The Overlooked Causes of Parkinson’s Disease—and Prevention Strategies That Work
Avoiding pesticides and staying active can go a long way toward protecting your brain.
But one study found that a simple daily habit could reduce your risk by up to 80%.
🧵 THREAD
Avoiding pesticides and staying active can go a long way toward protecting your brain.
But one study found that a simple daily habit could reduce your risk by up to 80%.
🧵 THREAD

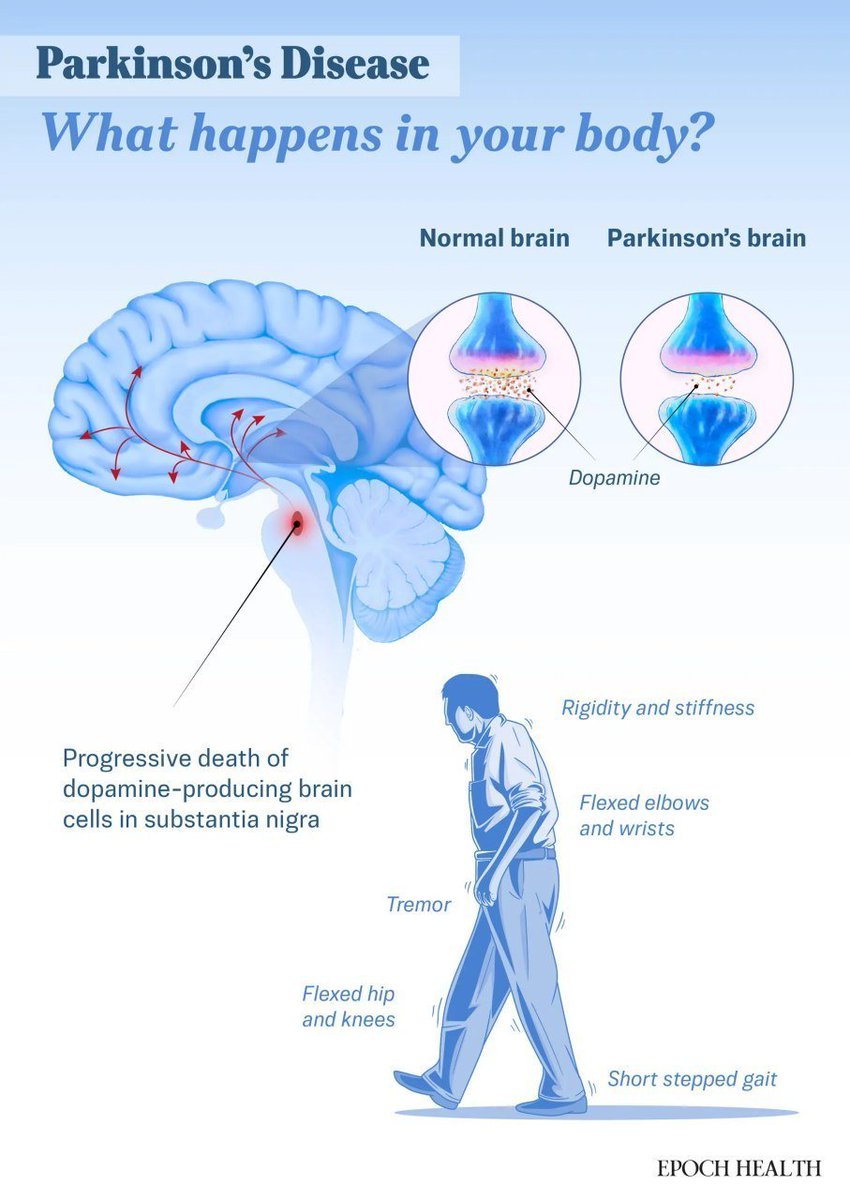
Parkinson’s disease is the second most common neurodegenerative disorder after Alzheimer’s disease.
In the United States alone, about 1.1 million people are currently living with this condition—a number expected to keep rising.
This progressive neurological disorder occurs when dopamine-producing neurons in the brain begin to degenerate, leading to movement- and emotion-related symptoms. It affects each person differently.
Though there isn’t a cure, certain lifestyle changes and natural approaches can help relieve symptoms effectively.
In the United States alone, about 1.1 million people are currently living with this condition—a number expected to keep rising.
This progressive neurological disorder occurs when dopamine-producing neurons in the brain begin to degenerate, leading to movement- and emotion-related symptoms. It affects each person differently.
Though there isn’t a cure, certain lifestyle changes and natural approaches can help relieve symptoms effectively.

