🧵 Fever of Unknown Origin (FUO) – A Clinical Approach
Every doctor faces this: a patient with fever that just won’t go away.
Here’s how to tackle FUO in a systematic, bedside-friendly way 👇
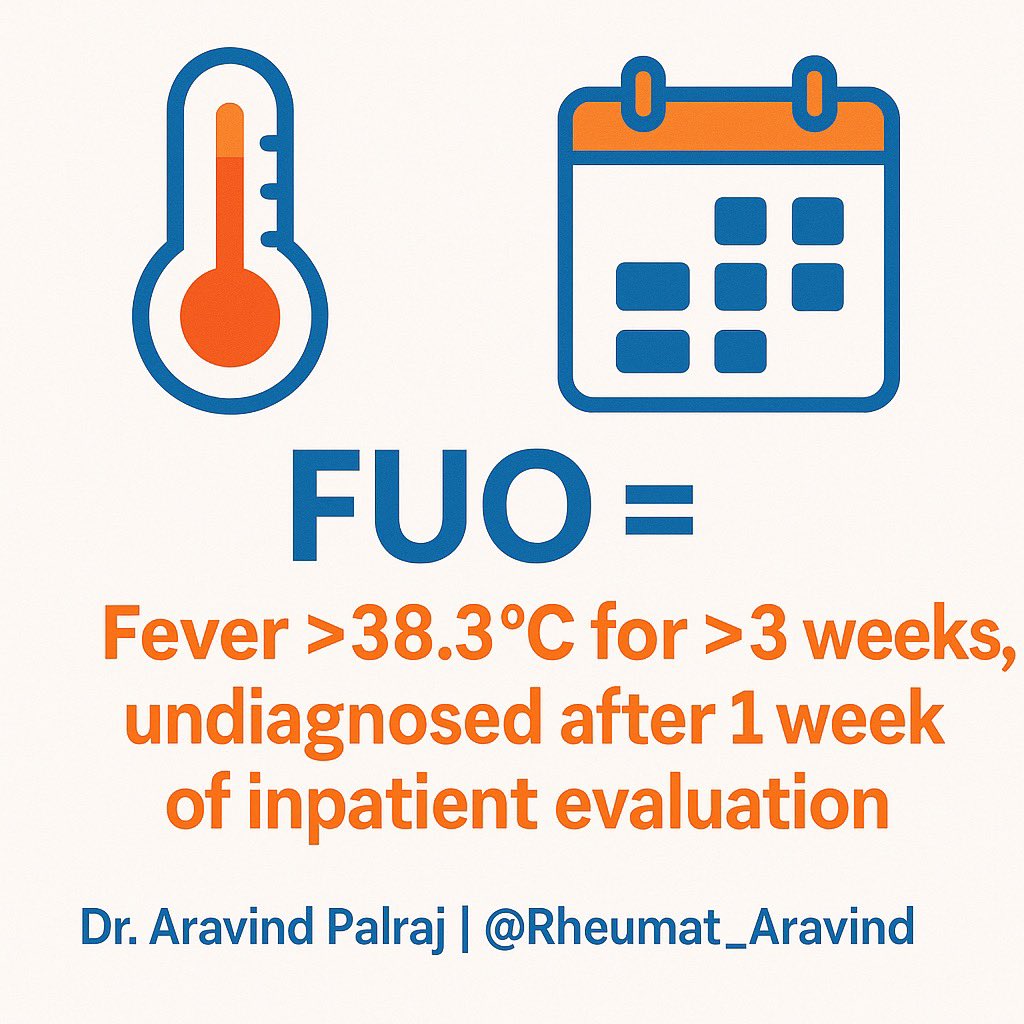
1. Definition 🔑
FUO = Fever >38.3°C (101°F) on multiple occasions, lasting >3 weeks, with no diagnosis despite 1 week of inpatient evaluation.
👉 Not just “fever for long time” — it’s a diagnosis of exclusion.
@IhabFathiSulima @DrAkhilX #MedTwitter #RheumTwitter
Every doctor faces this: a patient with fever that just won’t go away.
