🔥 🧵 Thread: “When Vasculitis Wears a Disguise”
Vasculitis is a shapeshifter.
It never walks into clinic saying, “Hello, I am vasculitis.”
Instead, it hides behind everyday symptoms.
Here are the common masks it wears 👇
@IhabFathiSulima @DrAkhilX @CelestinoGutirr #MedTwitter #RheumatX
Vasculitis is a shapeshifter.
It never walks into clinic saying, “Hello, I am vasculitis.”
Instead, it hides behind everyday symptoms.
Here are the common masks it wears 👇
@IhabFathiSulima @DrAkhilX @CelestinoGutirr #MedTwitter #RheumatX
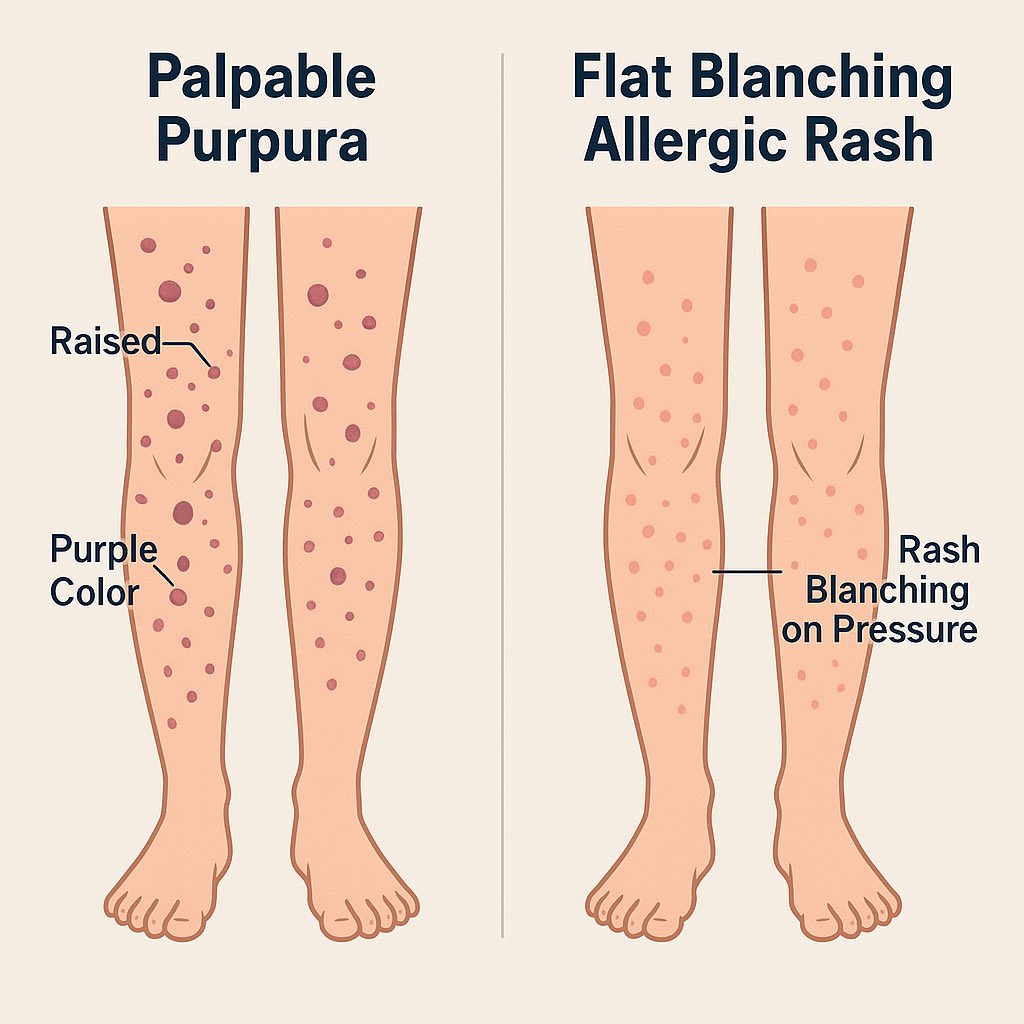
1. Just a rash?
Palpable purpura on the legs may look like “allergy.”
But when it’s non-blanching, raised, and painful → small-vessel vasculitis should be suspected.
Palpable purpura on the legs may look like “allergy.”
