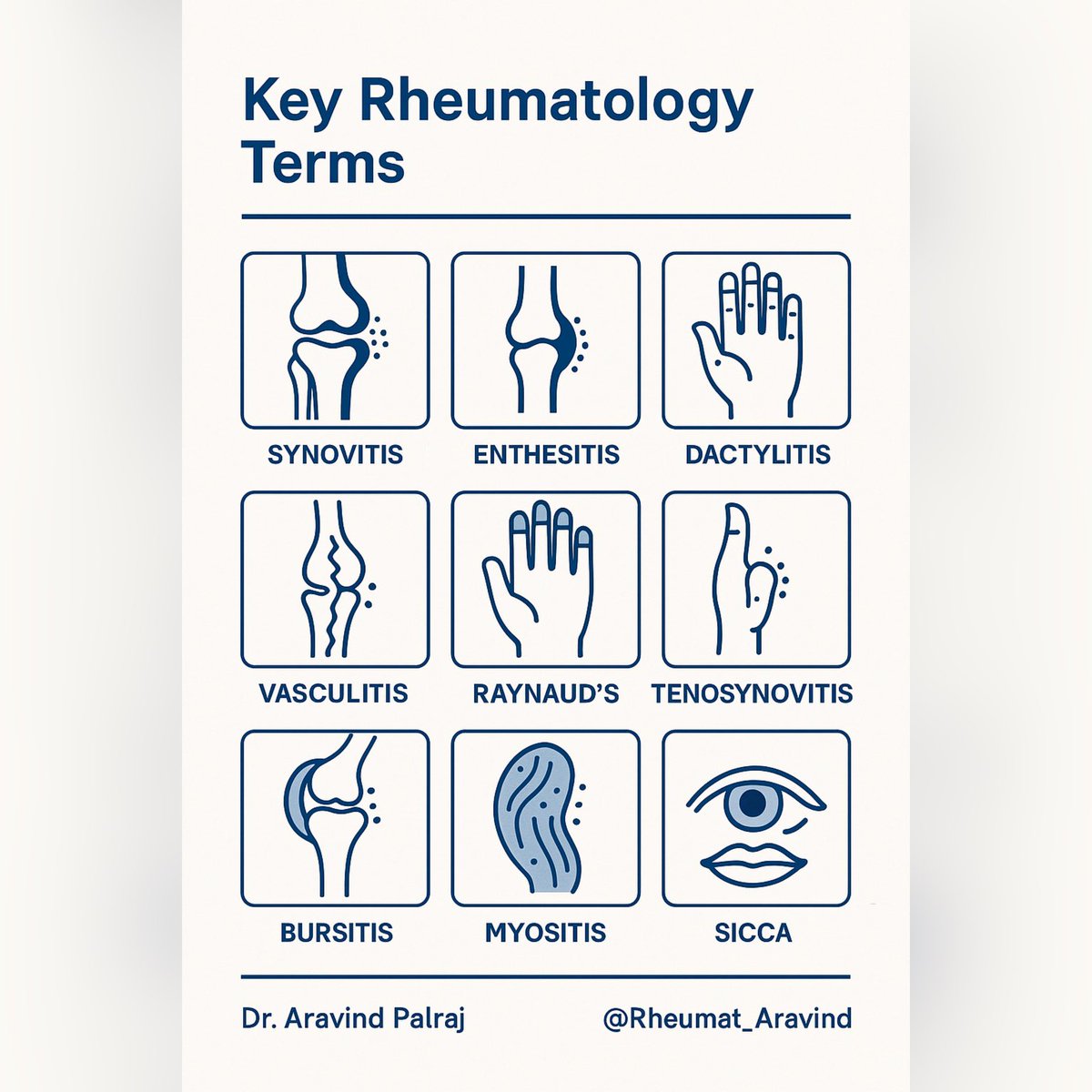
🧵 Key Terms in Rheumatology — Simplified & Explained ⬇️
Rheumatology is full of terms like synovitis, enthesitis, tenosynovitis, dactylitis.
