
We are organizing a coordinated research effort to revolutionize the diagnosis and treatment of #neuroinflammation illnesses and #mentalhealth symptoms.
11 subscribers
How to get URL link on X (Twitter) App


 Between March 2020 and August 2024, 3 out of 151 prescreened pediatric COVID-19 patients developed obsessive-compulsive disorder (OCD) after infection.
Between March 2020 and August 2024, 3 out of 151 prescreened pediatric COVID-19 patients developed obsessive-compulsive disorder (OCD) after infection.
 French and South African researchers isolated blood samples from:
French and South African researchers isolated blood samples from:

 Scientists recruited:
Scientists recruited: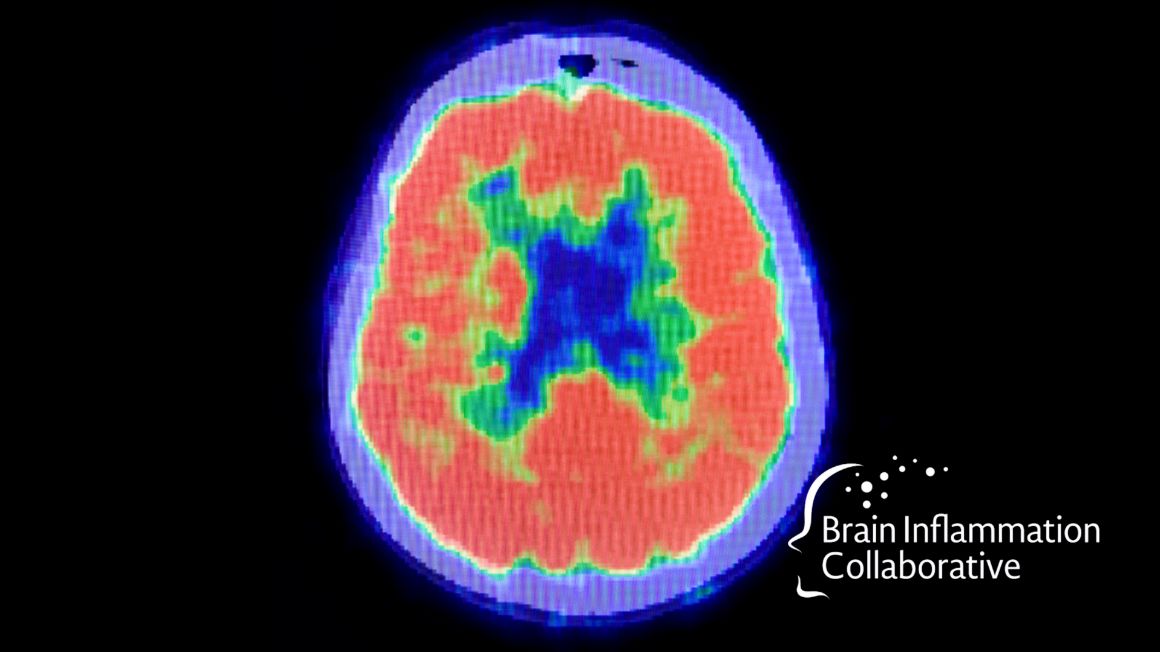
 Researchers from Ian Lipkin's Lab at Columbia University (and others) recruited:
Researchers from Ian Lipkin's Lab at Columbia University (and others) recruited: 