Here’s how to tackle FUO in a systematic, bedside-friendly way 👇
1. Definition 🔑
FUO = Fever >38.3°C (101°F) on multiple occasions, lasting >3 weeks, with no diagnosis despite 1 week of inpatient evaluation.
👉 Not just “fever for long time” — it’s a diagnosis of exclusion.
@IhabFathiSulima @DrAkhilX #MedTwitter #RheumTwitter
2. Categories of FUO 📂
Classically 4 buckets:
•Infectious
•Malignancy
•Autoimmune / Rheumatologic
•Miscellaneous / Undiagnosed
Classically 4 buckets:
•Infectious
•Malignancy
•Autoimmune / Rheumatologic
•Miscellaneous / Undiagnosed

3. Start with the basics 🩺
•Re-take history: travel, exposures, drugs, family hx.
•Do a head-to-toe exam: lymph nodes, rash, murmurs, organomegaly, joint swelling.
👉 Many diagnoses are hidden in plain sight.
•Re-take history: travel, exposures, drugs, family hx.
•Do a head-to-toe exam: lymph nodes, rash, murmurs, organomegaly, joint swelling.
👉 Many diagnoses are hidden in plain sight.
4. First-line labs 🧪
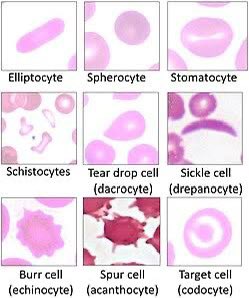
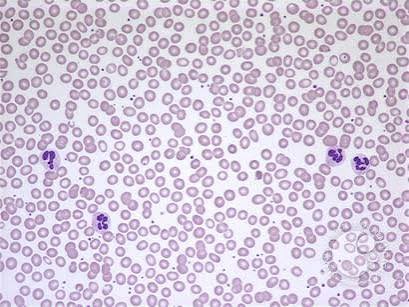
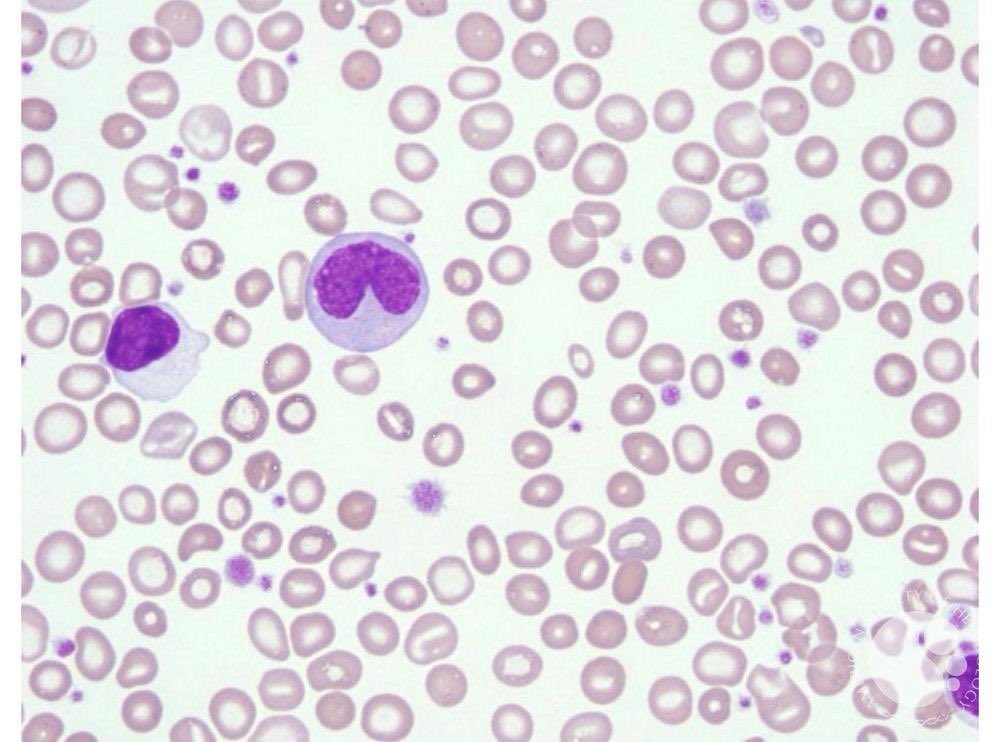
•CBC + Differential
•ESR, CRP (trend them!)