Let’s break them down in a clear way
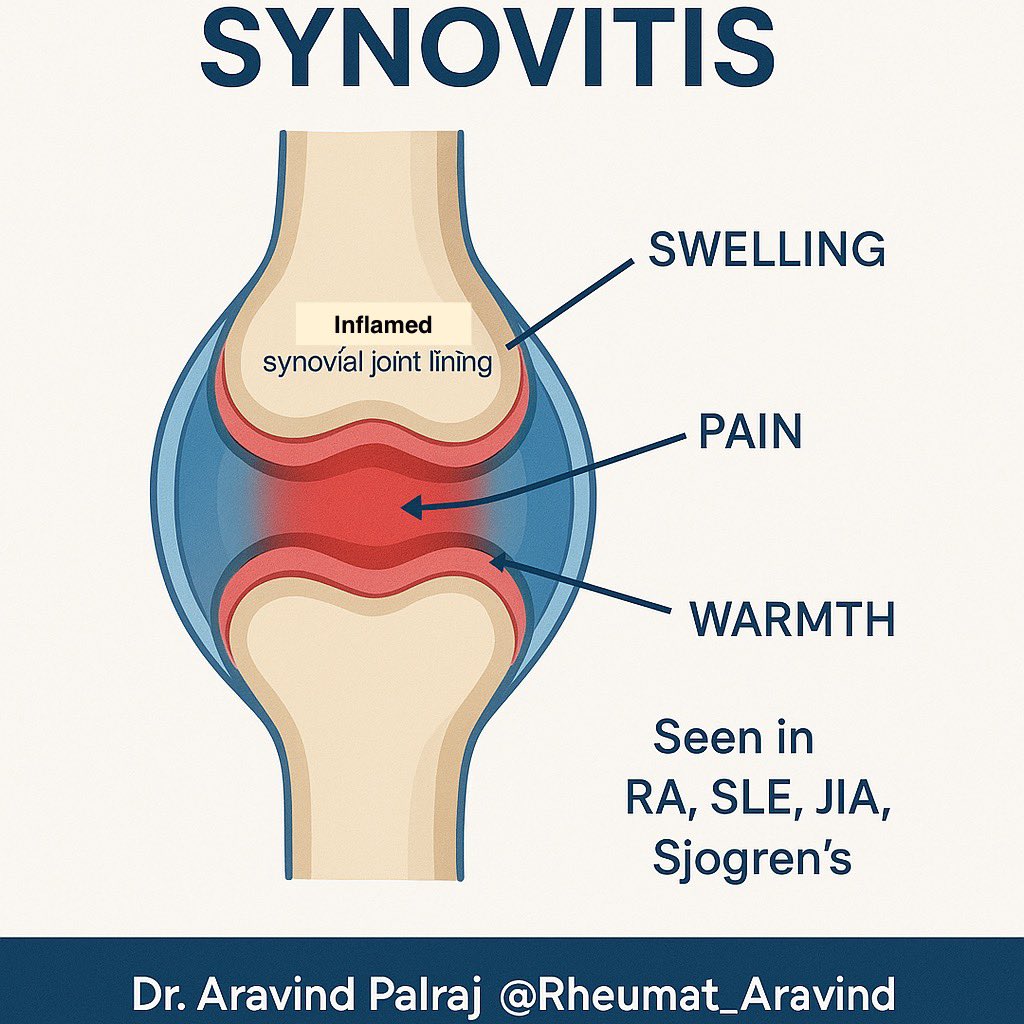
1️⃣ Synovitis
= Inflammation of the synovial lining of a joint.
Signs: swelling, warmth, tenderness, ↓ ROM.
Seen in: RA, lupus arthritis, JIA.
Think: “the joint lining is angry.”
@DrAkhilX @IhabFathiSulima #MedTwitter #RheumatTwitter
Rheumatology is full of terms like synovitis, enthesitis, tenosynovitis, dactylitis.
Let’s break them down in a clear way
1️⃣ Synovitis
= Inflammation of the synovial lining of a joint.
Signs: swelling, warmth, tenderness, ↓ ROM.
Seen in: RA, lupus arthritis, JIA.
Think: “the joint lining is angry.”
@DrAkhilX @IhabFathiSulima #MedTwitter #RheumatTwitter
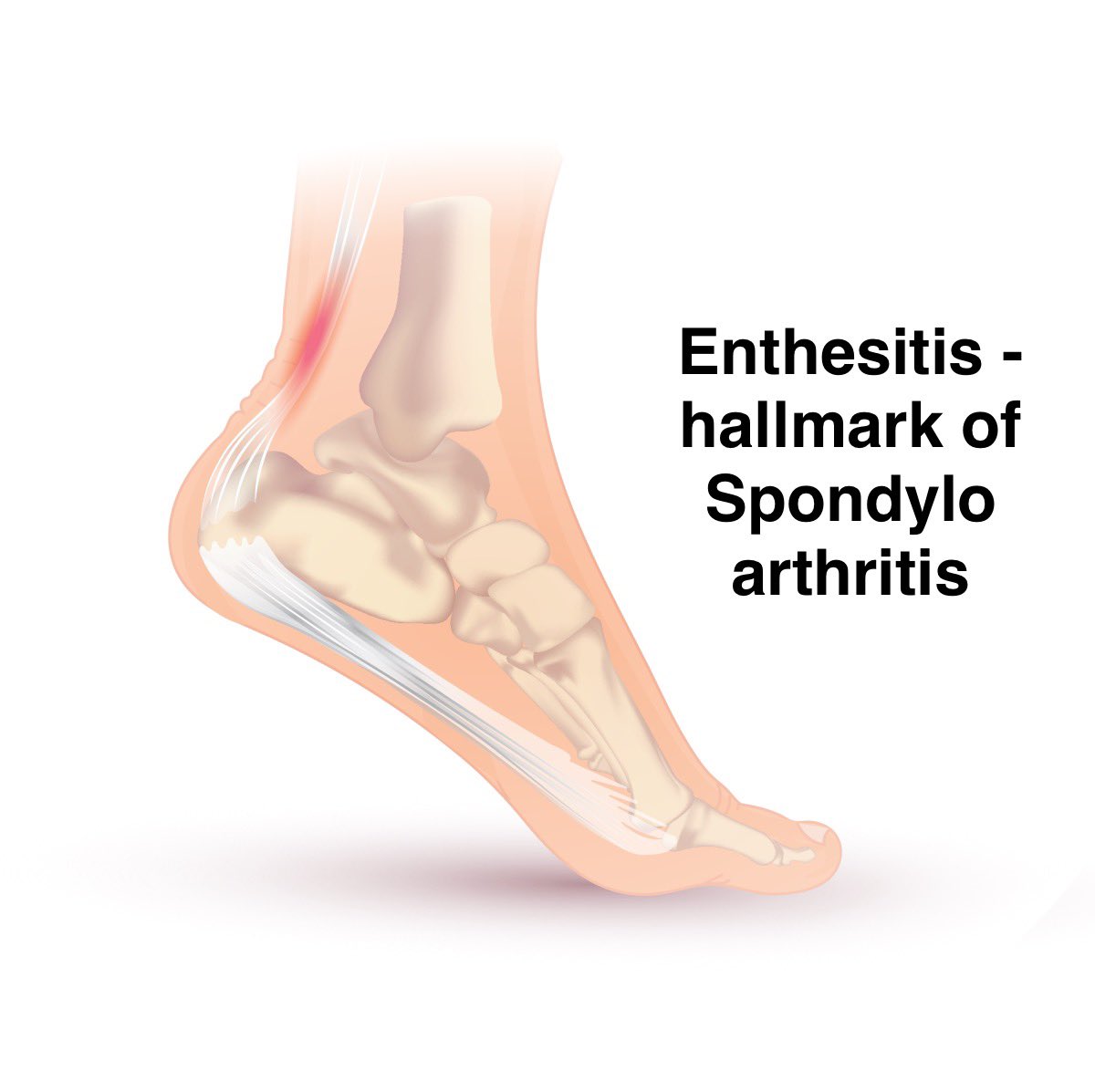
2️⃣ Enthesitis
