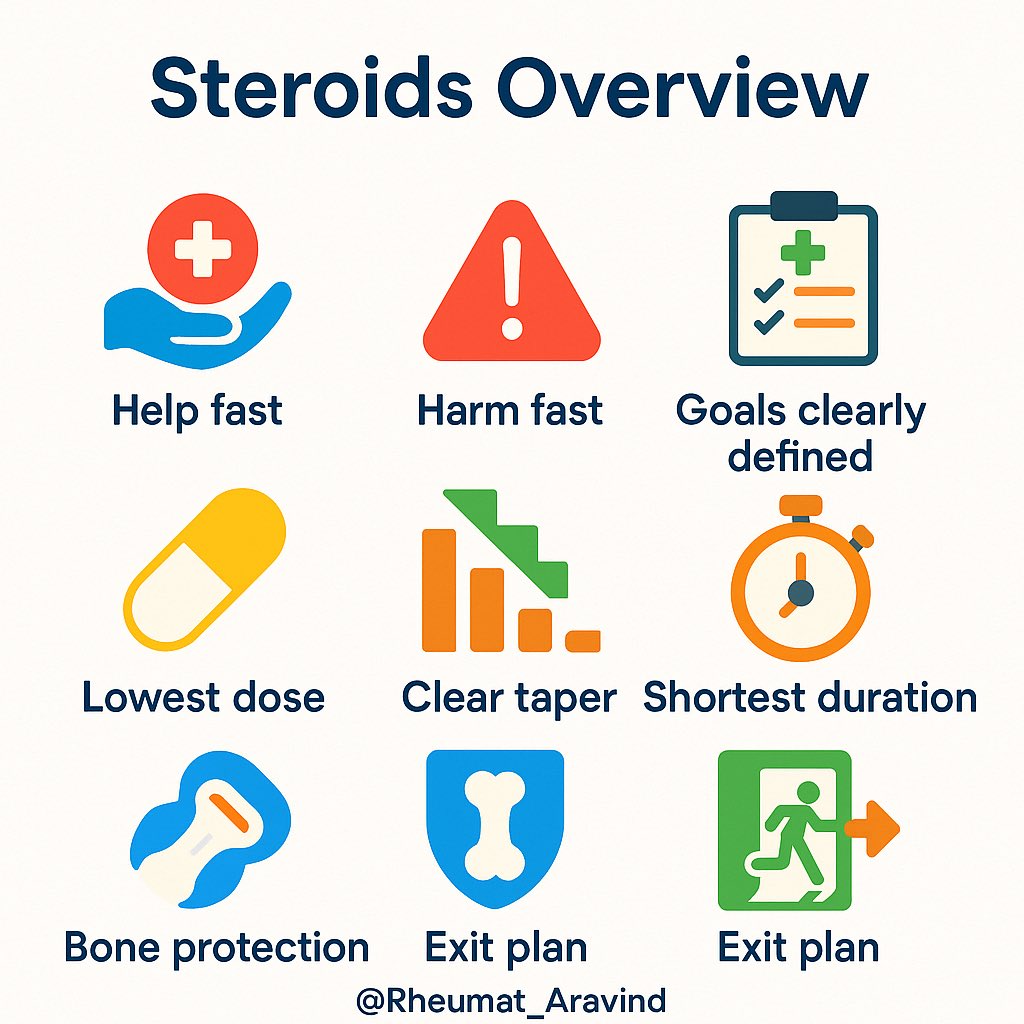
💊 “Steroid responder” doesn’t mean asthma always.
If fever, rash, cytopenia melt away with steroids → think autoimmune flare or vasculitis.
Steroid response is a clue, not just a treatment.
💊 “Steroid responder” doesn’t mean asthma always.
If fever, rash, cytopenia melt away with steroids → think autoimmune flare or vasculitis.
Steroid response is a clue, not just a treatment.
Tweet 16 (Closer)
Everyday complaints can be routine.
Or they can be a zebra 🦓 hiding in plain sight.
The difference?
👉 Curiosity.
👉 Listening.
👉 Examining.
That’s how lives are saved.
#MedTwitter #FOAMed #ClinicalPearls
Everyday complaints can be routine.
Or they can be a zebra 🦓 hiding in plain sight.
The difference?
👉 Curiosity.
👉 Listening.
👉 Examining.
That’s how lives are saved.
#MedTwitter #FOAMed #ClinicalPearls
• • •
Missing some Tweet in this thread? You can try to
force a refresh