What Are the Symptoms and Early Signs of Parkinson’s Disease?
Parkinson’s disease symptoms usually begin gradually and may be subtle at first. Symptoms often start on one side of the body and typically remain more severe on that side, even as they progress.
Common symptoms may include:
• Tremor: The most common movement-related symptom is tremor—particularly the classic “pill-rolling” motion between thumb and forefinger—that usually starts in one hand during rest.
• Slowed movement: Moving more slowly and with greater difficulty. People may shuffle with shorter steps or have trouble rising from a chair.
• Rigid muscles: Experiencing muscle stiffness anywhere in the body, which can limit motion and often cause pain.
• Impaired posture and balance: Developing a stooped posture and experiencing balance problems or frequent falls.
• Loss of automatic movements: Showing fewer involuntary actions, such as blinking, smiling, or swinging the arms while walking.
Parkinson’s disease symptoms usually begin gradually and may be subtle at first. Symptoms often start on one side of the body and typically remain more severe on that side, even as they progress.
Common symptoms may include:
• Tremor: The most common movement-related symptom is tremor—particularly the classic “pill-rolling” motion between thumb and forefinger—that usually starts in one hand during rest.
• Slowed movement: Moving more slowly and with greater difficulty. People may shuffle with shorter steps or have trouble rising from a chair.
• Rigid muscles: Experiencing muscle stiffness anywhere in the body, which can limit motion and often cause pain.
• Impaired posture and balance: Developing a stooped posture and experiencing balance problems or frequent falls.
• Loss of automatic movements: Showing fewer involuntary actions, such as blinking, smiling, or swinging the arms while walking.
Beyond movement changes, other early signs emerge gradually:
• Speech and swallowing changes: Speaking in a softer, more rapid, slurred, or monotone voice. Swallowing may become difficult, often starting with coughing during meals.
• Writing changes: Writing in smaller, more cramped handwriting that becomes increasingly difficult to produce.
• Reduced sense of smell: Losing or diminishing the ability to smell—an often-overlooked symptom may appear long before diagnosis and affect quality of life.
• Cognitive impairment: Having trouble focusing, carrying on conversations, or processing information quickly.
• Sleep problems: Experiencing insomnia or rapid eye movement sleep behavior disorder, which causes people to act out their dreams due to the absence of normal muscle paralysis during dreaming.
• Speech and swallowing changes: Speaking in a softer, more rapid, slurred, or monotone voice. Swallowing may become difficult, often starting with coughing during meals.
• Writing changes: Writing in smaller, more cramped handwriting that becomes increasingly difficult to produce.
• Reduced sense of smell: Losing or diminishing the ability to smell—an often-overlooked symptom may appear long before diagnosis and affect quality of life.
• Cognitive impairment: Having trouble focusing, carrying on conversations, or processing information quickly.
• Sleep problems: Experiencing insomnia or rapid eye movement sleep behavior disorder, which causes people to act out their dreams due to the absence of normal muscle paralysis during dreaming.

