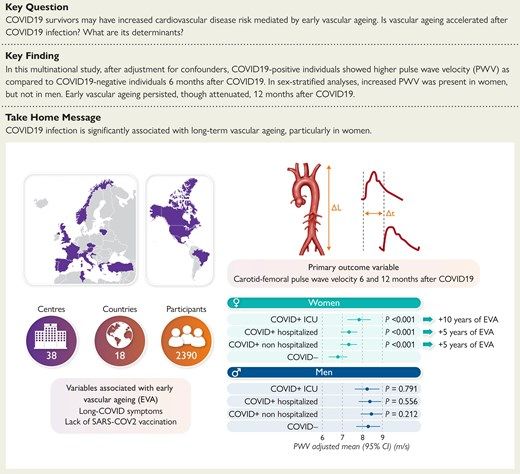
Researchers from 16 different countries recruited 2390 individuals (age 50 ± 15 years, 49.2% women) to assess the impacts of COVID-19 on vascular aging.
They found that persistent COVID-19 symptoms in women correlated with increased vascular aging.
Here is why this matters.
medpagetoday.com/cardiology/gen…
They found that persistent COVID-19 symptoms in women correlated with increased vascular aging.
Here is why this matters.
medpagetoday.com/cardiology/gen…
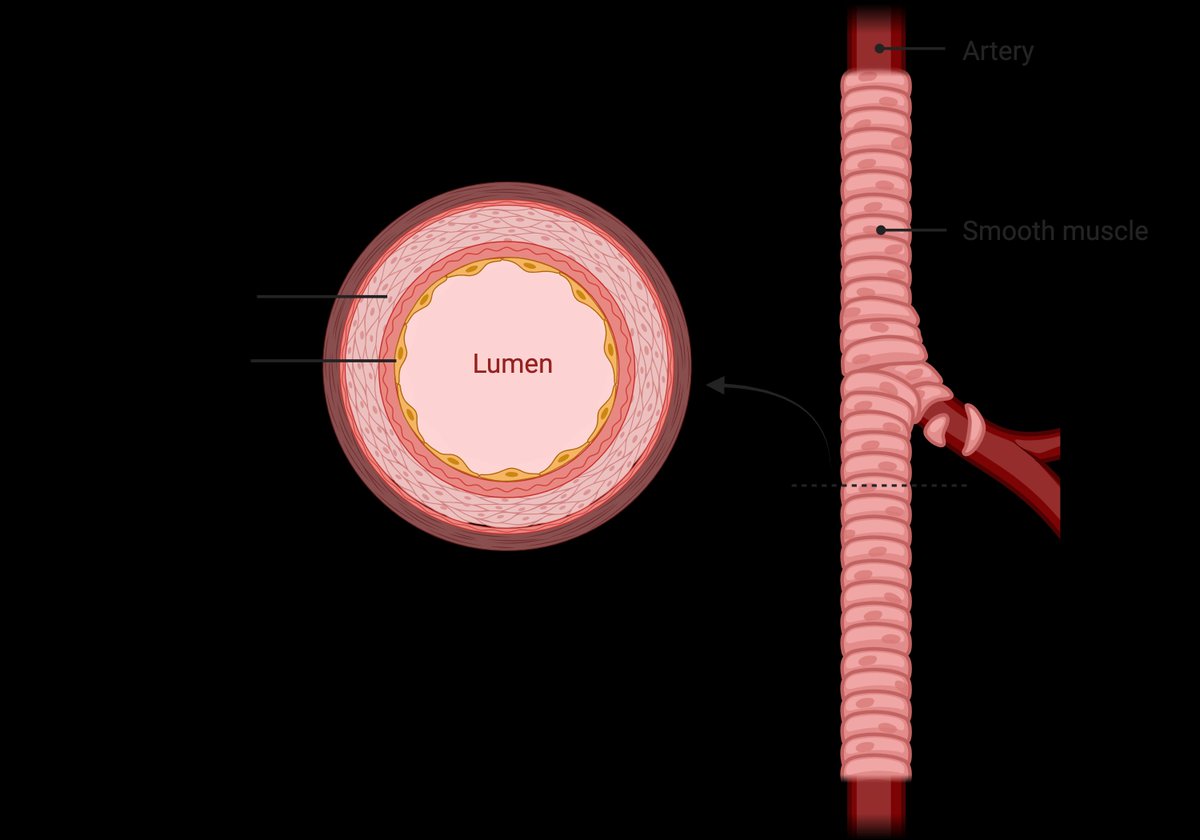
Arteries deliver oxygenated blood away from the heart.