= Inflammation at the enthesis (where tendons/ligaments insert into bone).
Common in: Spondyloarthritis (PsA, AS, IBD-arthritis).
Typical sites: Achilles tendon, plantar fascia, costochondral junctions.
Pain is deep, localized, worse with stress.
= Inflammation at the enthesis (where tendons/ligaments insert into bone).
Common in: Spondyloarthritis (PsA, AS, IBD-arthritis).
Typical sites: Achilles tendon, plantar fascia, costochondral junctions.
Pain is deep, localized, worse with stress.
3️⃣ Tenosynovitis
= Inflammation of the tendon sheath.
Classic example: de Quervain’s at wrist.
Also in RA, lupus, spondyloarthritis, infections (TB).
Feels like “painful sausage around the tendon.”
= Inflammation of the tendon sheath.
Classic example: de Quervain’s at wrist.
Also in RA, lupus, spondyloarthritis, infections (TB).
Feels like “painful sausage around the tendon.”

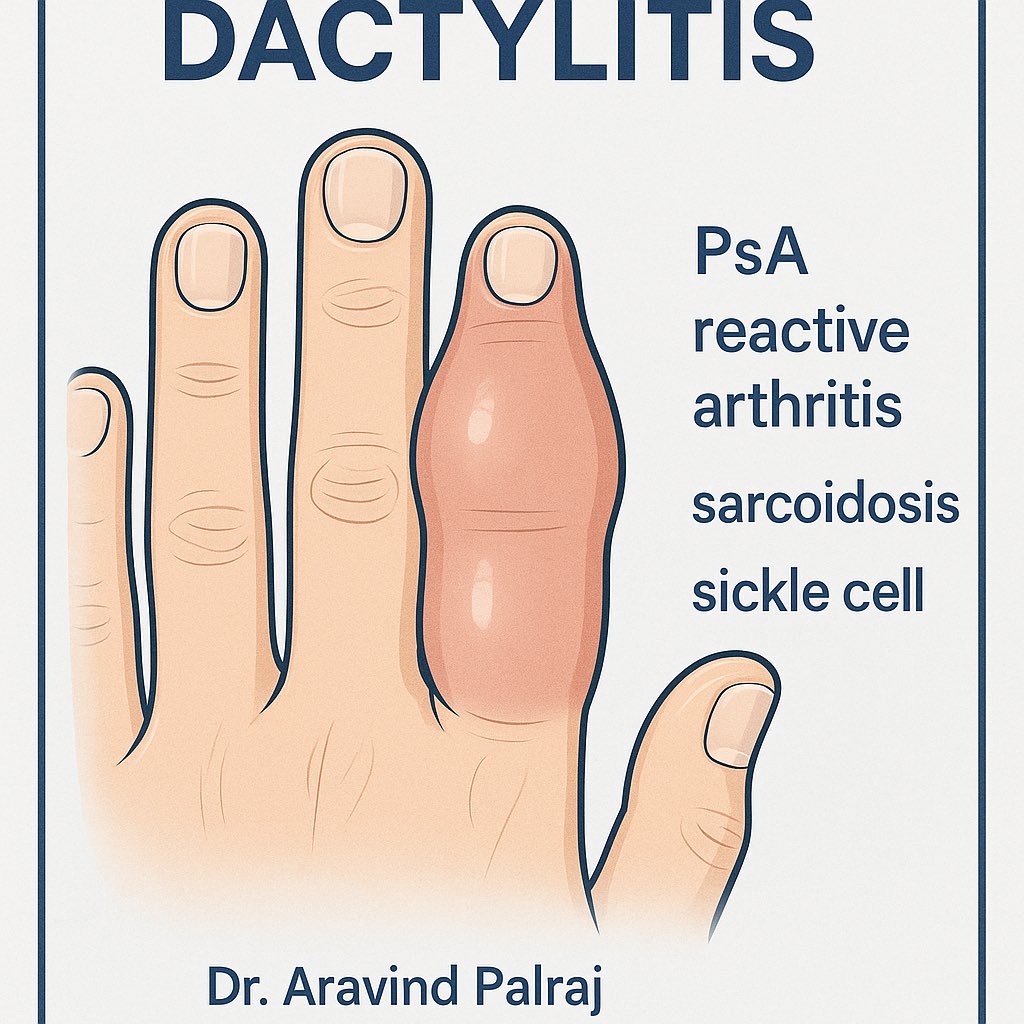
4️⃣ Dactylitis
= “Sausage digit” → uniform swelling of entire finger/toe.
Due to synovitis + tenosynovitis + enthesitis together.
Seen in: Psoriatic arthritis, reactive arthritis, sarcoidosis, sickle cell disease.
= “Sausage digit” → uniform swelling of entire finger/toe.
Due to synovitis + tenosynovitis + enthesitis together.
Seen in: Psoriatic arthritis, reactive arthritis, sarcoidosis, sickle cell disease.
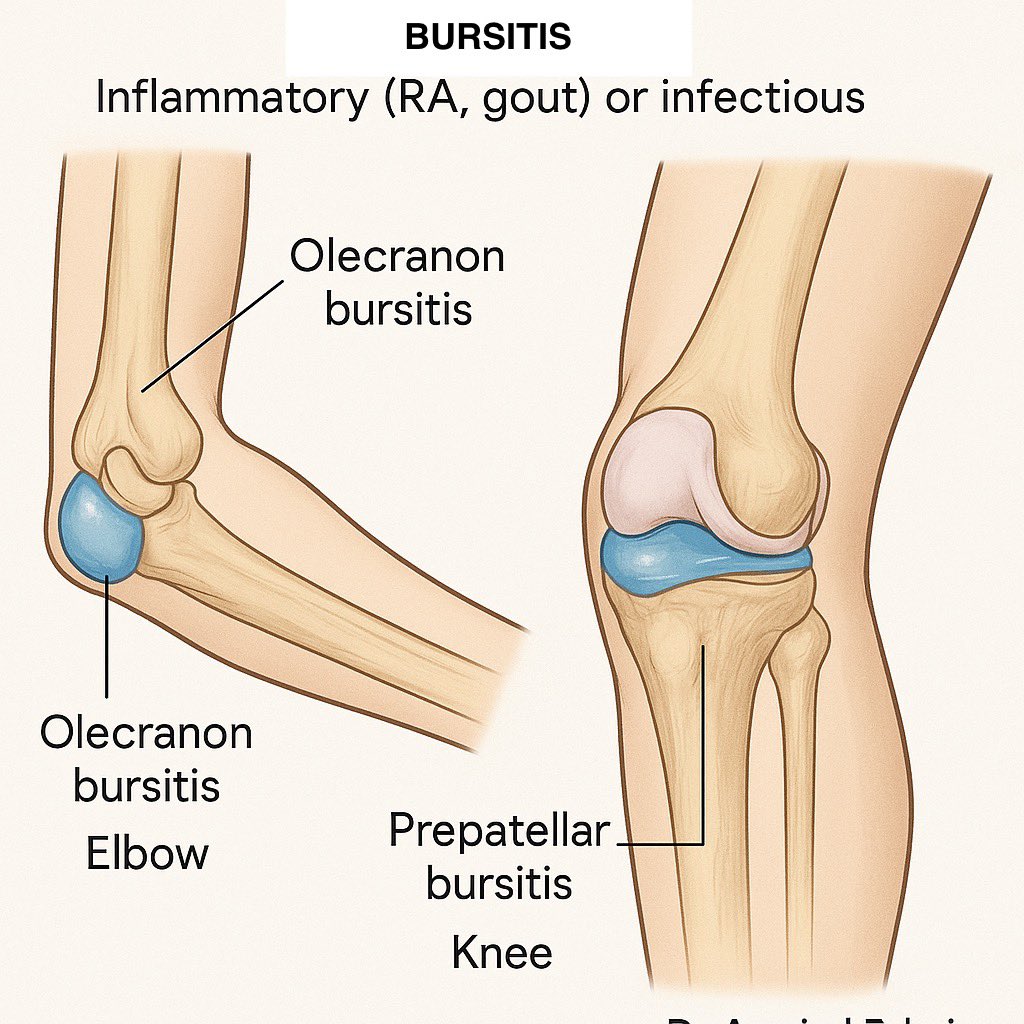
5️⃣ Bursitis
= Inflammation of a bursa (fluid-filled sac cushioning bone/tendon/joint).