•LFT, RFT
•Blood cultures (multiple sets)
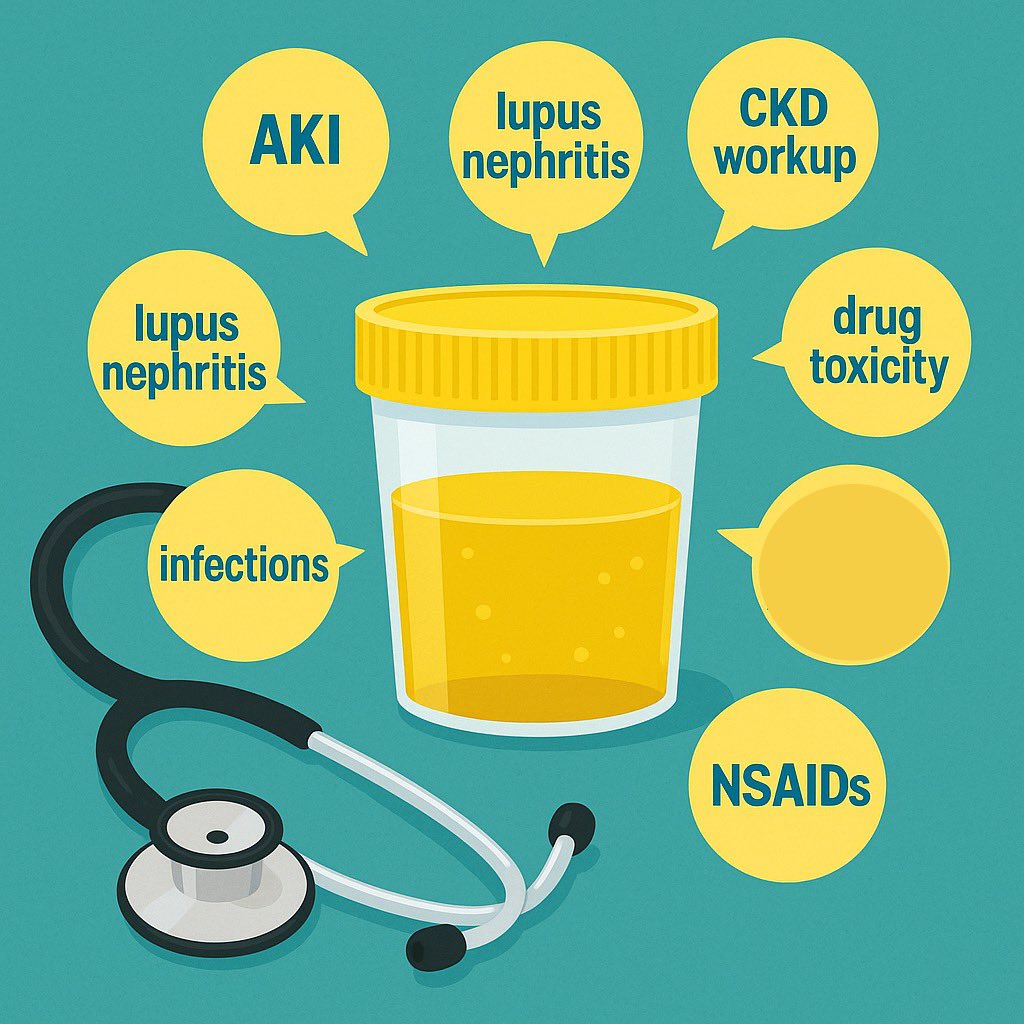
•Urinalysis + cultures
•CBC + Differential
•ESR, CRP (trend them!)