They are surrounded by layers of cells, including smooth muscle cells (SMCs).
The diameter of the arteries expands and contracts in part due to the SMCs.
Higher O2 demand = SMC relaxation = increased artery diameter.
They are surrounded by layers of cells, including smooth muscle cells (SMCs).
The diameter of the arteries expands and contracts in part due to the SMCs.
Higher O2 demand = SMC relaxation = increased artery diameter.
When we say higher O2 demand, you're likely thinking of exercise.
But the expansion and contraction of arteries can occur at rest.
For instance, with neurovascular coupling...
But the expansion and contraction of arteries can occur at rest.
For instance, with neurovascular coupling...
Neurovascular coupling is a fancy way of saying that increased neural activity will increase blood flow to your brain.
But not your entire brain.
Here is an example.
But not your entire brain.
Here is an example.
Reading this thread is causing neurons to fire in your temporal lobe (and elsewhere).
The firing of those neurons causes potassium ions (formerly inside the neuron) to diffuse away from the neuron and bind SMCs.
This causes SMCs on nearby arteries to relax, increasing the diameter.
Increased arterial diameter = increased blood flow to the neuron(s).
Thus, neurovascular coupling helps nourish your active neurons.
The firing of those neurons causes potassium ions (formerly inside the neuron) to diffuse away from the neuron and bind SMCs.
This causes SMCs on nearby arteries to relax, increasing the diameter.
Increased arterial diameter = increased blood flow to the neuron(s).
Thus, neurovascular coupling helps nourish your active neurons.
This happens rapidly - in milliseconds.
In other words, neuron firing throughout the brain conducts a symphony of highly localized vasodilation events.
This is needed for peak 🧠 performance.
In other words, neuron firing throughout the brain conducts a symphony of highly localized vasodilation events.
This is needed for peak 🧠 performance.
Thus, vascular health is important.