 Dr. Leonard Weinstock, in collaboration with a group of other prominent researchers, used questionnaires from:
Dr. Leonard Weinstock, in collaboration with a group of other prominent researchers, used questionnaires from:
 Researchers from Cornell University sequenced the cell-free ribonucleic acid (cfRNA) from the blood of:
Researchers from Cornell University sequenced the cell-free ribonucleic acid (cfRNA) from the blood of: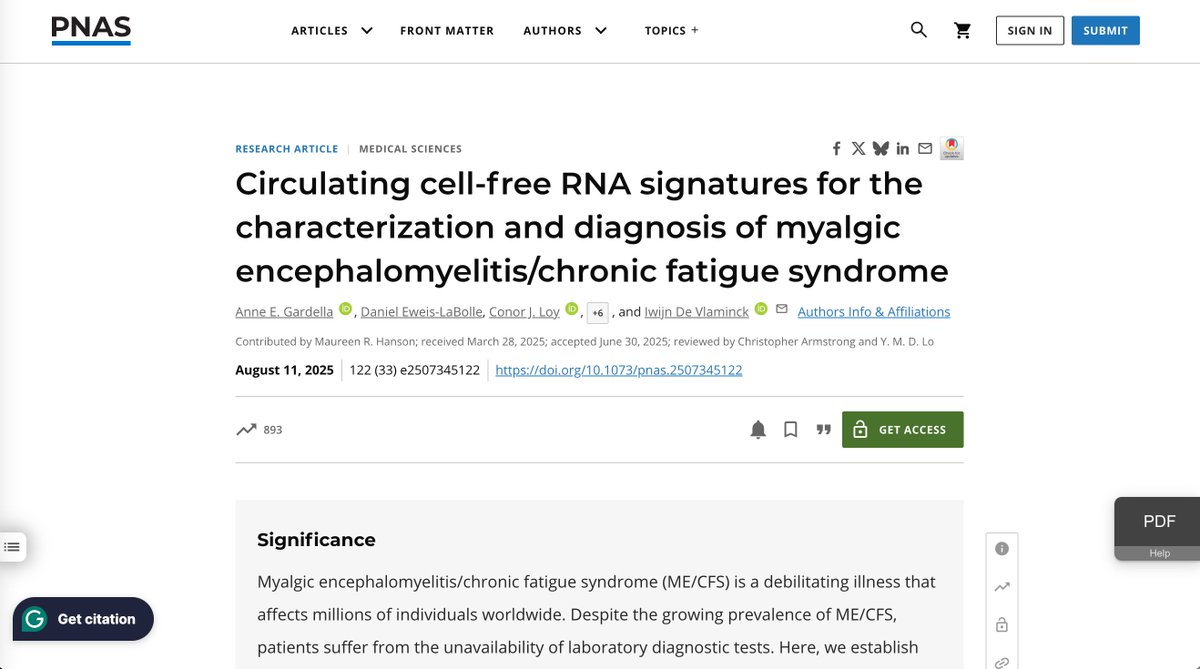
 🧠 The Kynurenine Pathway Background
🧠 The Kynurenine Pathway Background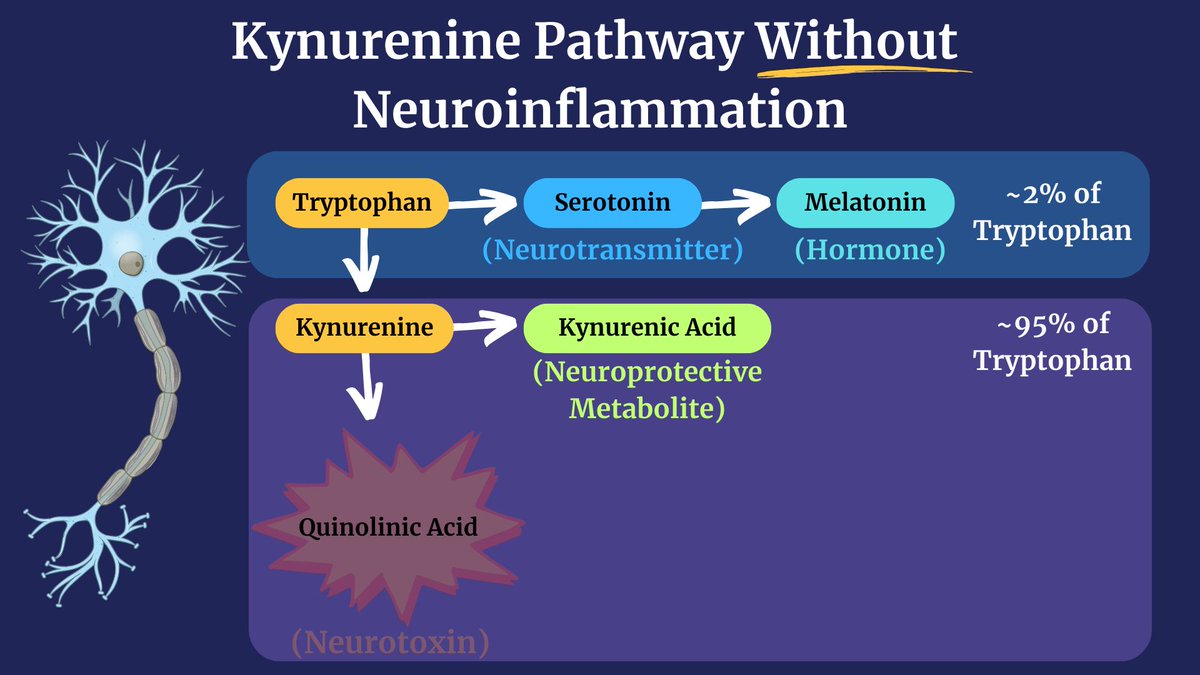