•LFT, RFT
•Blood cultures (multiple sets)
•Urinalysis + cultures

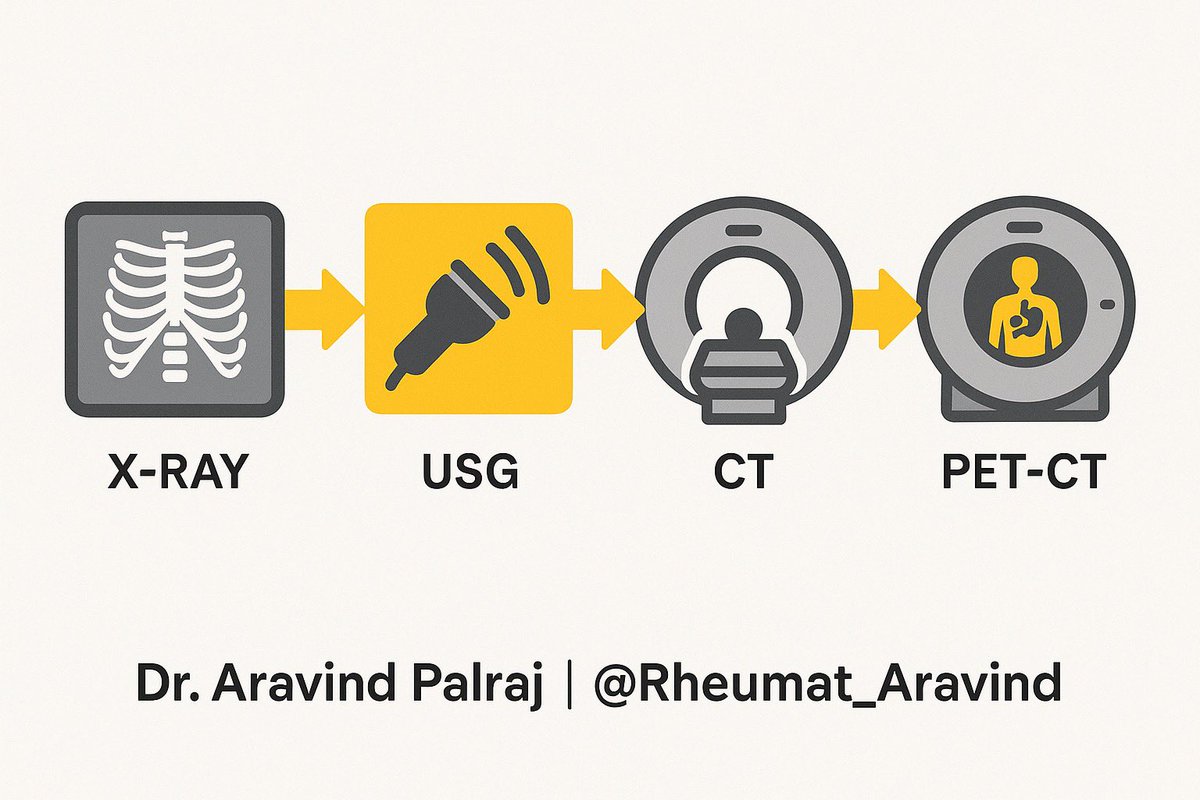
5. Imaging 🔍
•Chest X-ray (never skip)
•Ultrasound abdomen
•If still blind → CT Chest/Abdomen/Pelvis
•FDG-PET is emerging as a powerful tool for hidden malignancy, vasculitis, sarcoid.
•Chest X-ray (never skip)
•Ultrasound abdomen
•If still blind → CT Chest/Abdomen/Pelvis
•FDG-PET is emerging as a powerful tool for hidden malignancy, vasculitis, sarcoid.