But when it’s non-blanching, raised, and painful → small-vessel vasculitis should be suspected.
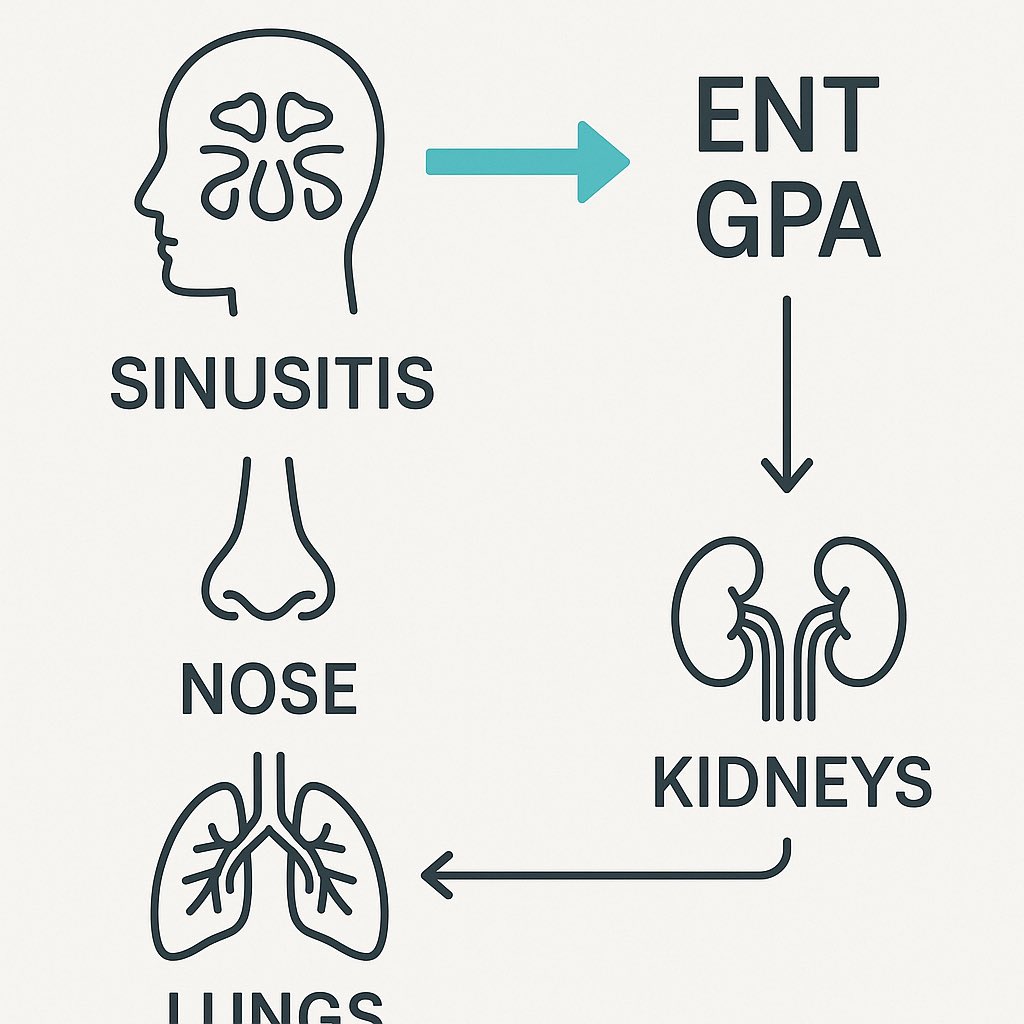
2. Just sinusitis?
Recurrent sinusitis, ear infections, or epistaxis might be ENT’s problem.
But add hematuria or lung shadows, and GPA (Granulomatosis with polyangiitis) enters the picture.
Recurrent sinusitis, ear infections, or epistaxis might be ENT’s problem.
But add hematuria or lung shadows, and GPA (Granulomatosis with polyangiitis) enters the picture.