Examples:
•Olecranon bursitis (“student’s elbow”)
•Prepatellar bursitis (“housemaid’s knee”)
Can be inflammatory (RA, gout) or infectious.
= Inflammation of a bursa (fluid-filled sac cushioning bone/tendon/joint).
Examples:
•Olecranon bursitis (“student’s elbow”)
•Prepatellar bursitis (“housemaid’s knee”)
Can be inflammatory (RA, gout) or infectious.
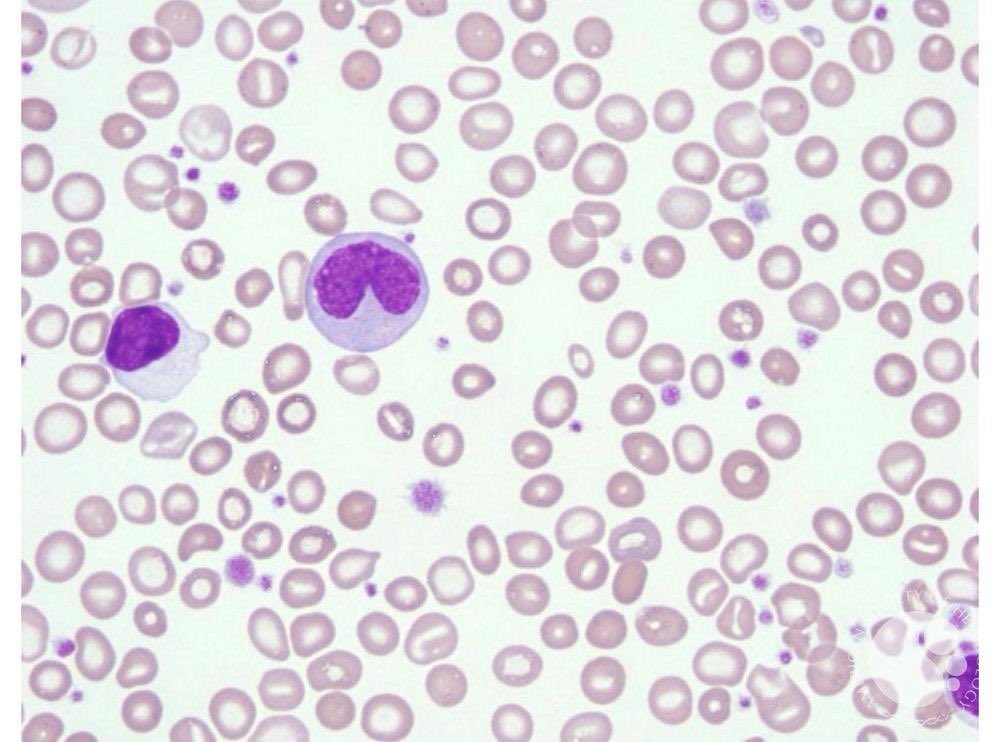
6️⃣ Myositis
= Inflammation of skeletal muscle fibers.
Manifestation: proximal muscle weakness ± pain.
Seen in: Dermatomyositis, Polymyositis, overlap syndromes.
Clue: ↑ CK, MRI edema, muscle biopsy changes.
= Inflammation of skeletal muscle fibers.
Manifestation: proximal muscle weakness ± pain.
Seen in: Dermatomyositis, Polymyositis, overlap syndromes.
Clue: ↑ CK, MRI edema, muscle biopsy changes.