Parkinson’s disease has five stages:
• Stage 1: Mild Symptoms
Experiencing subtle symptoms that typically affect only one side of the body. Daily activities remain unaffected, though slight changes in posture, facial expression, or walking may be noticeable.
• Stage 2: Moderate Symptoms
Noticing symptoms appear on both sides of the body. Daily activities remain manageable but take more time due to increased muscle stiffness and slowed movement. Postural changes continue, but balance is not yet affected.
• Stage 3: Middle Stage
Developing balance impairments that increase the risk of falls. Movements slow down further, and basic tasks like dressing or eating become more challenging but are still possible without full assistance.
• Stage 4: Severe Symptoms
Losing the ability to live independently. People may be able to stand without help but typically require a walker or other assistance to walk. Daily tasks require significant help.
• Stage 5: Most Advanced Stage
Reaching the most debilitating stage. People are often bedridden or require a wheelchair. Severe stiffness, frequent falls, and cognitive decline—such as dementia and hallucinations—are common. Full-time care is necessary.
• Stage 1: Mild Symptoms
Experiencing subtle symptoms that typically affect only one side of the body. Daily activities remain unaffected, though slight changes in posture, facial expression, or walking may be noticeable.
• Stage 2: Moderate Symptoms
Noticing symptoms appear on both sides of the body. Daily activities remain manageable but take more time due to increased muscle stiffness and slowed movement. Postural changes continue, but balance is not yet affected.
• Stage 3: Middle Stage
Developing balance impairments that increase the risk of falls. Movements slow down further, and basic tasks like dressing or eating become more challenging but are still possible without full assistance.
• Stage 4: Severe Symptoms
Losing the ability to live independently. People may be able to stand without help but typically require a walker or other assistance to walk. Daily tasks require significant help.
• Stage 5: Most Advanced Stage
Reaching the most debilitating stage. People are often bedridden or require a wheelchair. Severe stiffness, frequent falls, and cognitive decline—such as dementia and hallucinations—are common. Full-time care is necessary.

A little about us: We’re a team of journalists and researchers on a mission to give you REAL and honest information about your health.
Side effects of reading our posts may include: critical thinking.
Follow us for more daily threads—backed by hard data.
—> @EpochHealth
Side effects of reading our posts may include: critical thinking.
Follow us for more daily threads—backed by hard data.
—> @EpochHealth

What Causes Parkinson’s Disease?
Parkinson’s disease is a brain disorder that gradually worsens over time.
theepochtimes.com/health/parkins…
Parkinson’s disease is a brain disorder that gradually worsens over time.
theepochtimes.com/health/parkins…
It occurs when brain cells—especially those that produce dopamine, a chemical that helps regulate movement—are lost or damaged.
When more than half of these dopamine-producing cells are gone, movement problems such as tremors, stiffness, slowness, and issues with balance and coordination begin to appear.
In Parkinson’s disease, the brain undergoes many changes.
The changes involves the presence of abnormal protein clumps called Lewy bodies. These clumps consist largely of alpha-synuclein, a protein that, in Parkinson’s, builds up in a way the brain cannot clear.
This buildup is a key focus of ongoing research, as it appears to drive disease progression. Some patients also have altered mitochondria, leading to brain cell damage.
When more than half of these dopamine-producing cells are gone, movement problems such as tremors, stiffness, slowness, and issues with balance and coordination begin to appear.
In Parkinson’s disease, the brain undergoes many changes.
The changes involves the presence of abnormal protein clumps called Lewy bodies. These clumps consist largely of alpha-synuclein, a protein that, in Parkinson’s, builds up in a way the brain cannot clear.
This buildup is a key focus of ongoing research, as it appears to drive disease progression. Some patients also have altered mitochondria, leading to brain cell damage.
For the vast majority of cases, the exact cause of Parkinson’s remains unknown. However, research points to a multifaceted interplay between genetic and environmental factors.
Chemical exposures represent a major environmental risk factor.
Long-term exposure to pesticides and herbicides significantly increases the risk—particularly for people working in agriculture or living in farming communities.
Veterans exposed to Agent Orange during the Vietnam War show notably higher rates of Parkinson’s disease. Industrial toxins, including certain workplace chemicals and heavy metals, may also contribute.
Some studies even suggest that contaminated well water in specific regions could raise the risk.
Risk factors for Parkinson’s disease:
• Age: The strongest known risk factor. Parkinson’s disease becomes more common with age, typically appearing in people in their 60s. However, about 5 percent to 10 percent of cases are diagnosed before age 50.
• Sex: Being male increases the risk. Parkinson’s disease is about 50 percent more common in men.
• Family history: Having a parent or sibling with Parkinson’s roughly doubles a person’s risk of developing the disease.
• Head injuries: A history of traumatic brain injury or repeated head trauma may increase the risk of Parkinson’s.
Chemical exposures represent a major environmental risk factor.
Long-term exposure to pesticides and herbicides significantly increases the risk—particularly for people working in agriculture or living in farming communities.
Veterans exposed to Agent Orange during the Vietnam War show notably higher rates of Parkinson’s disease. Industrial toxins, including certain workplace chemicals and heavy metals, may also contribute.
Some studies even suggest that contaminated well water in specific regions could raise the risk.
Risk factors for Parkinson’s disease:
• Age: The strongest known risk factor. Parkinson’s disease becomes more common with age, typically appearing in people in their 60s. However, about 5 percent to 10 percent of cases are diagnosed before age 50.
• Sex: Being male increases the risk. Parkinson’s disease is about 50 percent more common in men.
• Family history: Having a parent or sibling with Parkinson’s roughly doubles a person’s risk of developing the disease.
• Head injuries: A history of traumatic brain injury or repeated head trauma may increase the risk of Parkinson’s.

