🧵 Serum Uric Acid in Rheumatology:
Tweet 1:
Serum uric acid — one of the most over-ordered and misinterpreted tests in medicine.
Here’s how to understand it in rheumatology 👇
@IhabFathiSulima @DrAkhilX @CelestinoGutirr #MedTwitter #Rheumatology
Tweet 1:
Serum uric acid — one of the most over-ordered and misinterpreted tests in medicine.
Here’s how to understand it in rheumatology 👇
@IhabFathiSulima @DrAkhilX @CelestinoGutirr #MedTwitter #Rheumatology
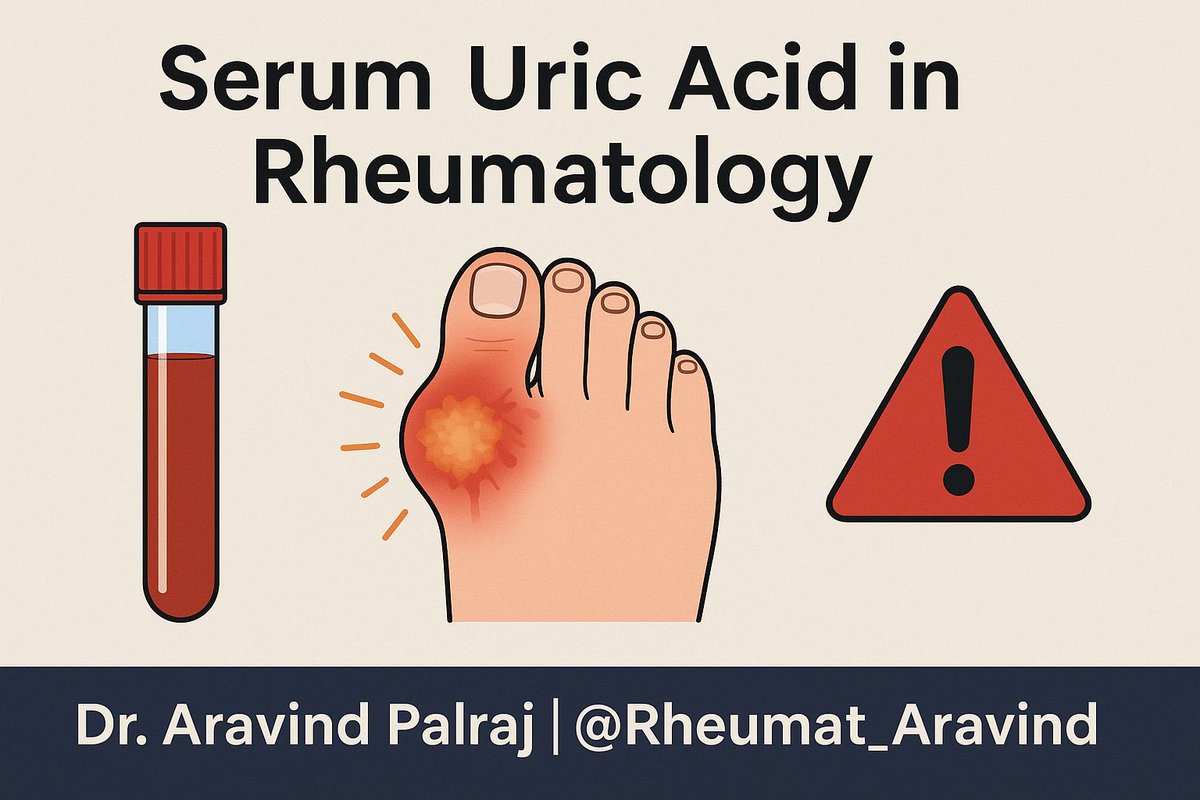
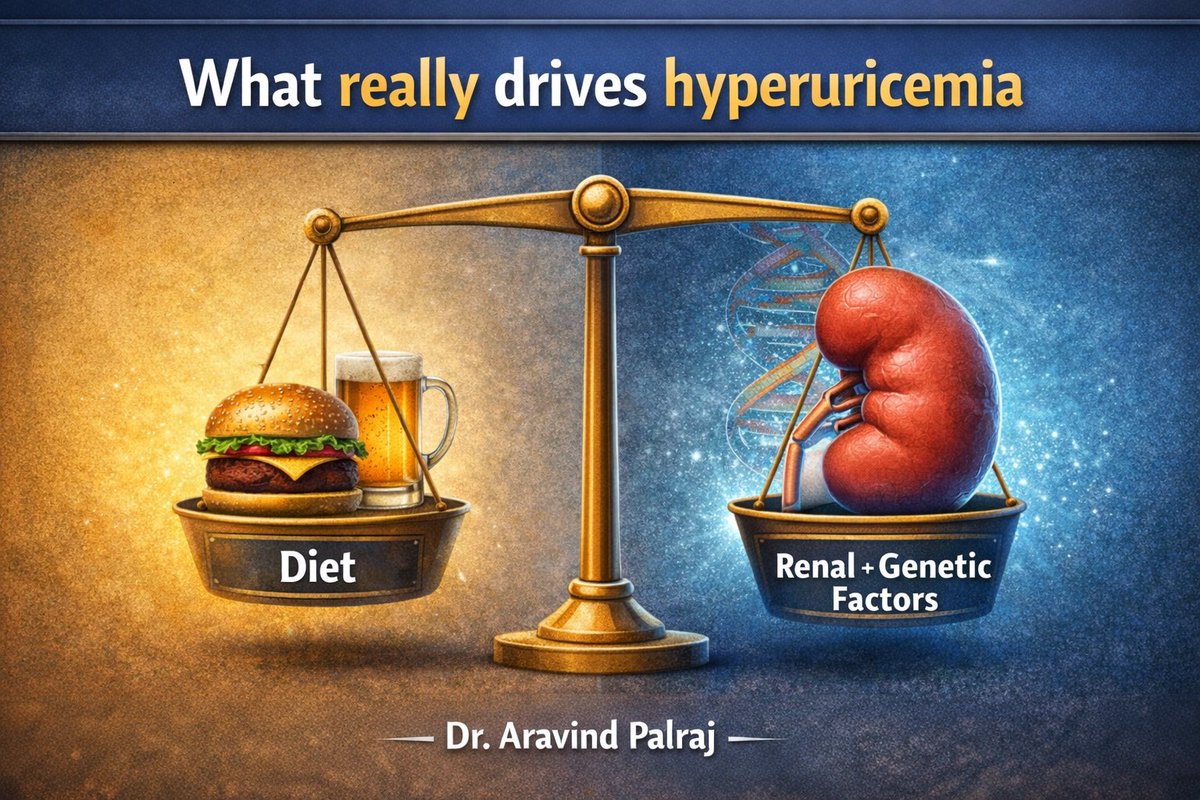
Tweet 2 (Basics):
•Uric acid = end product of purine metabolism
•Normal range: ~3.5–7 mg/dL (varies by lab/sex)
•Excreted mainly by kidneys (~70%) + gut (~30%)