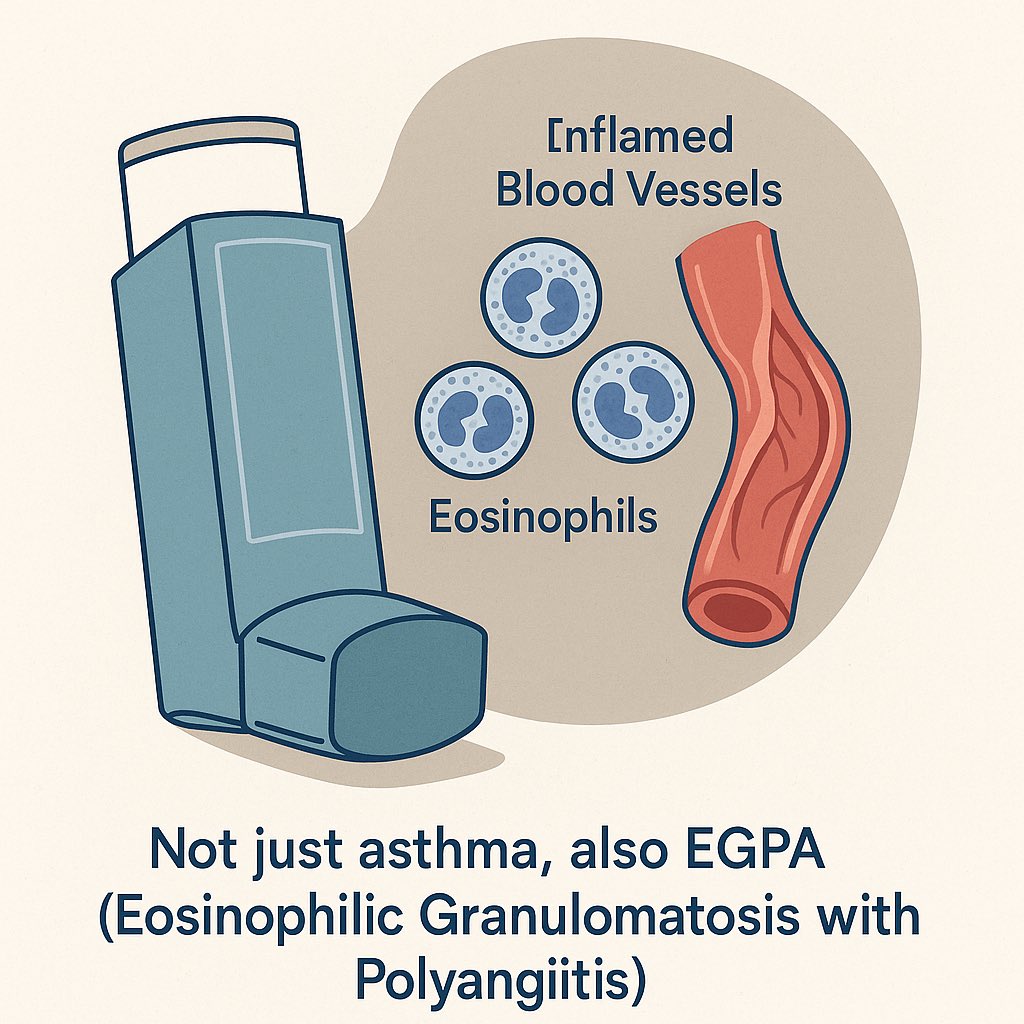
3. Just asthma?
Late-onset, steroid-dependent asthma with eosinophilia may not be “just asthma.”
It could be EGPA (Eosinophilic granulomatosis with polyangiitis).
Late-onset, steroid-dependent asthma with eosinophilia may not be “just asthma.”
It could be EGPA (Eosinophilic granulomatosis with polyangiitis).
4. Just neuropathy?
Sudden foot drop or wrist drop without trauma often signals vasculitic neuropathy (mononeuritis multiplex).
Sudden foot drop or wrist drop without trauma often signals vasculitic neuropathy (mononeuritis multiplex).