How Is Parkinson’s Disease Diagnosed?
Parkinson’s disease cannot be diagnosed with a single specific test. Instead, a neurologist evaluates the person’s medical history and symptoms and performs a neurological and physical examination to make a clinical diagnosis.
Diagnostic criteria, according to most clinical guidelines, include slowness of movement (bradykinesia) along with a resting tremor and/or rigidity.
Tests Commonly Used in Diagnosis
Diagnostic imaging tools can support—but not confirm—a Parkinson’s diagnosis. These may include:
• Single-photon emission computed tomography scan (SPECT): A nuclear imaging test that creates 3D images of organs and tissues using a radioactive tracer. Used to assess internal brain structures but is not specific to Parkinson’s.
• Dopamine transporter scan: A specialized type of SPECT imaging that visualizes the brain’s dopamine system.
• Magnetic resonance imaging scan (MRI): Produces detailed images of brain structure. Typically used to rule out other conditions rather than diagnose Parkinson’s directly.
• Transcranial sonography scan: An ultrasound technique used to help distinguish idiopathic Parkinson’s–the most common form, with no known cause—from other movement disorders.
• Positron emission tomography scan: Assesses brain function and activity, especially in areas related to movement.
Parkinson’s disease cannot be diagnosed with a single specific test. Instead, a neurologist evaluates the person’s medical history and symptoms and performs a neurological and physical examination to make a clinical diagnosis.
Diagnostic criteria, according to most clinical guidelines, include slowness of movement (bradykinesia) along with a resting tremor and/or rigidity.
Tests Commonly Used in Diagnosis
Diagnostic imaging tools can support—but not confirm—a Parkinson’s diagnosis. These may include:
• Single-photon emission computed tomography scan (SPECT): A nuclear imaging test that creates 3D images of organs and tissues using a radioactive tracer. Used to assess internal brain structures but is not specific to Parkinson’s.
• Dopamine transporter scan: A specialized type of SPECT imaging that visualizes the brain’s dopamine system.
• Magnetic resonance imaging scan (MRI): Produces detailed images of brain structure. Typically used to rule out other conditions rather than diagnose Parkinson’s directly.
• Transcranial sonography scan: An ultrasound technique used to help distinguish idiopathic Parkinson’s–the most common form, with no known cause—from other movement disorders.
• Positron emission tomography scan: Assesses brain function and activity, especially in areas related to movement.

Emerging Diagnostic Tools
New approaches are being developed to improve early and accurate diagnosis of Parkinson’s disease:
• Earwax analysis: An artificial intelligence-powered method that examines scent compounds in earwax and has demonstrated up to 94 percent accuracy in detecting the condition.
• Polymerase chain reaction-based blood test: A test that analyzes genetic material to identify early signs of Parkinson’s more quickly and noninvasively.
• Artificial-intelligence enhanced “magnetic pen”: A machine learning-driven device that detects subtle writing-related motor deficits, offering another noninvasive diagnostic option.
New approaches are being developed to improve early and accurate diagnosis of Parkinson’s disease:
• Earwax analysis: An artificial intelligence-powered method that examines scent compounds in earwax and has demonstrated up to 94 percent accuracy in detecting the condition.
• Polymerase chain reaction-based blood test: A test that analyzes genetic material to identify early signs of Parkinson’s more quickly and noninvasively.
• Artificial-intelligence enhanced “magnetic pen”: A machine learning-driven device that detects subtle writing-related motor deficits, offering another noninvasive diagnostic option.