•Uric acid = end product of purine metabolism
•Normal range: ~3.5–7 mg/dL (varies by lab/sex)
•Excreted mainly by kidneys (~70%) + gut (~30%)
Tweet 3 (Hyperuricemia ≠ Gout):
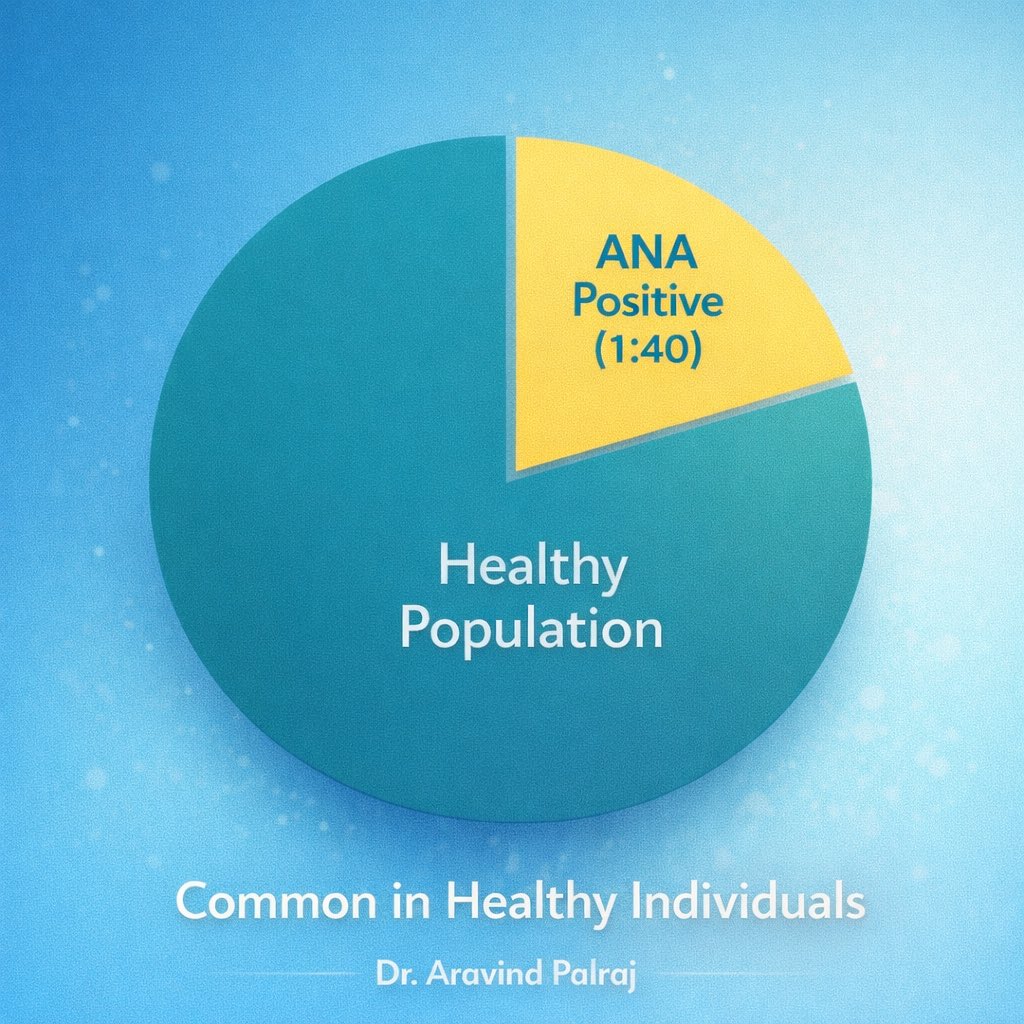
•Many people with high uric acid never develop gout
•Risk rises as uric acid >9 mg/dL
•Gout diagnosis = clinical + crystals, not just lab value
•Many people with high uric acid never develop gout
•Risk rises as uric acid >9 mg/dL
•Gout diagnosis = clinical + crystals, not just lab value
Tweet 4 (When uric acid matters):
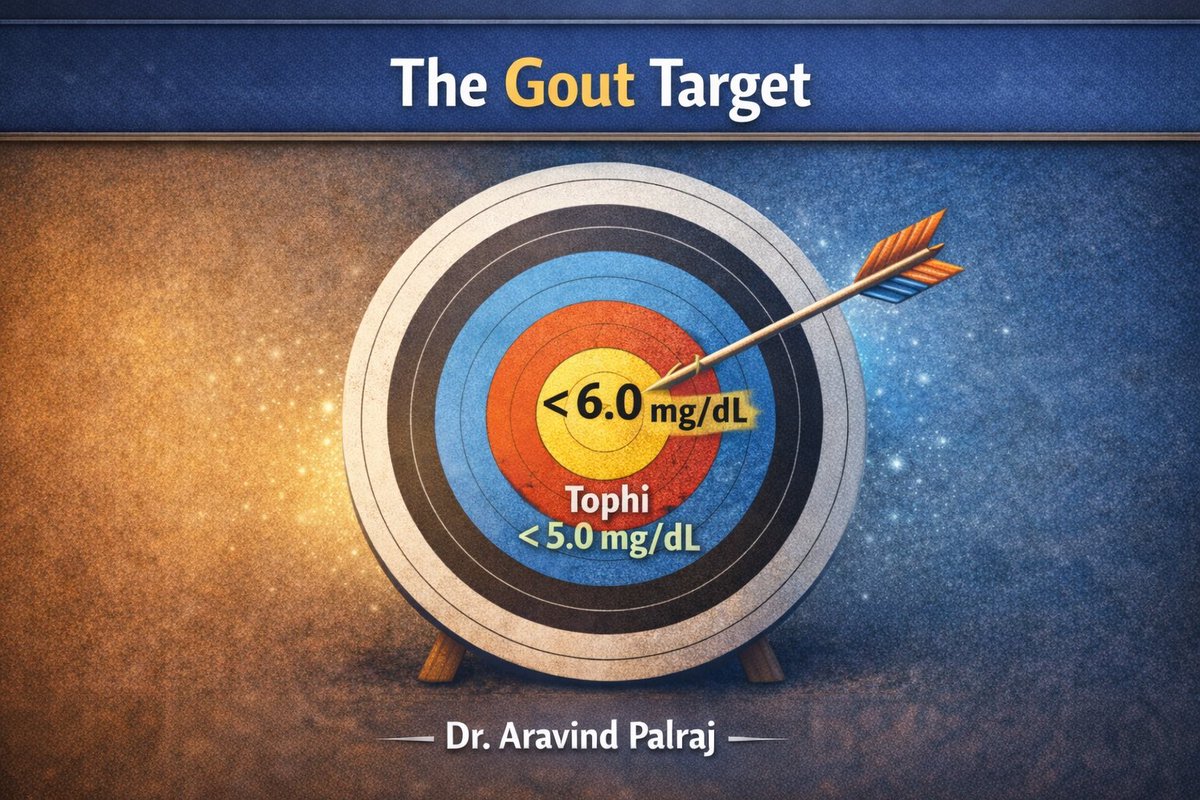
•Gout → diagnosis, flare risk, urate-lowering therapy target (<6 mg/dL)
•Tumor lysis syndrome → oncology emergency
•CKD/HTN/metabolic syndrome → marker of risk, not treatment target (usually)