 Researchers from 16 different countries recruited 2390 individuals (age 50 ± 15 years, 49.2% women) to assess the impacts of COVID-19 on vascular aging.
Researchers from 16 different countries recruited 2390 individuals (age 50 ± 15 years, 49.2% women) to assess the impacts of COVID-19 on vascular aging. 
 Research from Dr. Sonya Marshall-Gradisnik in Brisbane, Australia, verified that Long COVID patients, like ME/CFS patients, have a dysfunctional calcium ion channel called TRPM3(1).
Research from Dr. Sonya Marshall-Gradisnik in Brisbane, Australia, verified that Long COVID patients, like ME/CFS patients, have a dysfunctional calcium ion channel called TRPM3(1).

 But first, a disclaimer.
But first, a disclaimer.


 South Korean researchers found that two FDA-approved drugs can reverse these repetitive movements:
South Korean researchers found that two FDA-approved drugs can reverse these repetitive movements:

 "More than 80% of [systemic autoimmune rheumatic disease] patients reported that having their symptoms dismissed as... psychological, along with comments like "it's in your head," harmed their self-worth. For 72%, the experience remained upsetting even decades later."
"More than 80% of [systemic autoimmune rheumatic disease] patients reported that having their symptoms dismissed as... psychological, along with comments like "it's in your head," harmed their self-worth. For 72%, the experience remained upsetting even decades later."