What Are the Treatments for Parkinson’s Disease?
While there’s no cure for Parkinson’s, a comprehensive treatment approach can significantly improve quality of life and slow the progression of symptoms.
1. Medication
Many medications for Parkinson’s disease either increase dopamine levels in the brain or mimic its effects.
• Carbidopa-levodopa: The most effective treatment for Parkinson’s symptoms. Levodopa is converted into dopamine in the brain, while carbidopa prevents levodopa from being converted too early outside the brain—ensuring more dopamine reaches its target. An inhaled version provides quick relief for managing intermittent “off” periods.
• Carbidopa-levodopa infusion: A gel form of the medication delivered directly to the small intestine through a feeding tube. This continuous delivery offers steady symptom control throughout the day and is used in advanced Parkinson’s disease.
• Vyalev (foscarbidopa and foslevodopa): Approved by the U.S. Food and Drug Administration in October 2024, Vyalev is the first 24-hour continuous subcutaneous levodopa infusion. It delivers steady dopamine levels to help reduce motor fluctuations.
• Dopamine agonists: These drugs act like dopamine in the brain and help improve movement symptoms. Other medications in this category include MAO-B inhibitors, COMT inhibitors, and A2A antagonists, which either keep dopamine from breaking down too quickly or help it work more effectively.
• Pimavanserin: A medication used specifically to treat hallucinations and delusions associated with Parkinson’s disease. It works on serotonin receptors and does not interfere with dopamine levels.
While there’s no cure for Parkinson’s, a comprehensive treatment approach can significantly improve quality of life and slow the progression of symptoms.
1. Medication
Many medications for Parkinson’s disease either increase dopamine levels in the brain or mimic its effects.
• Carbidopa-levodopa: The most effective treatment for Parkinson’s symptoms. Levodopa is converted into dopamine in the brain, while carbidopa prevents levodopa from being converted too early outside the brain—ensuring more dopamine reaches its target. An inhaled version provides quick relief for managing intermittent “off” periods.
• Carbidopa-levodopa infusion: A gel form of the medication delivered directly to the small intestine through a feeding tube. This continuous delivery offers steady symptom control throughout the day and is used in advanced Parkinson’s disease.
• Vyalev (foscarbidopa and foslevodopa): Approved by the U.S. Food and Drug Administration in October 2024, Vyalev is the first 24-hour continuous subcutaneous levodopa infusion. It delivers steady dopamine levels to help reduce motor fluctuations.
• Dopamine agonists: These drugs act like dopamine in the brain and help improve movement symptoms. Other medications in this category include MAO-B inhibitors, COMT inhibitors, and A2A antagonists, which either keep dopamine from breaking down too quickly or help it work more effectively.
• Pimavanserin: A medication used specifically to treat hallucinations and delusions associated with Parkinson’s disease. It works on serotonin receptors and does not interfere with dopamine levels.

2. Deep Brain Stimulation (DBS)
DBS is typically recommended for people with advanced Parkinson’s disease who experience unpredictable responses to levodopa. The procedure involves implanting electrodes in the brain to help reduce tremors, stabilize medication effects, decrease involuntary movements, relieve muscle rigidity, and improve overall motor function.
3. MRI-Guided Focused Ultrasound (MRgFUS)
MRgFUS is a minimally invasive procedure used to manage tremors in some people with Parkinson’s disease.
4. Physical Therapy
Physical therapy plays a crucial role in managing motor and functional challenges associated with Parkinson’s disease. Physical therapists use targeted strategies to help reduce stiffness, tremors, balance issues, and walking difficulties.
DBS is typically recommended for people with advanced Parkinson’s disease who experience unpredictable responses to levodopa. The procedure involves implanting electrodes in the brain to help reduce tremors, stabilize medication effects, decrease involuntary movements, relieve muscle rigidity, and improve overall motor function.
3. MRI-Guided Focused Ultrasound (MRgFUS)
MRgFUS is a minimally invasive procedure used to manage tremors in some people with Parkinson’s disease.
4. Physical Therapy
Physical therapy plays a crucial role in managing motor and functional challenges associated with Parkinson’s disease. Physical therapists use targeted strategies to help reduce stiffness, tremors, balance issues, and walking difficulties.

