🧵 Serum ACE in Rheumatology:
One of the most debated biomarkers.
Ordered often, misinterpreted even more.
Let’s clear the confusion 👇
#Rheumatology #Sarcoidosis #Biomarkers @IhabFathiSulima @DrAkhilX @CelestinoGutirr
One of the most debated biomarkers.
Ordered often, misinterpreted even more.
Let’s clear the confusion 👇
#Rheumatology #Sarcoidosis #Biomarkers @IhabFathiSulima @DrAkhilX @CelestinoGutirr
1/
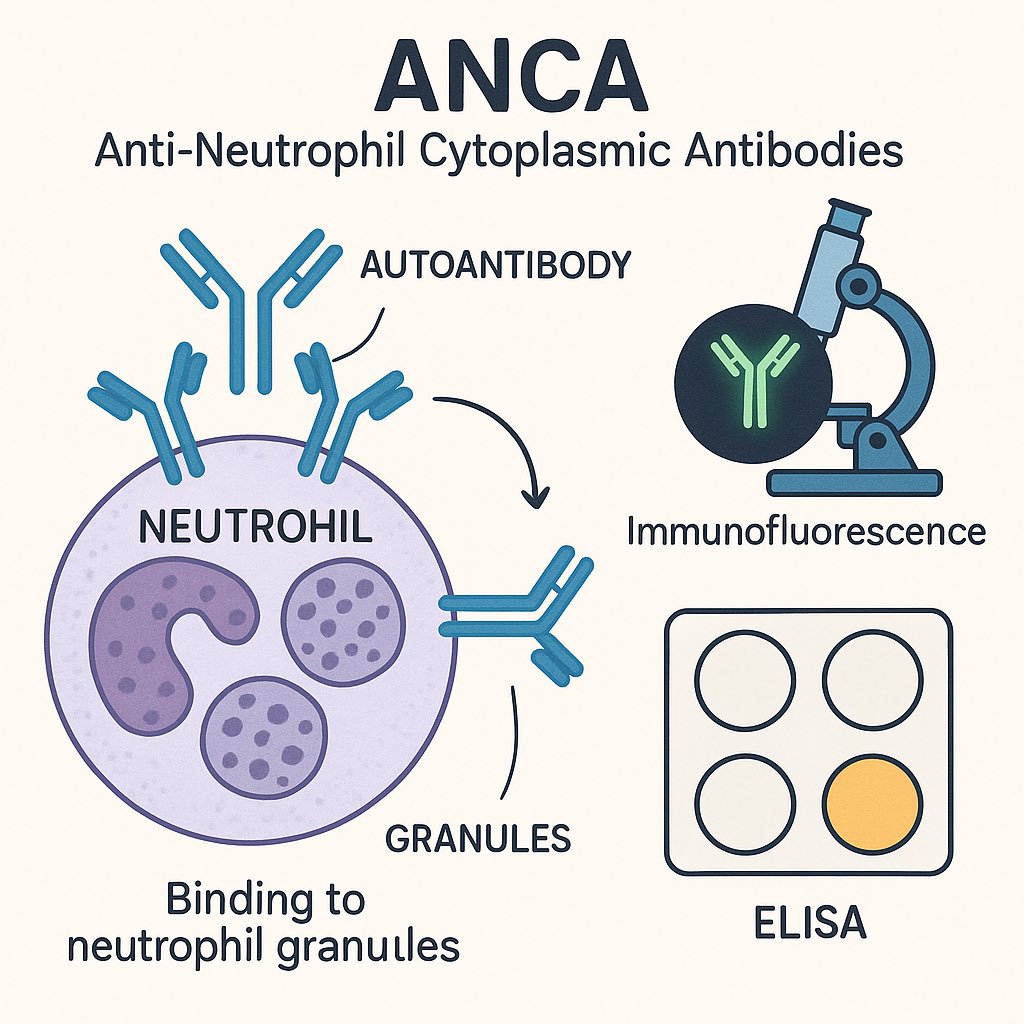
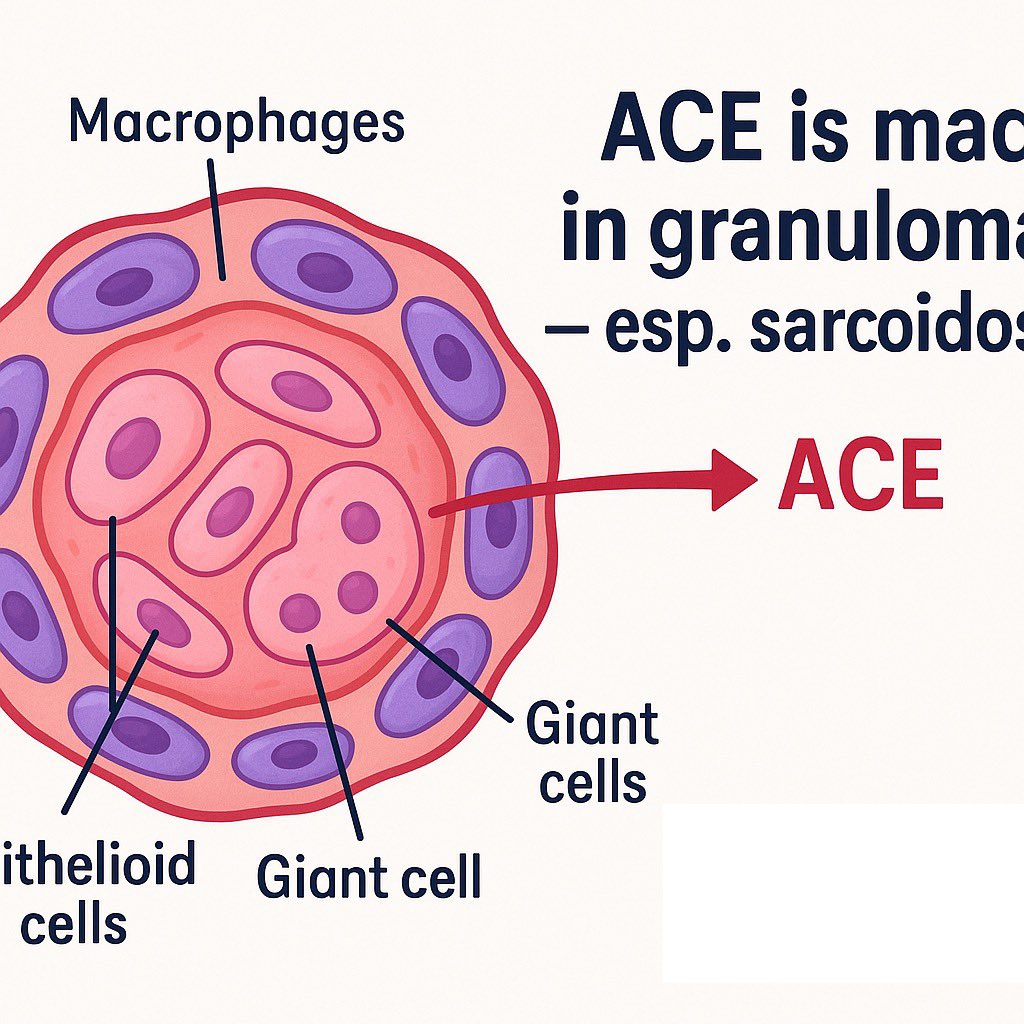
🔬 Serum ACE is produced by epithelioid cells in granulomas.
Hence, levels may be elevated in granulomatous diseases — especially sarcoidosis.
🔬 Serum ACE is produced by epithelioid cells in granulomas.
Hence, levels may be elevated in granulomatous diseases — especially sarcoidosis.