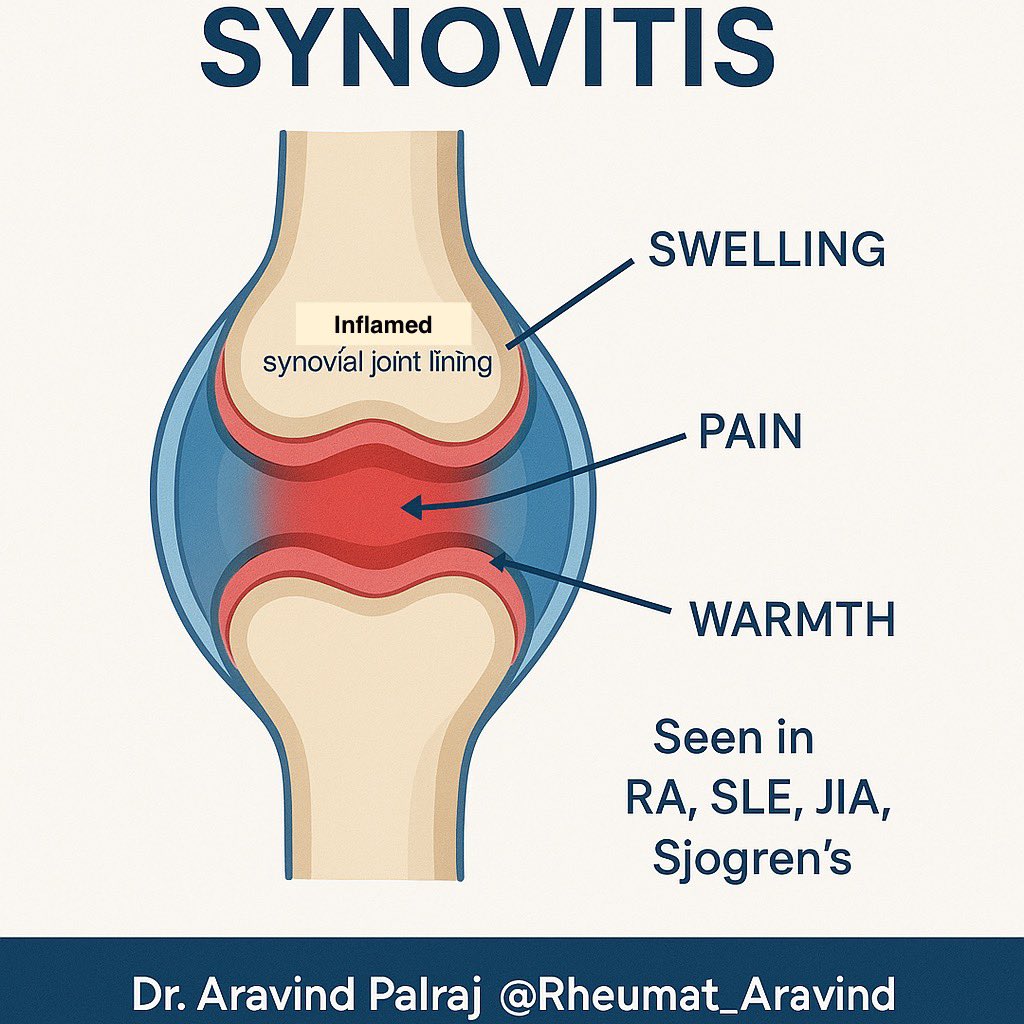
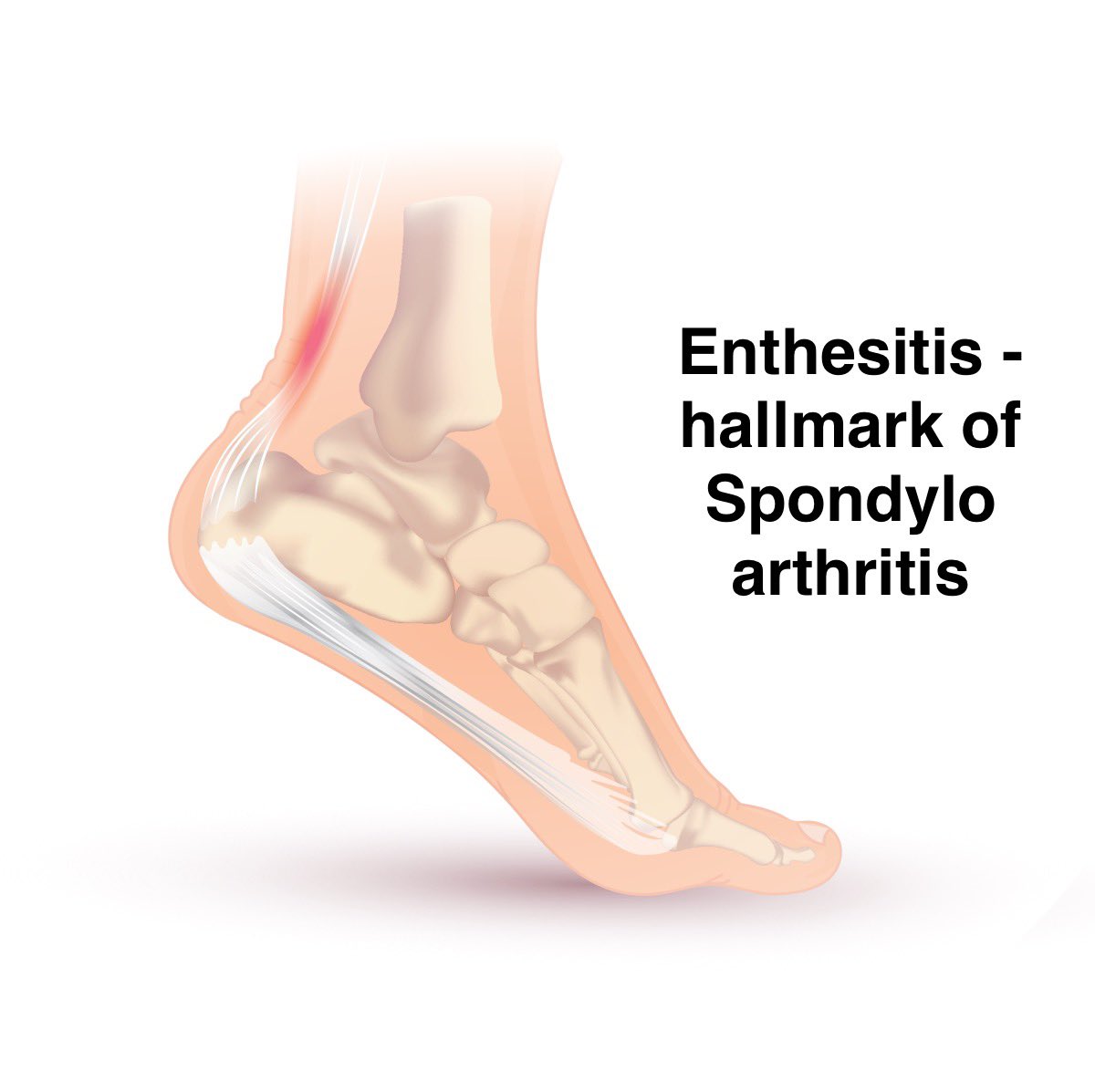
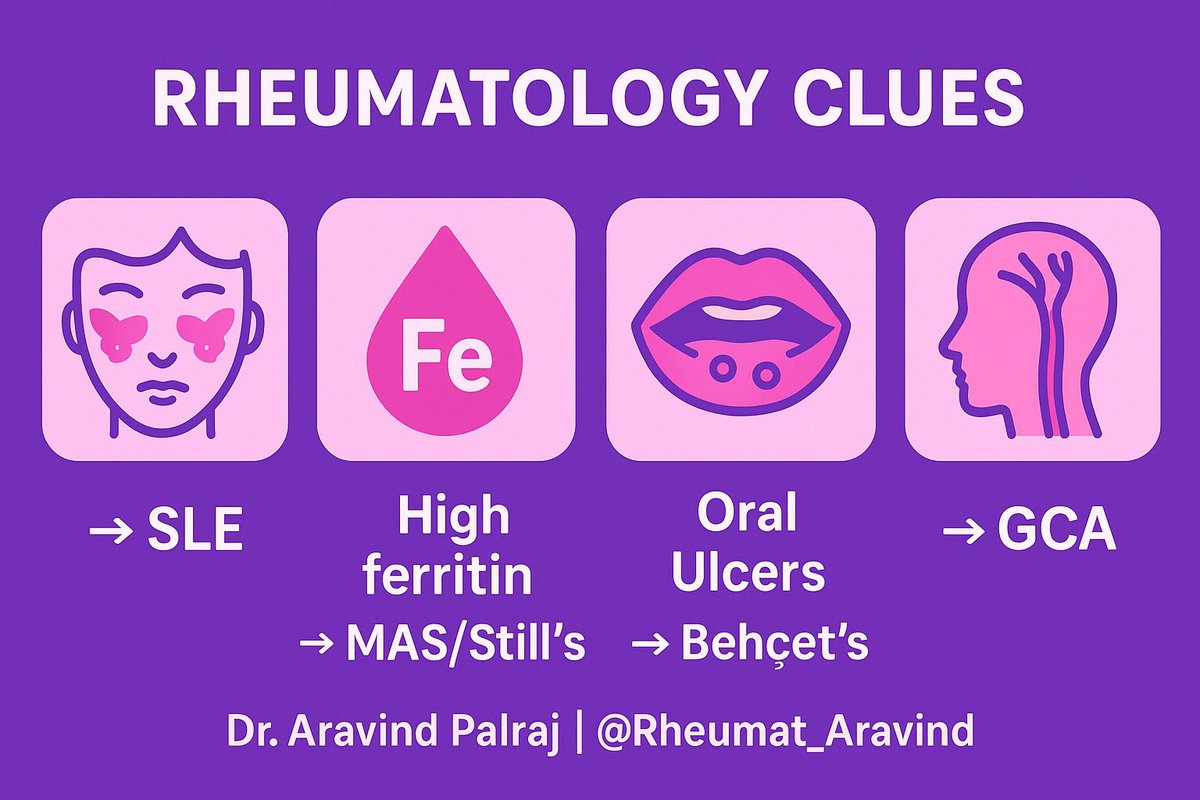
6. Rheumatology clues 🧩
Think autoimmunity when you see:
•Rash + arthritis → SLE, Still’s
•Jaw claudication + ↑ESR → Giant Cell Arteritis
•Recurrent oral/genital ulcers → Behçet’s
•Granulomas → Sarcoidosis
•Cytopenias + high ferritin → MAS / HLH
Think autoimmunity when you see:
•Rash + arthritis → SLE, Still’s
•Jaw claudication + ↑ESR → Giant Cell Arteritis
•Recurrent oral/genital ulcers → Behçet’s
•Granulomas → Sarcoidosis
•Cytopenias + high ferritin → MAS / HLH
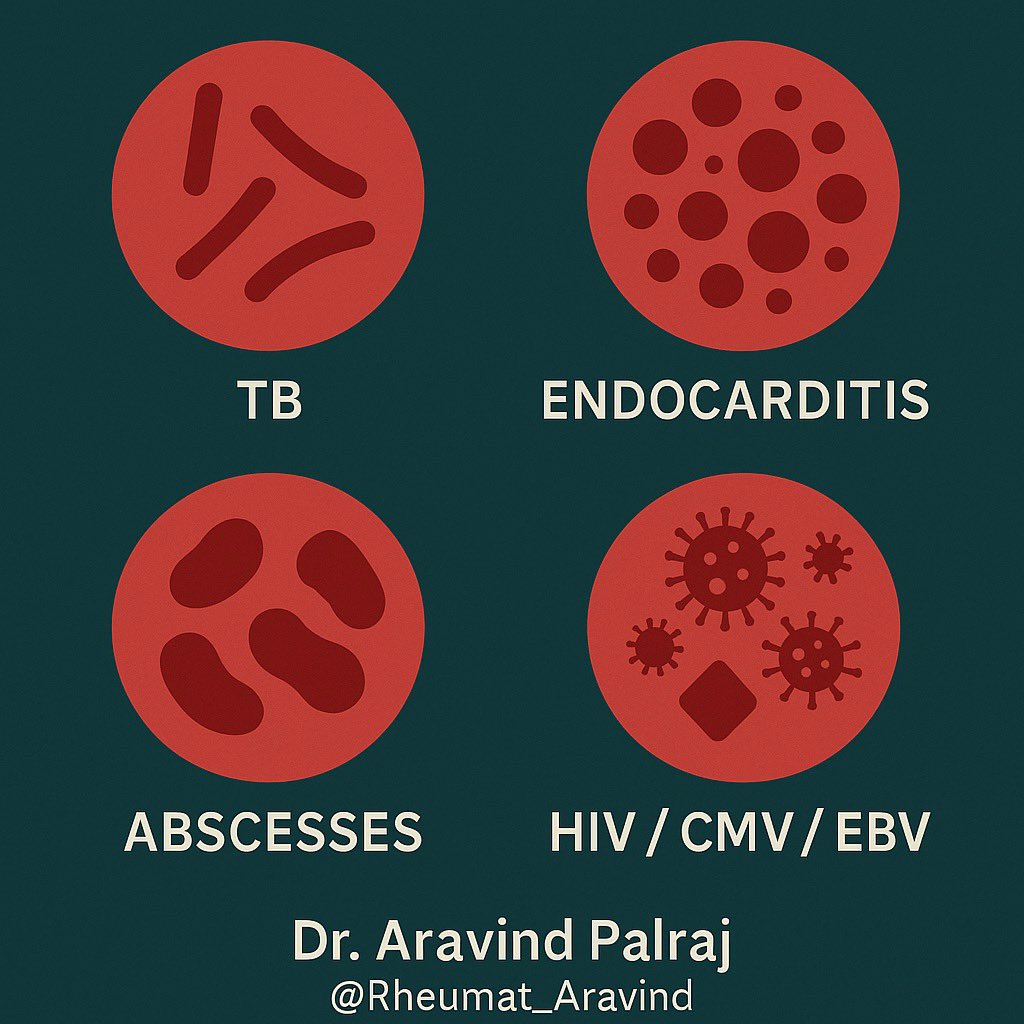
7. Infections to never miss 🦠