5. Supplements
Some research suggests that adding specific supplements may help ease symptoms when added to a balanced diet:
• Coenzyme Q10: Supports cellular energy production and may slow early disease progression.
• Vitamins C and E: Known for antioxidant properties; high doses may reduce Parkinson’s risk.
• Cytidinediphosphocholine: A naturally occurring compound that may help increase dopamine levels and reduce reliance on levodopa.
• Nicotinamide adenine dinucleotide: A compound that serves as an active form of vitamin B3. It may help boost dopamine production, though study results have been mixed.
Some research suggests that adding specific supplements may help ease symptoms when added to a balanced diet:
• Coenzyme Q10: Supports cellular energy production and may slow early disease progression.
• Vitamins C and E: Known for antioxidant properties; high doses may reduce Parkinson’s risk.
• Cytidinediphosphocholine: A naturally occurring compound that may help increase dopamine levels and reduce reliance on levodopa.
• Nicotinamide adenine dinucleotide: A compound that serves as an active form of vitamin B3. It may help boost dopamine production, though study results have been mixed.

6. Traditional Chinese Medicine (TCM)
TCM views illness as the result of internal imbalances. Parkinson’s disease has historically been treated within this framework using therapies such as acupuncture.
Some people with Parkinson’s symptoms may find acupuncture helpful, especially as a complement to conventional treatment.
TCM views illness as the result of internal imbalances. Parkinson’s disease has historically been treated within this framework using therapies such as acupuncture.
Some people with Parkinson’s symptoms may find acupuncture helpful, especially as a complement to conventional treatment.

What Are the Lifestyle Approaches for Parkinson’s Disease?
Lifestyle changes are often recommended to help manage symptoms related to movement and communication—and may even enhance the effectiveness of treatment.
1. Mediterranean and Antioxidant-Rich Diet
Research consistently shows that the Mediterranean diet may delay Parkinson’s onset and slow disease progression. This eating pattern emphasizes olive oil as the primary fat source and includes fatty fish, fruits, vegetables, and whole grains. Regularly eating fatty fish rich in omega-3s provides brain-protective nutrients.
A meta-analysis published in February found that the Mediterranean diet may also reduce the risk of Parkinson’s disease by lowering inflammation, supporting healthy gut bacteria, and improving mitochondrial function.
Eating antioxidant-rich foods—such as berries, leafy greens, and colorful vegetables—may help combat oxidative stress, which contributes to the breakdown of dopamine-producing brain cells. Getting enough fiber can help manage constipation, a common issue in Parkinson’s.
Timing protein intake away from levodopa doses may improve medication absorption, while staying hydrated supports overall health and enhances the effectiveness of treatment.
Lifestyle changes are often recommended to help manage symptoms related to movement and communication—and may even enhance the effectiveness of treatment.
1. Mediterranean and Antioxidant-Rich Diet
Research consistently shows that the Mediterranean diet may delay Parkinson’s onset and slow disease progression. This eating pattern emphasizes olive oil as the primary fat source and includes fatty fish, fruits, vegetables, and whole grains. Regularly eating fatty fish rich in omega-3s provides brain-protective nutrients.
A meta-analysis published in February found that the Mediterranean diet may also reduce the risk of Parkinson’s disease by lowering inflammation, supporting healthy gut bacteria, and improving mitochondrial function.
Eating antioxidant-rich foods—such as berries, leafy greens, and colorful vegetables—may help combat oxidative stress, which contributes to the breakdown of dopamine-producing brain cells. Getting enough fiber can help manage constipation, a common issue in Parkinson’s.
Timing protein intake away from levodopa doses may improve medication absorption, while staying hydrated supports overall health and enhances the effectiveness of treatment.