But not just in the brain - your entire body.
Back to the study.
But not just in the brain - your entire body.
Back to the study.
Researchers measured arterial stiffness by calculating the speed of a pressure wave traveling from the carotid artery (neck) to the femoral artery (groin).
They adjusted for factors like age and blood pressure to enhance accuracy.
This serves as a proxy for vascular health because higher values indicate stiffer arteries.
They adjusted for factors like age and blood pressure to enhance accuracy.
This serves as a proxy for vascular health because higher values indicate stiffer arteries.
The researchers stratified the data by sex.
Males showed no significant difference in arterial stiffness.
However, women with persistent COVID-19-like symptoms had a higher pressure wave velocity (proxy for stiffer arteries).
Even mild C-19 increased stiffness.
A 12-month follow-up found a slight reduction in stiffness.
Full study:
academic.oup.com/eurheartj/adva…
Males showed no significant difference in arterial stiffness.
However, women with persistent COVID-19-like symptoms had a higher pressure wave velocity (proxy for stiffer arteries).
Even mild C-19 increased stiffness.
A 12-month follow-up found a slight reduction in stiffness.
Full study:
academic.oup.com/eurheartj/adva…
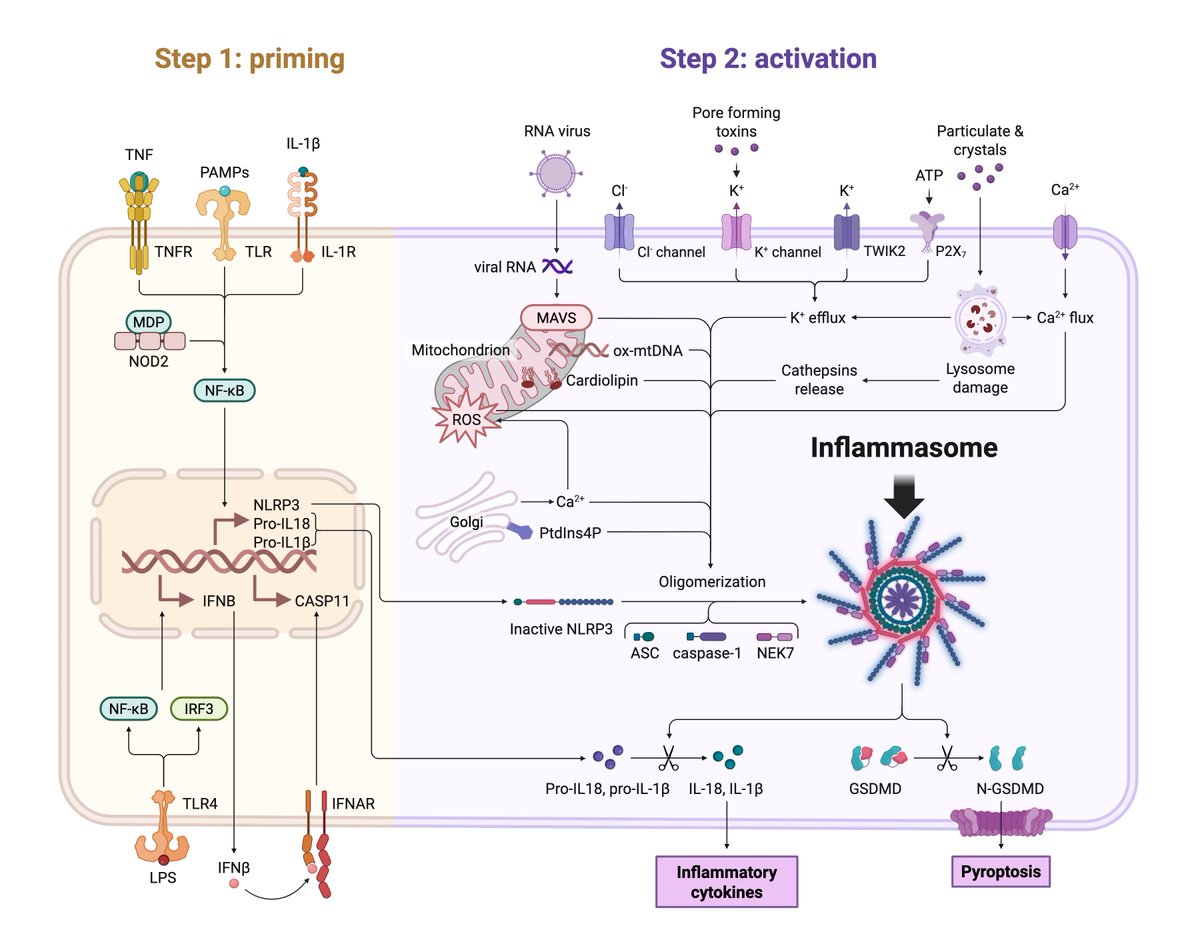
This stiffness is likely caused by endothelial cell dysfunction and vascular inflammation.
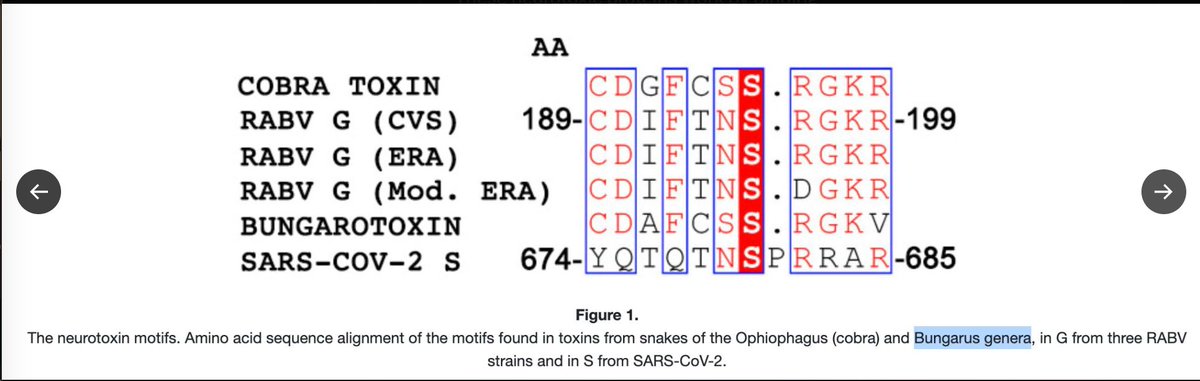
There are hints that SARS-CoV-2 can dysregulate vascular smooth muscle cell function, but more data are needed (1).
Leave a comment below - we want to hear from you.
There are hints that SARS-CoV-2 can dysregulate vascular smooth muscle cell function, but more data are needed (1).
Leave a comment below - we want to hear from you.
Literature Cited:
1. Pelisek J, et al. Clin Sci (Lond). 2022 Nov 11;136(21):1571-1590. PMID: 36367091.
1. Pelisek J, et al. Clin Sci (Lond). 2022 Nov 11;136(21):1571-1590. PMID: 36367091.
• • •
Missing some Tweet in this thread? You can try to
force a refresh