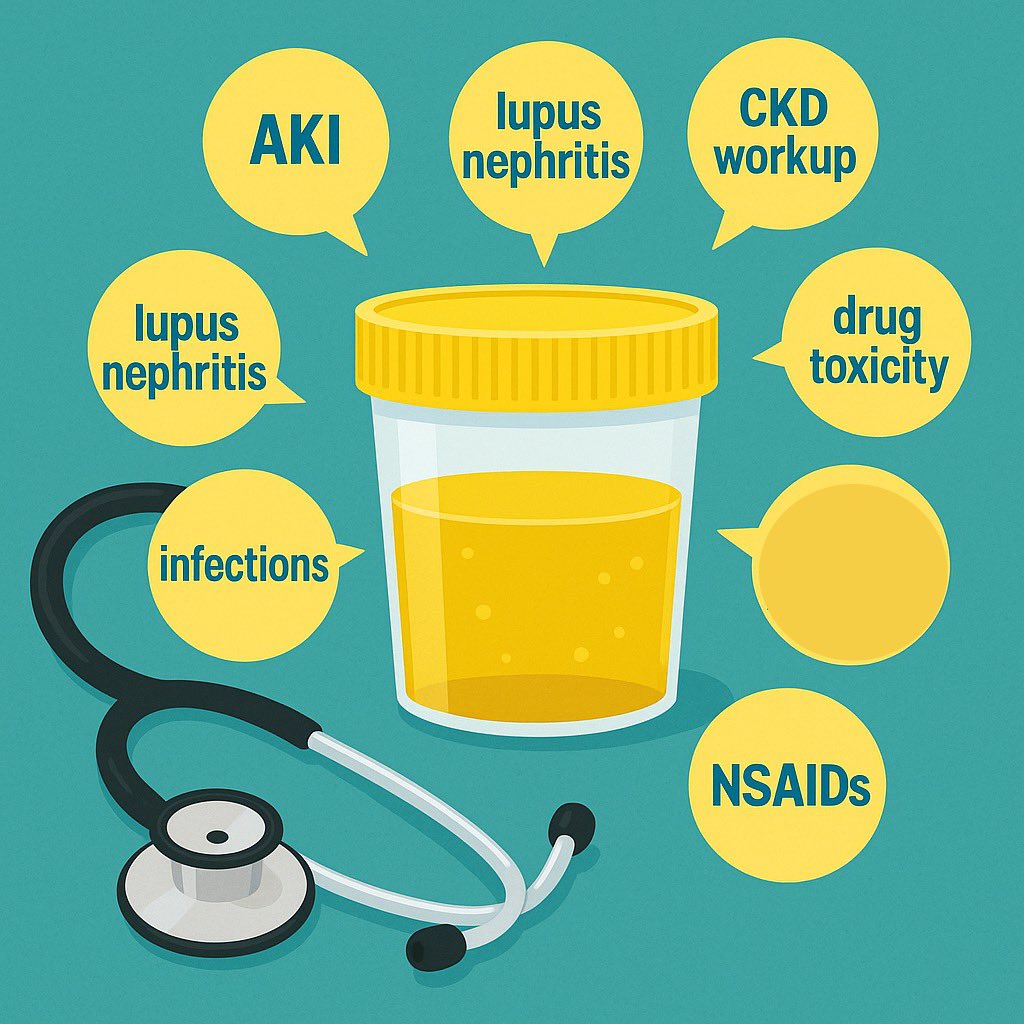
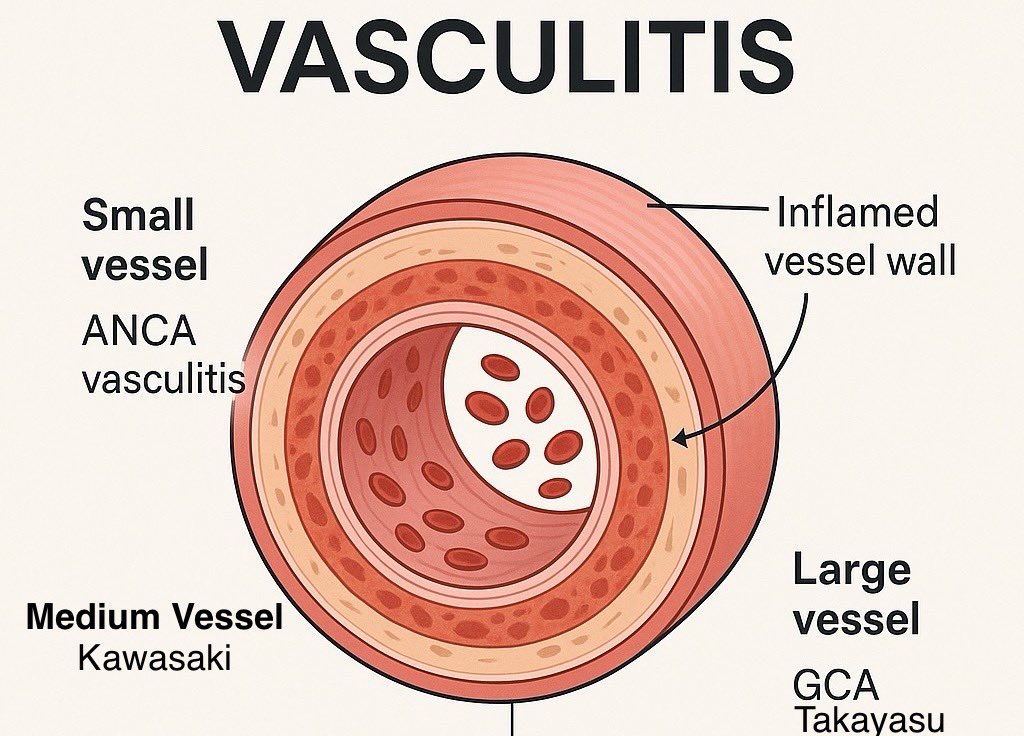
7️⃣ Vasculitis
= Inflammation of blood vessel wall → ischemia, organ damage.