2/
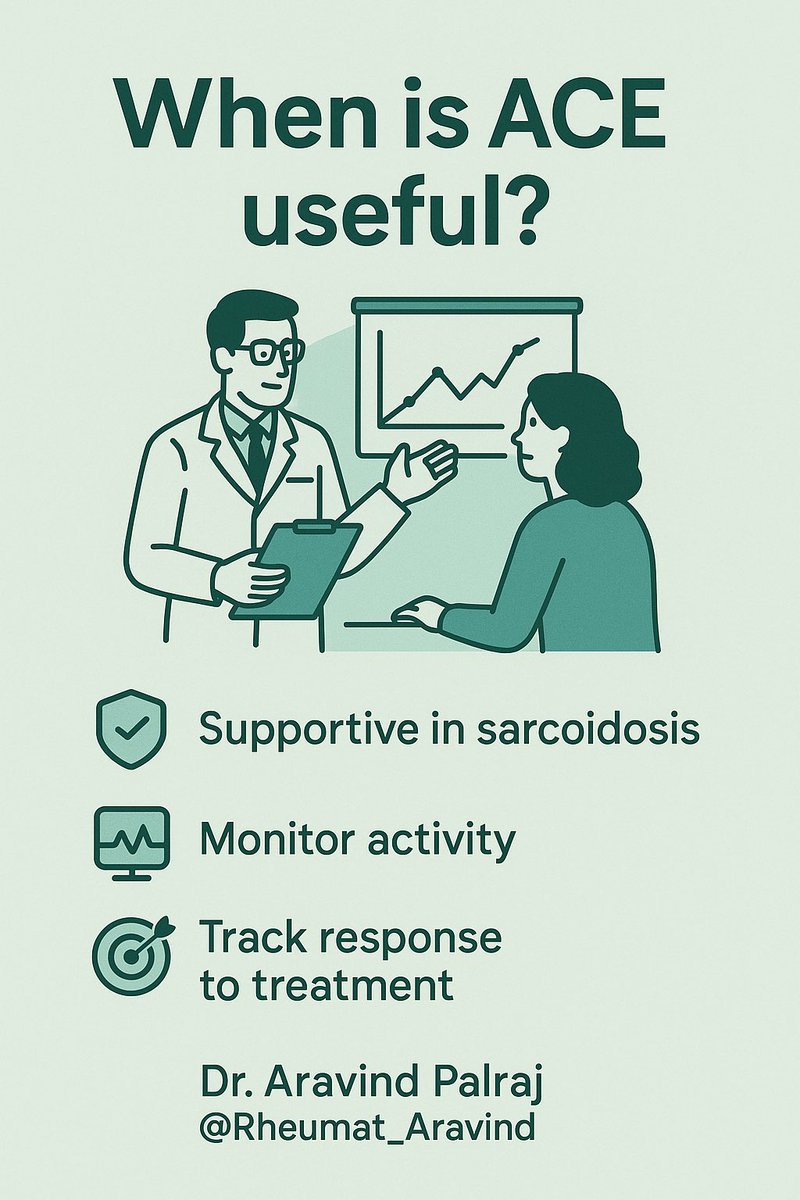
📊 When is ACE useful?
•Supporting diagnosis of sarcoidosis (not diagnostic alone)
•Monitoring disease activity (trend > absolute value)
•May fall with treatment response
📊 When is ACE useful?