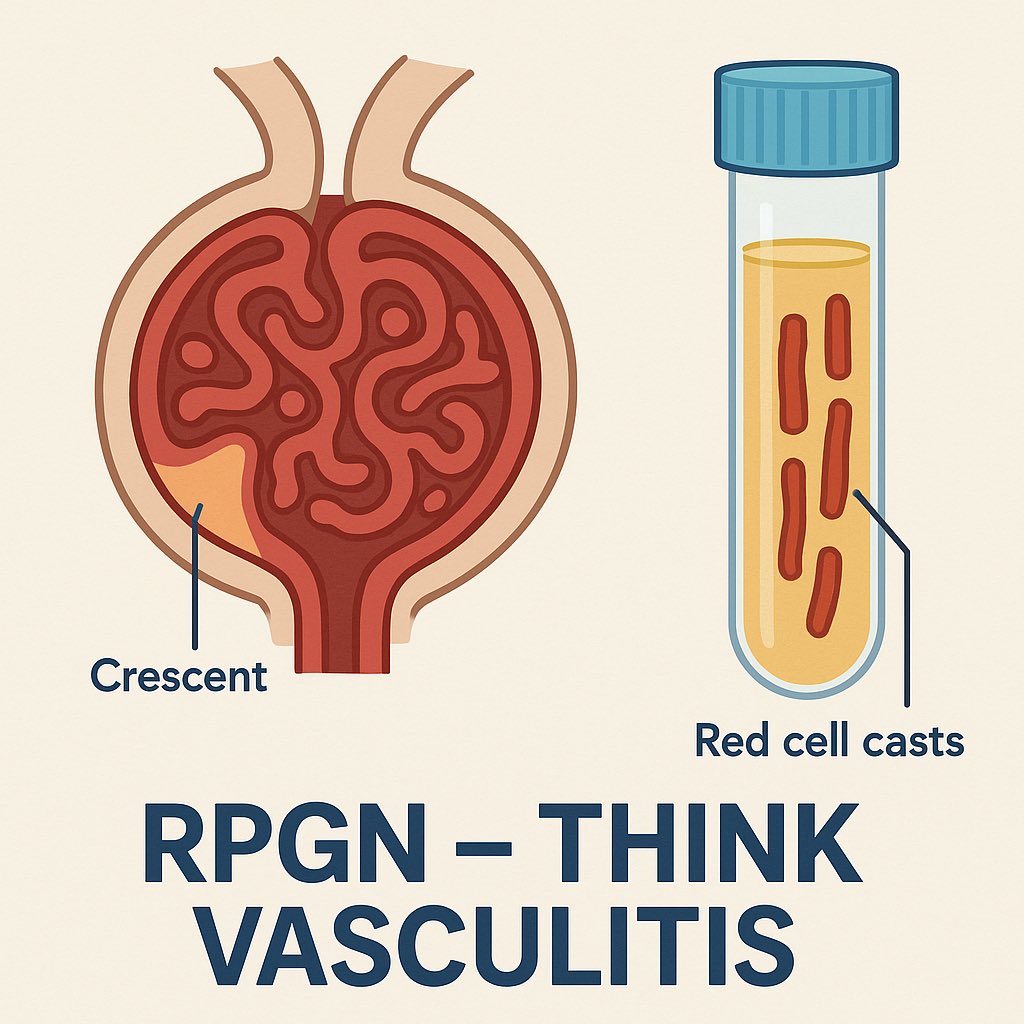
5. Just kidney disease?
Rapidly progressive renal failure with RBC casts in urine = a red flag for ANCA-associated vasculitis.
Rapidly progressive renal failure with RBC casts in urine = a red flag for ANCA-associated vasculitis.
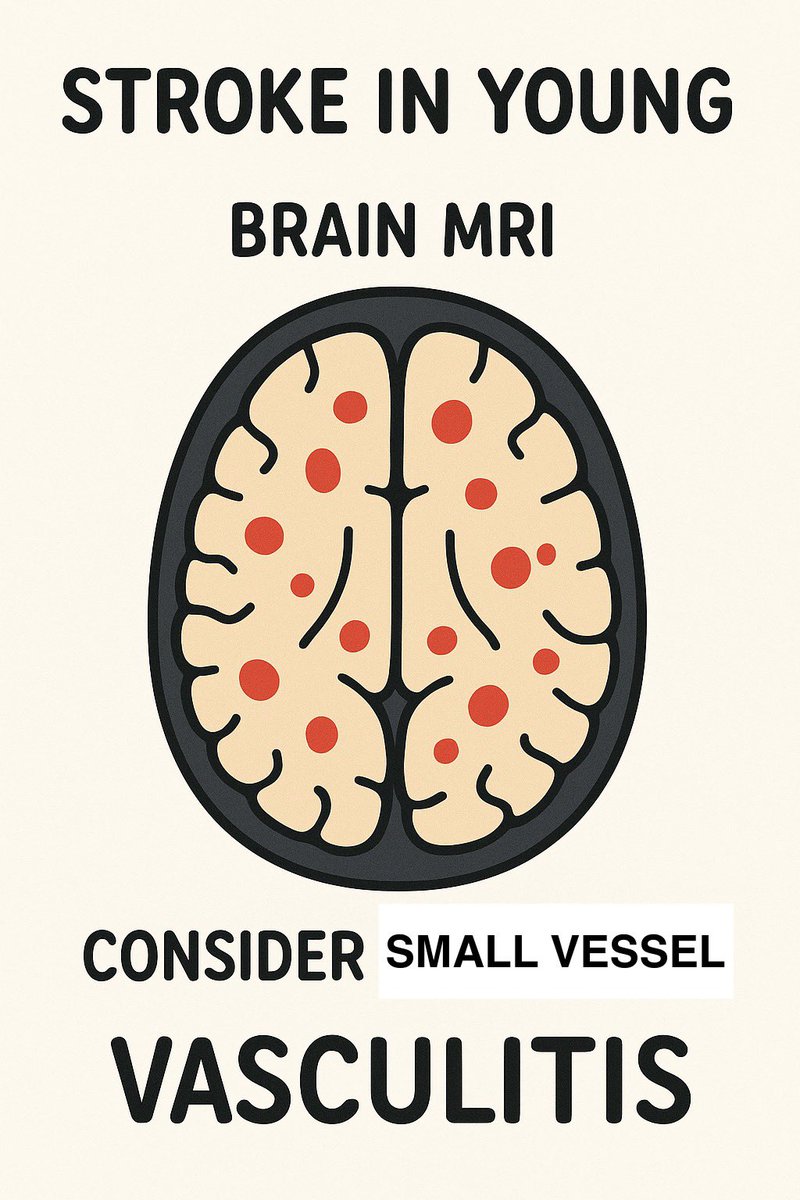
6. Just stroke in the young?