Small, medium, large vessel types.
Seen in: ANCA vasculitis, PAN, GCA, Takayasu’s.
Clue: purpura, ulcers, hematuria, neuropathy.
= Inflammation of blood vessel wall → ischemia, organ damage.
Small, medium, large vessel types.
Seen in: ANCA vasculitis, PAN, GCA, Takayasu’s.
Clue: purpura, ulcers, hematuria, neuropathy.
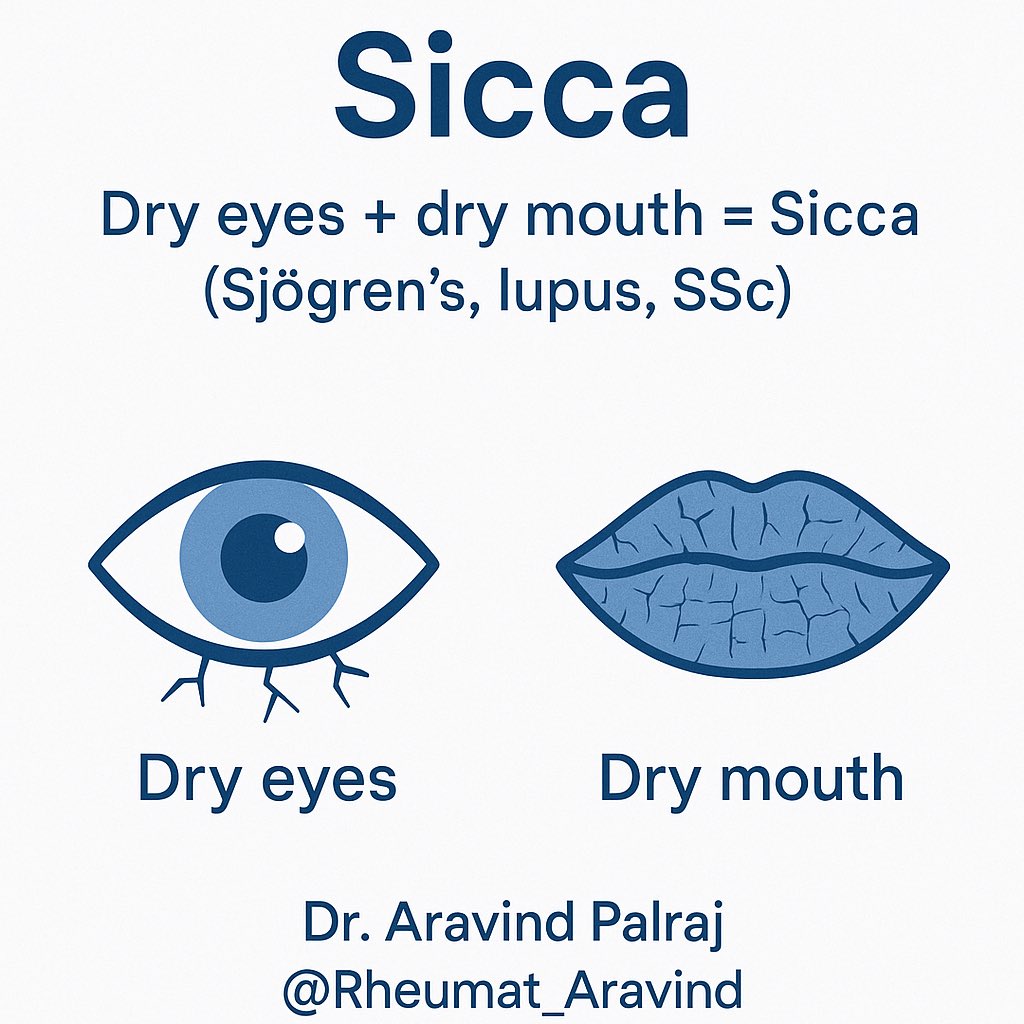
8️⃣ Sicca
= “Dryness” of eyes (keratoconjunctivitis sicca) & mouth (xerostomia).
Seen in: Sjögren’s, lupus, systemic sclerosis.
Clues: sandy eyes, difficulty swallowing dry food, rampant dental caries.