•TB (esp. extrapulmonary in India)
•Endocarditis (culture-negative too!)
•Abscesses
•HIV, CMV, EBV
•TB (esp. extrapulmonary in India)
•Endocarditis (culture-negative too!)
•Abscesses
•HIV, CMV, EBV
8. Malignancies 📉
•Lymphoma (often only fever + sweats)
•Leukemia
•Renal cell carcinoma
•Occult solid tumors
•Lymphoma (often only fever + sweats)
•Leukemia
•Renal cell carcinoma
•Occult solid tumors

9. Miscellaneous 🌀
•Drug fever (check timeline!)
•Factitious fever
•Autoinflammatory syndromes (rare, but real)
•Drug fever (check timeline!)
•Factitious fever
•Autoinflammatory syndromes (rare, but real)

10. Practical tips 📝
•Re-examine daily — things evolve.
•Don’t shotgun all tests at once. Stepwise saves money and confusion.
•Always ask: Is the patient sick enough for empirics, or stable enough to wait?
•Re-examine daily — things evolve.
•Don’t shotgun all tests at once. Stepwise saves money and confusion.
•Always ask: Is the patient sick enough for empirics, or stable enough to wait?
11. FUO is not just a diagnostic puzzle.
Patients suffer from uncertainty, repeated admissions, financial stress.
👉 Keep communication clear, show empathy, and reassure that persistence pays off.
Patients suffer from uncertainty, repeated admissions, financial stress.
👉 Keep communication clear, show empathy, and reassure that persistence pays off.
12. Takeaway
FUO is not a “black box.”
Think Infection – Malignancy – Autoimmune – Miscellaneous, keep re-evaluating, and most cases reveal themselves with patience + pattern recognition.
✨ Follow Dr. Aravind Palraj | @Rheumat_Aravind for more practical threads blending Internal Medicine & Rheumatology.
FUO is not a “black box.”
Think Infection – Malignancy – Autoimmune – Miscellaneous, keep re-evaluating, and most cases reveal themselves with patience + pattern recognition.
✨ Follow Dr. Aravind Palraj | @Rheumat_Aravind for more practical threads blending Internal Medicine & Rheumatology.
• • •
Missing some Tweet in this thread? You can try to
force a refresh