•Supporting diagnosis of sarcoidosis (not diagnostic alone)
•Monitoring disease activity (trend > absolute value)
•May fall with treatment response
3/
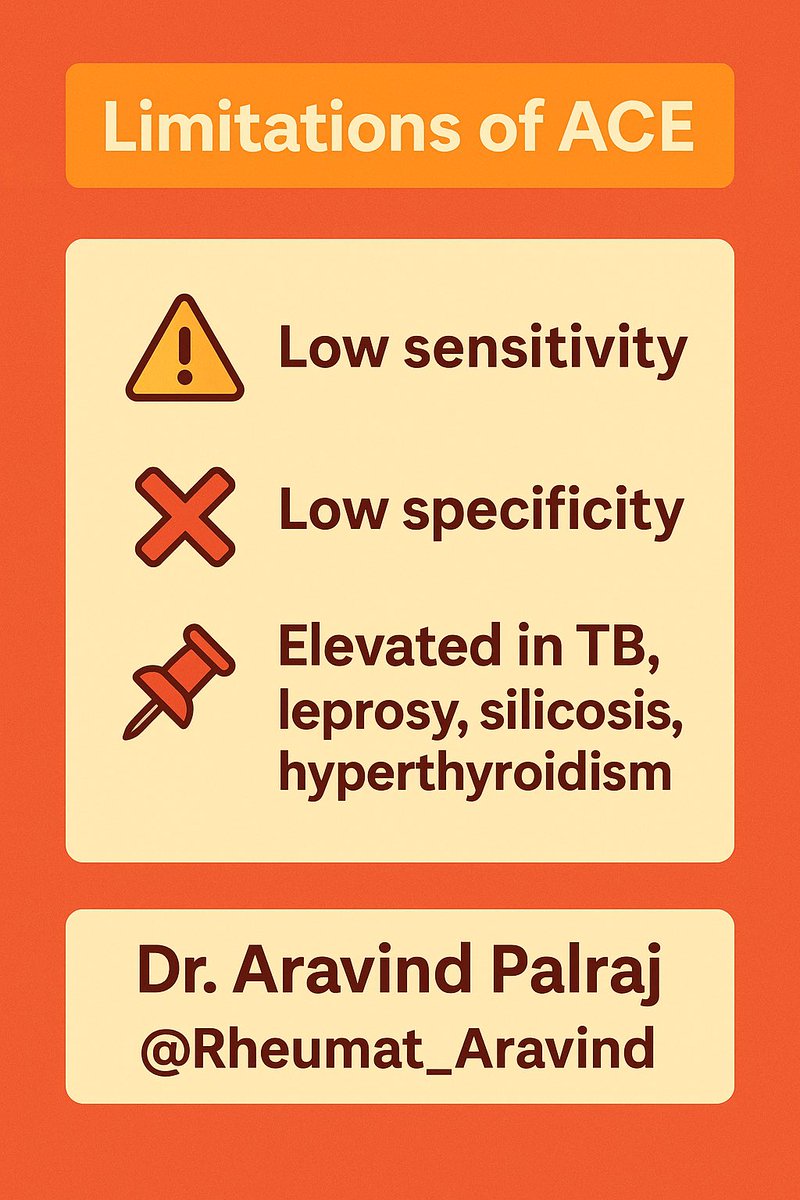
⚠️ Limitations:
•Low sensitivity (40–60%)
•Low specificity — elevated in TB, leprosy, silicosis, berylliosis, histoplasmosis, even hyperthyroidism
•Normal ACE does not exclude sarcoidosis
⚠️ Limitations:
•Low sensitivity (40–60%)
•Low specificity — elevated in TB, leprosy, silicosis, berylliosis, histoplasmosis, even hyperthyroidism
•Normal ACE does not exclude sarcoidosis
4/
🧪 Practical notes:
•Always correlate with clinical + imaging (esp. CXR/HRCT)
•Repeatable for follow-up but avoid over-reliance
•Genetic ACE polymorphisms can affect baseline levels
🧪 Practical notes:
•Always correlate with clinical + imaging (esp. CXR/HRCT)
•Repeatable for follow-up but avoid over-reliance
•Genetic ACE polymorphisms can affect baseline levels
5/
✅ Take-home:
Serum ACE is a supportive biomarker, not a stand-alone test.
Use it for trends in known sarcoidosis, not as a universal screening tool.
✅ Take-home:
Serum ACE is a supportive biomarker, not a stand-alone test.
Use it for trends in known sarcoidosis, not as a universal screening tool.
• • •
Missing some Tweet in this thread? You can try to
force a refresh