Infarcts in multiple territories or with systemic features → think primary angiitis of CNS or systemic vasculitis.
Infarcts in multiple territories or with systemic features → think primary angiitis of CNS or systemic vasculitis.
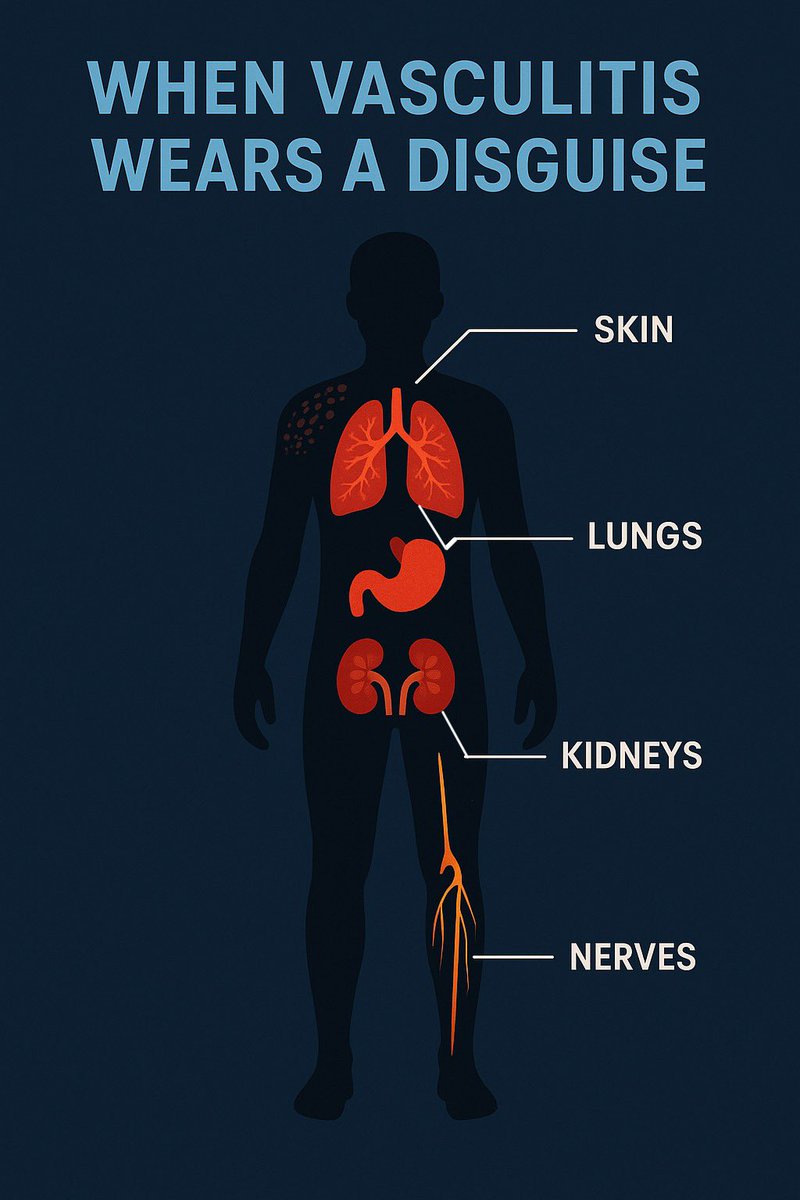
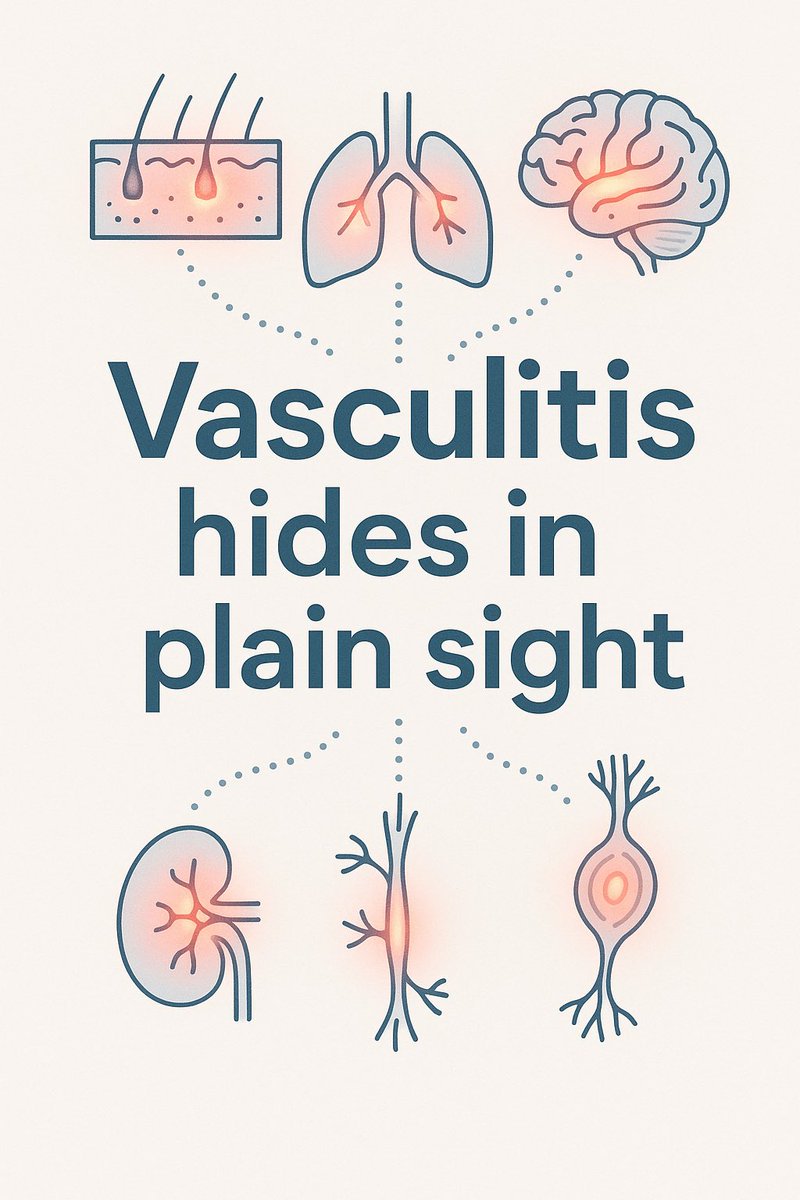
💡 Clinical pearl:
Vasculitis rarely appears in isolation.
It leaves a trail across multiple systems — skin, lungs, kidneys, nerves.
The key is to connect the dots before irreversible damage.
Vasculitis rarely appears in isolation.
It leaves a trail across multiple systems — skin, lungs, kidneys, nerves.
The key is to connect the dots before irreversible damage.
• • •
Missing some Tweet in this thread? You can try to
force a refresh