2. Dopamine-Driven Exercise
Exercise plays a vital role in managing symptoms. It enhances mobility, balance, flexibility, and strength.
Physical activity increases dopamine levels in the brain. It is also believed to lower oxidative stress, inflammation, and the buildup of toxic alpha-synuclein clumps in the brain—which contribute to nerve cell death in Parkinson’s disease.
A 2024 study found that six months of intense exercise boosted dopamine in people with early Parkinson’s.
A 2021 meta-analysis found that bicycling significantly improved motor function—especially gait—as well as balance, walking speed, and overall quality of life. While cognitive benefits were less pronounced, cycling programs consistently produced positive physical outcomes.
Overall, bicycling appears to be a safe and effective intervention for improving movement and well-being in people with Parkinson’s disease.
Daily exercise—including activities like swimming and brisk walking—helps maintain muscle strength, flexibility, and mental well-being. Both moderate activities such as water aerobics and vigorous ones like jogging or hiking are beneficial.
Exercise plays a vital role in managing symptoms. It enhances mobility, balance, flexibility, and strength.
Physical activity increases dopamine levels in the brain. It is also believed to lower oxidative stress, inflammation, and the buildup of toxic alpha-synuclein clumps in the brain—which contribute to nerve cell death in Parkinson’s disease.
A 2024 study found that six months of intense exercise boosted dopamine in people with early Parkinson’s.
A 2021 meta-analysis found that bicycling significantly improved motor function—especially gait—as well as balance, walking speed, and overall quality of life. While cognitive benefits were less pronounced, cycling programs consistently produced positive physical outcomes.
Overall, bicycling appears to be a safe and effective intervention for improving movement and well-being in people with Parkinson’s disease.
Daily exercise—including activities like swimming and brisk walking—helps maintain muscle strength, flexibility, and mental well-being. Both moderate activities such as water aerobics and vigorous ones like jogging or hiking are beneficial.

3. Dance and Music
Dance classes designed for people with Parkinson’s help improve motor control and boost mood through music and social interaction.
A 2022 study found that while music initially improved participants’ gait, their walking improved even without music after class—suggesting they may have internalized the rhythm through dance.
Synchronized drumming activates the caudate nucleus—a brain region affected in Parkinson’s disease—and has been shown to improve mood, attention, and social connection.
In one study, people with Parkinson’s who participated in twice-weekly West African drum circle sessions for six weeks reported a significant improvement in quality of life.
The findings suggest that drumming may be a valuable complement to traditional therapies like physical therapy.
Dance classes designed for people with Parkinson’s help improve motor control and boost mood through music and social interaction.
A 2022 study found that while music initially improved participants’ gait, their walking improved even without music after class—suggesting they may have internalized the rhythm through dance.
Synchronized drumming activates the caudate nucleus—a brain region affected in Parkinson’s disease—and has been shown to improve mood, attention, and social connection.
In one study, people with Parkinson’s who participated in twice-weekly West African drum circle sessions for six weeks reported a significant improvement in quality of life.
The findings suggest that drumming may be a valuable complement to traditional therapies like physical therapy.

4. Massage
Massage therapy may improve circulation and reduce muscle spasms. Craniosacral therapy—a specialized massage technique that targets the brain and spinal column—may help lessen tremors and improve overall function.
5. Mind-Body Practices
Practices such as tai chi, yoga, and qigong can enhance balance, flexibility, and range of motion for people with Parkinson’s disease, while promoting better mood and sleep.
Massage therapy may improve circulation and reduce muscle spasms. Craniosacral therapy—a specialized massage technique that targets the brain and spinal column—may help lessen tremors and improve overall function.
5. Mind-Body Practices
Practices such as tai chi, yoga, and qigong can enhance balance, flexibility, and range of motion for people with Parkinson’s disease, while promoting better mood and sleep.

How Does Mindset Affect Parkinson’s Disease?
People living with Parkinson’s disease often face physical, emotional, and mental challenges that affect daily life.
A 2022 survey of more than 1,400 people with Parkinson’s found that 75 percent said maintaining a positive attitude significantly improved their quality of life. In addition, 70 percent reported needing some form of support, with emotional support identified as the most important.
Many respondents noted that humor and laughter were helpful—51 percent used them as coping tools, while nearly half drew strength from faith or spirituality.
Staying engaged in meaningful activities—such as volunteering, crafting, reading, journaling, meditating, shopping, painting, and spending time with loved ones—also played a key role in helping them stay positive and emotionally resilient.
People living with Parkinson’s disease often face physical, emotional, and mental challenges that affect daily life.
A 2022 survey of more than 1,400 people with Parkinson’s found that 75 percent said maintaining a positive attitude significantly improved their quality of life. In addition, 70 percent reported needing some form of support, with emotional support identified as the most important.
Many respondents noted that humor and laughter were helpful—51 percent used them as coping tools, while nearly half drew strength from faith or spirituality.
Staying engaged in meaningful activities—such as volunteering, crafting, reading, journaling, meditating, shopping, painting, and spending time with loved ones—also played a key role in helping them stay positive and emotionally resilient.