•Gout → diagnosis, flare risk, urate-lowering therapy target (<6 mg/dL)
•Tumor lysis syndrome → oncology emergency
•CKD/HTN/metabolic syndrome → marker of risk, not treatment target (usually)

Tweet 5 (Pitfalls):
⚠️ Gout can occur with normal uric acid (during flare, levels may fall)
⚠️ Asymptomatic hyperuricemia often needs no treatment
⚠️ Treat the patient, not the number
⚠️ Gout can occur with normal uric acid (during flare, levels may fall)
⚠️ Asymptomatic hyperuricemia often needs no treatment
⚠️ Treat the patient, not the number
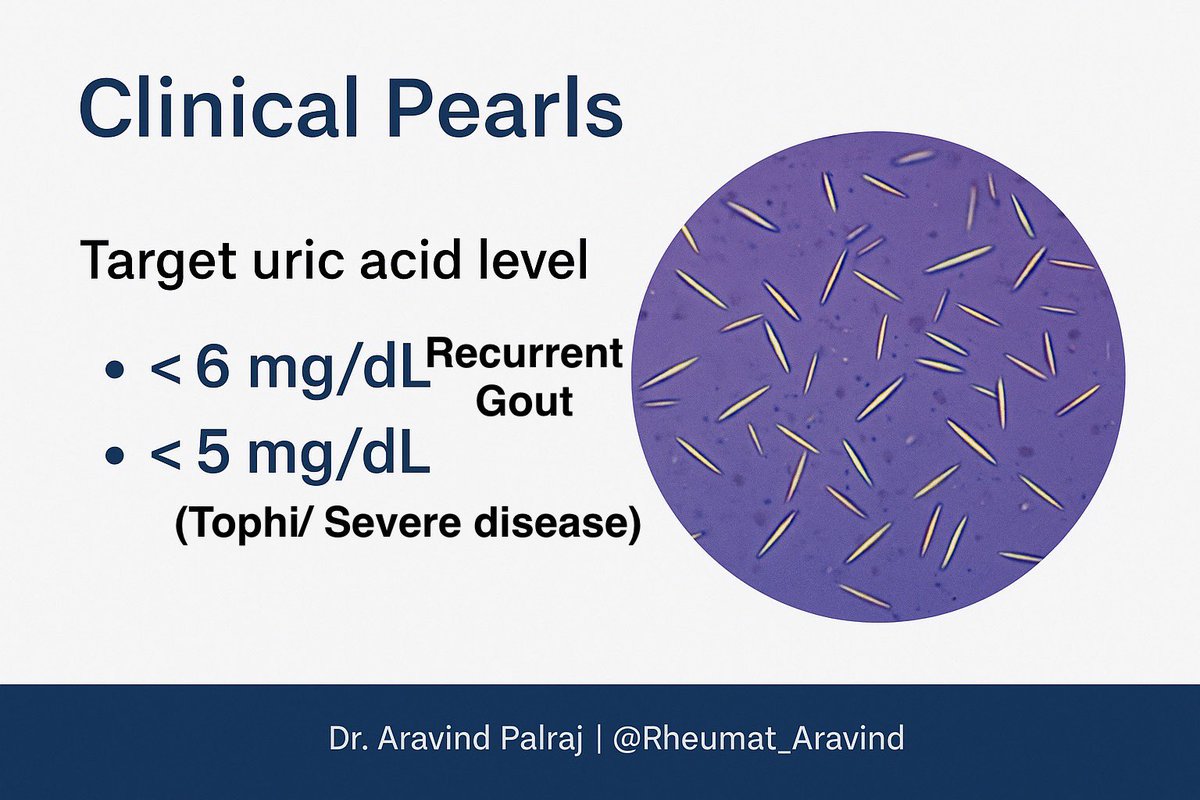
Tweet 6 (Clinical pearls):
•Always confirm gout with joint aspiration if possible
•For recurrent gout → target uric acid <6 mg/dL
•In tophi/severe disease → target <5 mg/dL
•Lifestyle (diet, alcohol, weight) helps but drugs usually needed
•Always confirm gout with joint aspiration if possible
•For recurrent gout → target uric acid <6 mg/dL
•In tophi/severe disease → target <5 mg/dL
•Lifestyle (diet, alcohol, weight) helps but drugs usually needed
Tweet 7 (Take-home):
✅ Uric acid is useful for gout management, not for screening
❌ High uric acid ≠ automatic treatment
🔑 Clinical context is everything.
✅ Uric acid is useful for gout management, not for screening
❌ High uric acid ≠ automatic treatment
🔑 Clinical context is everything.
• • •
Missing some Tweet in this thread? You can try to
force a refresh