= “Dryness” of eyes (keratoconjunctivitis sicca) & mouth (xerostomia).
Seen in: Sjögren’s, lupus, systemic sclerosis.
Clues: sandy eyes, difficulty swallowing dry food, rampant dental caries.
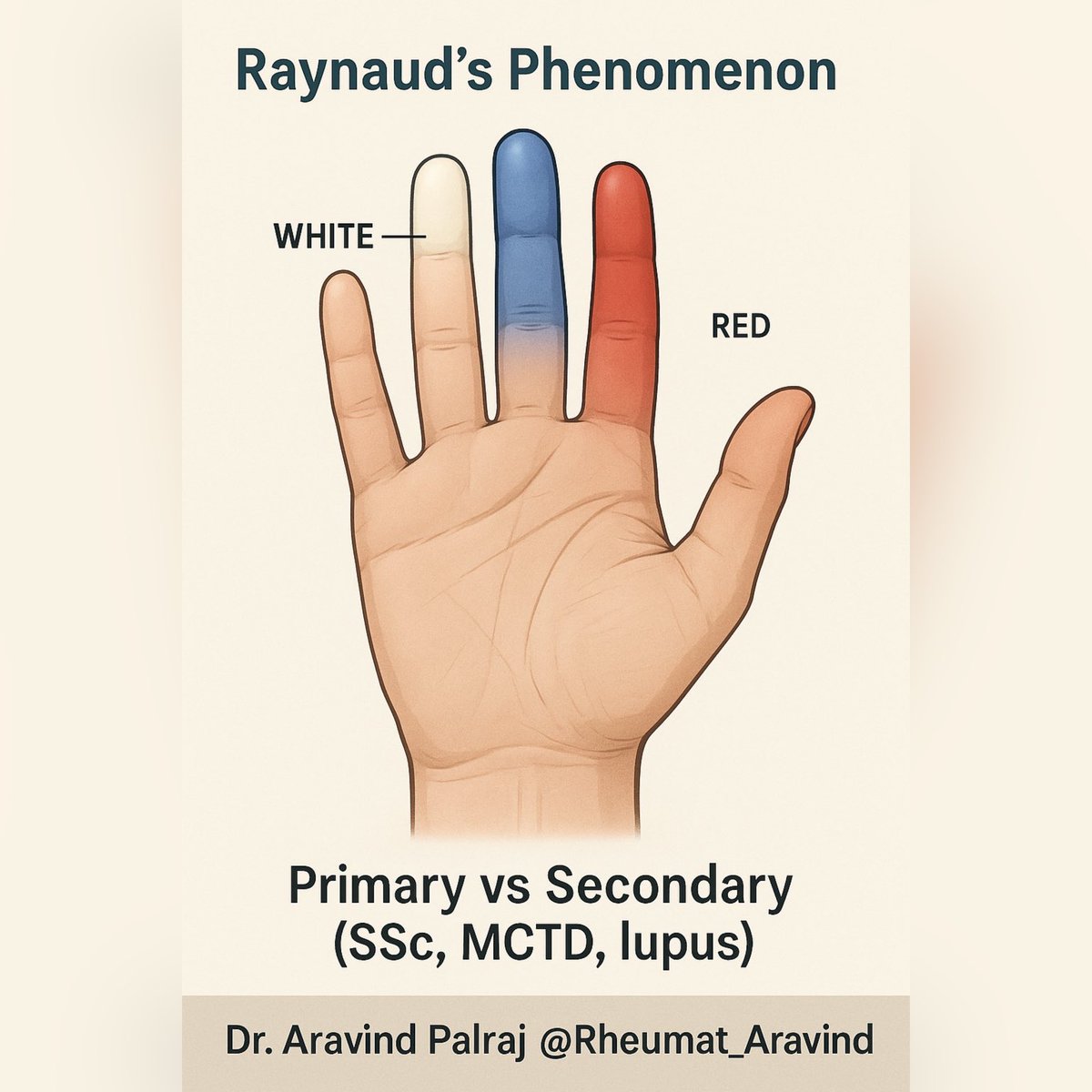
9️⃣ Raynaud’s Phenomenon
= Reversible color changes of fingers/toes on cold exposure or stress:
White → Blue → Red
Primary (benign) or Secondary (SSc, MCTD, lupus).
= Reversible color changes of fingers/toes on cold exposure or stress:
White → Blue → Red
Primary (benign) or Secondary (SSc, MCTD, lupus).
🔟 Takeaway
These terms aren’t just jargon.
They describe specific clinical patterns that point directly to diagnosis.
Mastering them = thinking like a rheumatologist 🔎
Share to spread knowledge.
These terms aren’t just jargon.
They describe specific clinical patterns that point directly to diagnosis.
Mastering them = thinking like a rheumatologist 🔎
Share to spread knowledge.
• • •
Missing some Tweet in this thread? You can try to
force a refresh