How Can I Prevent Parkinson’s Disease?
There is no known way to prevent Parkinson’s disease, but certain lifestyle choices may help lower your risk.
• Diet: Eating enough protein can help prevent weight loss and muscle wasting while supporting healing and disease resistance. Maintaining a balanced diet is also important.
• Caffeine: Caffeine has neuroprotective effects and may reduce brain inflammation and oxidative stress—both linked to dopamine nerve loss. Multiple studies have associated caffeine consumption with a reduced risk of Parkinson’s. One study found that drinking at least 28 ounces of coffee daily in midlife lowered the risk of developing Parkinson’s disease by five times at age 65 compared to those who did not drink coffee.
• Gait training: Practicing gait exercises can improve balance, reduce the risk of falls, and correct abnormal walking patterns associated with Parkinson’s.
• Avoiding harmful chemicals: Reducing exposure to pesticides, herbicides, and industrial toxins may help lower the risk of Parkinson’s disease.
There is no known way to prevent Parkinson’s disease, but certain lifestyle choices may help lower your risk.
• Diet: Eating enough protein can help prevent weight loss and muscle wasting while supporting healing and disease resistance. Maintaining a balanced diet is also important.
• Caffeine: Caffeine has neuroprotective effects and may reduce brain inflammation and oxidative stress—both linked to dopamine nerve loss. Multiple studies have associated caffeine consumption with a reduced risk of Parkinson’s. One study found that drinking at least 28 ounces of coffee daily in midlife lowered the risk of developing Parkinson’s disease by five times at age 65 compared to those who did not drink coffee.
• Gait training: Practicing gait exercises can improve balance, reduce the risk of falls, and correct abnormal walking patterns associated with Parkinson’s.
• Avoiding harmful chemicals: Reducing exposure to pesticides, herbicides, and industrial toxins may help lower the risk of Parkinson’s disease.

What Are the Complications of Parkinson’s Disease?
Parkinson’s disease can lead to various complications, many of which worsen as the condition progresses.
• Difficulty thinking: Many people with Parkinson’s develop impairment, dementia, or other thinking challenges, typically in the later stages. These complications may be managed with medications and behavioral interventions.
• Sleep problems: Difficulty falling asleep, frequent night awakenings, early waking, daytime sleepiness, and sleep apnea are common. Sleep apnea affects about 40 percent of people with Parkinson’s.
• Eating problems: Late-stage Parkinson’s can impair the muscles used for chewing, increasing the risk of choking. As the disease progresses, swallowing difficulties may lead to poor nutrition and saliva buildup, which can cause drooling.
• Bladder issues: About 30 percent to 60 percent of people with Parkinson’s experience urinary problems, such as difficulty urinating or loss of bladder control.
Parkinson’s disease can lead to various complications, many of which worsen as the condition progresses.
• Difficulty thinking: Many people with Parkinson’s develop impairment, dementia, or other thinking challenges, typically in the later stages. These complications may be managed with medications and behavioral interventions.
• Sleep problems: Difficulty falling asleep, frequent night awakenings, early waking, daytime sleepiness, and sleep apnea are common. Sleep apnea affects about 40 percent of people with Parkinson’s.
• Eating problems: Late-stage Parkinson’s can impair the muscles used for chewing, increasing the risk of choking. As the disease progresses, swallowing difficulties may lead to poor nutrition and saliva buildup, which can cause drooling.
• Bladder issues: About 30 percent to 60 percent of people with Parkinson’s experience urinary problems, such as difficulty urinating or loss of bladder control.

Thanks for reading! If you found this valuable, here's a special deal:
Unlock our ENTIRE library of @EpochHealth articles for just $1/week—plus unlimited access to everything else on our site.
Claim it here:
on.theepochtimes.com/vfox/health?ut…
Unlock our ENTIRE library of @EpochHealth articles for just $1/week—plus unlimited access to everything else on our site.
Claim it here:
on.theepochtimes.com/vfox/health?ut…

• • •
Missing some Tweet in this thread? You can try to
force a refresh