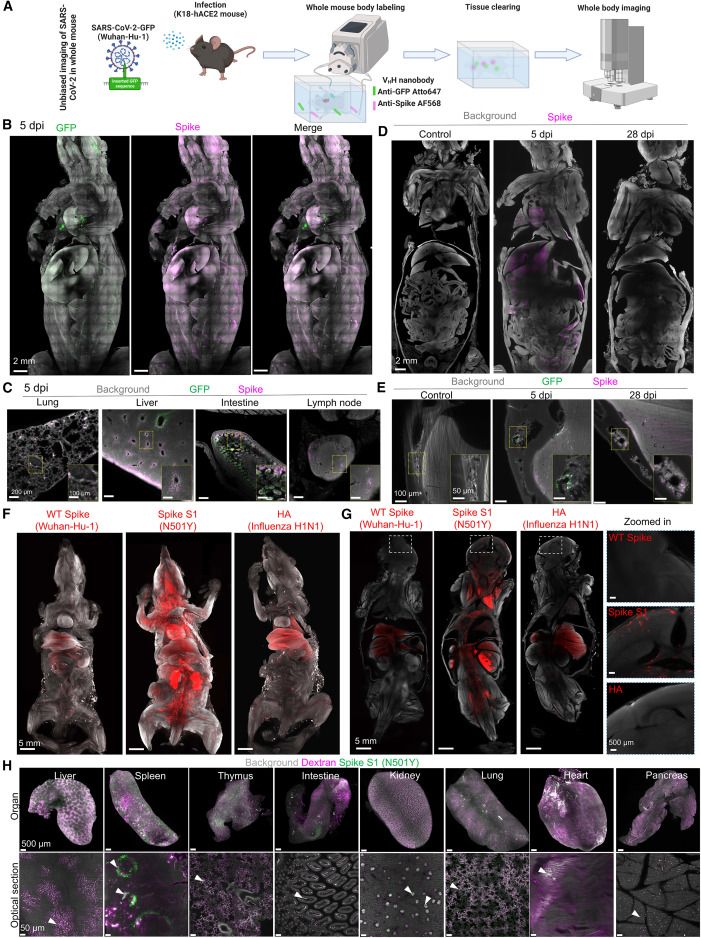
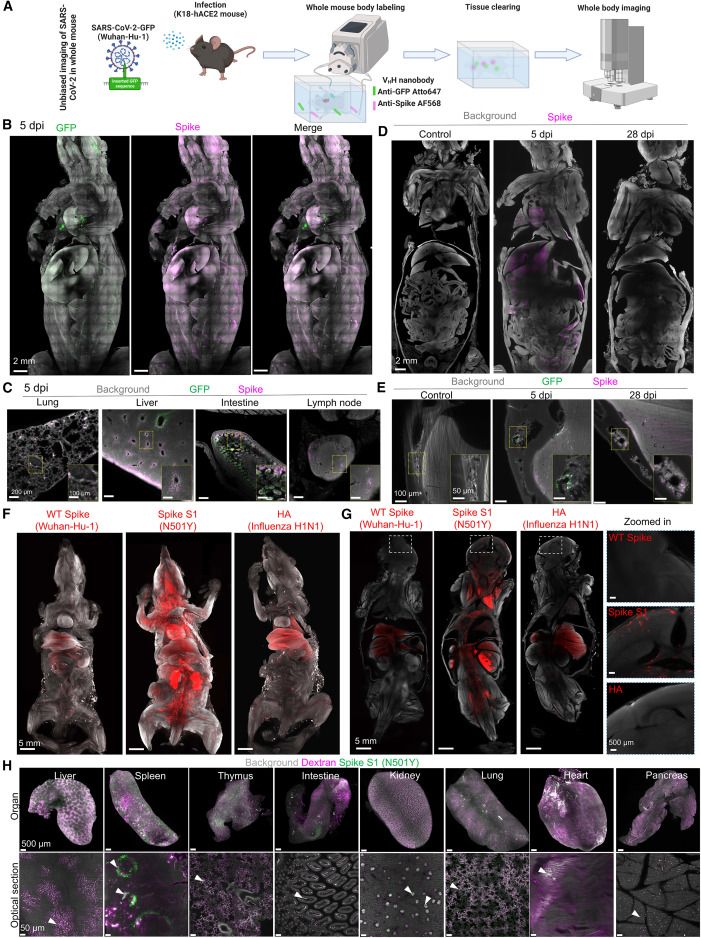
 To understand the nicotine hypothesis, we must start with the spike protein.
To understand the nicotine hypothesis, we must start with the spike protein.


 🧠 Psychosis & Autoantibodies:
🧠 Psychosis & Autoantibodies:
 Researchers believe they have identified a cause of TRD: chronic inflammation.
Researchers believe they have identified a cause of TRD: chronic inflammation.

 \ The Study:
\ The Study:

 Being a kid today is hard enough.
Being a kid today is hard enough. 