A NEW review explores how SARS-CoV-2 may influence cancer risk.
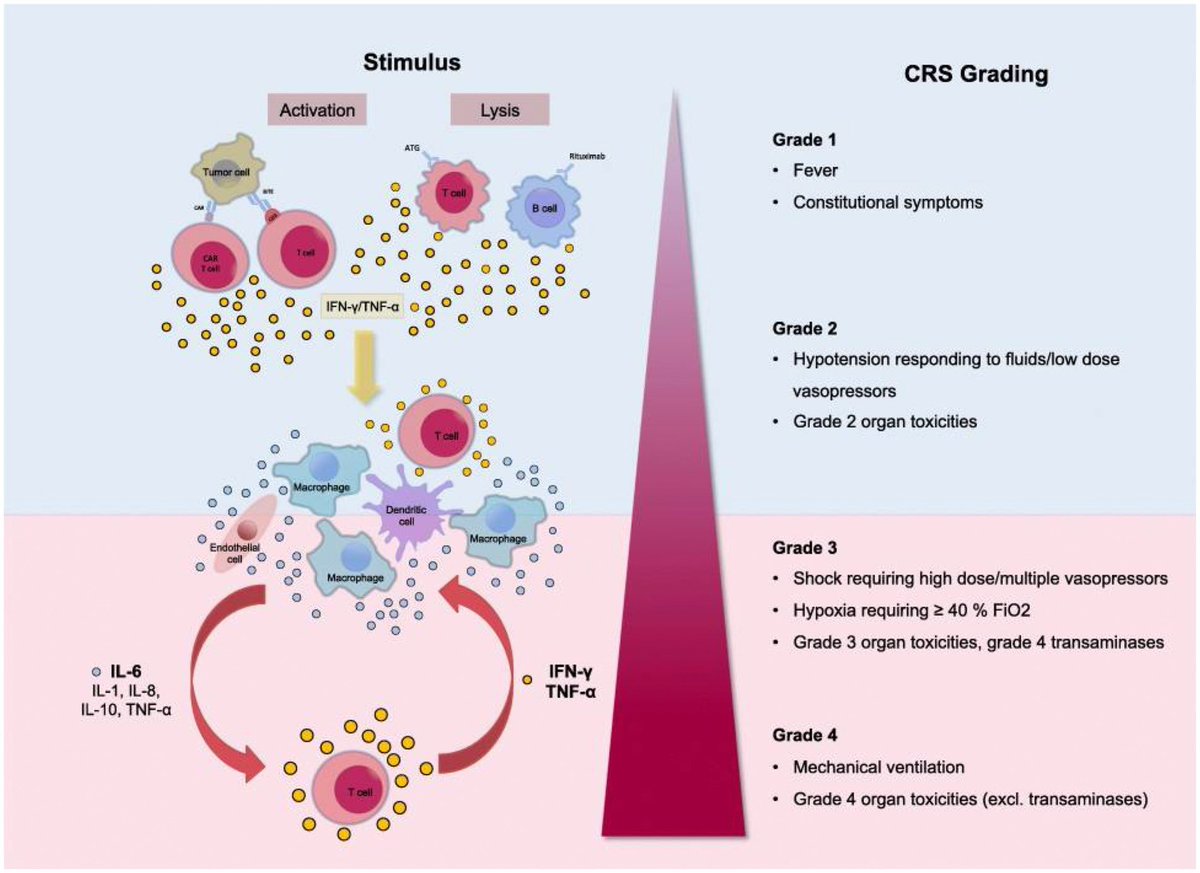
➡️ Unlike classical oncogenic viruses, it doesn’t insert viral oncogenes. Instead, its proteins:
-Inhibit tumor suppressors
-Activate growth, survival & inflammation pathways
👉 Potential role in cancer initiation & progression. 1/
➡️ Unlike classical oncogenic viruses, it doesn’t insert viral oncogenes. Instead, its proteins:
-Inhibit tumor suppressors
-Activate growth, survival & inflammation pathways
👉 Potential role in cancer initiation & progression. 1/

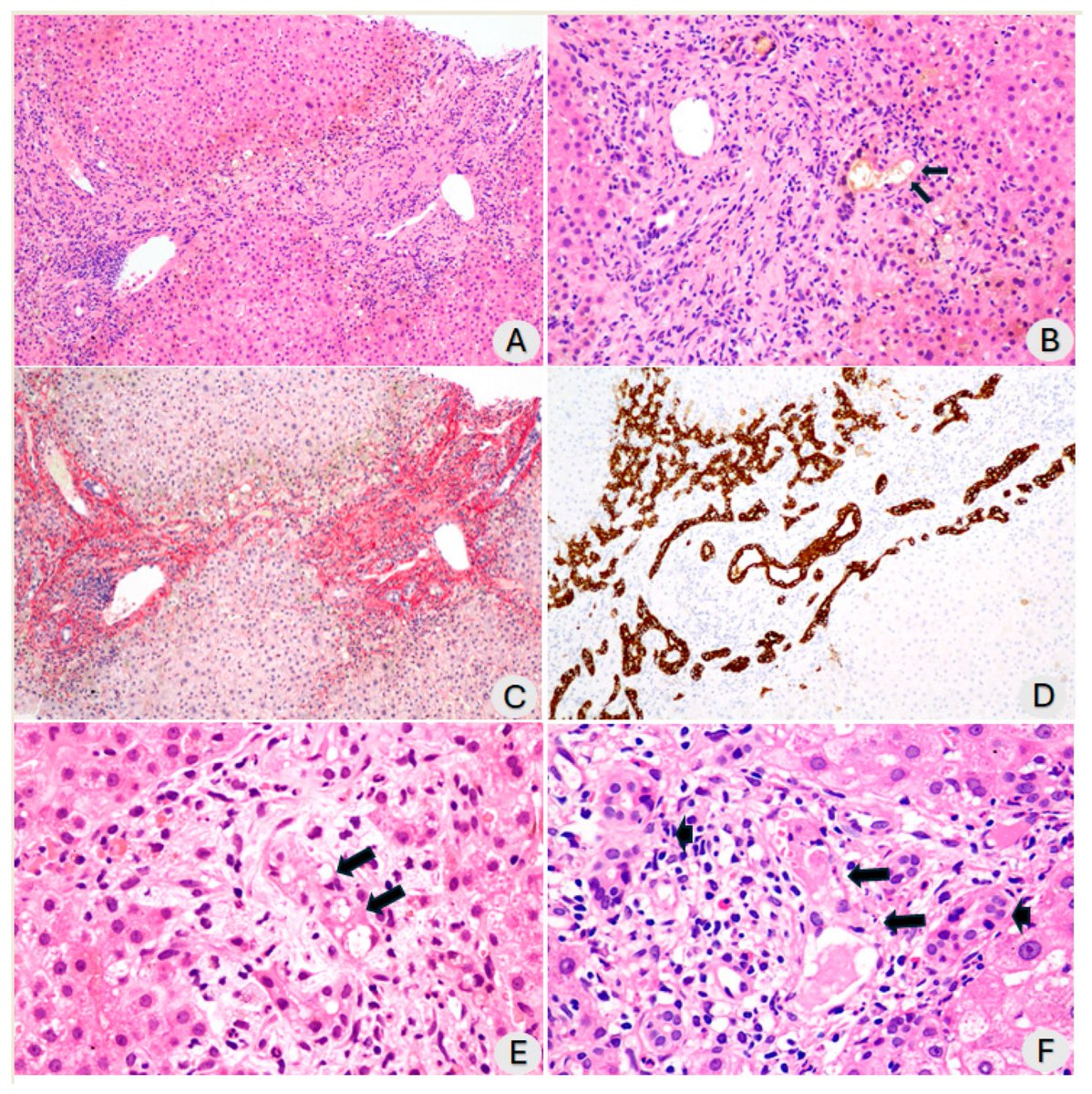
Bioinformatic & experimental studies show direct interactions between viral proteins and host cellular components tied to cancer hallmarks.
➡️ These mechanisms could contribute to initiation, promotion, and progression of tumors, raising the possibility that SARS-CoV-2 may act as an oncovirus.
👇The figure illustrates various key oncogenic signaling molecules or pathways targeted by SARS-CoV-2 NSP, N, M and S protein. The activation of oncogenic pathways can lead to the conversion of a normal cell into a cancer cell. 2/
➡️ These mechanisms could contribute to initiation, promotion, and progression of tumors, raising the possibility that SARS-CoV-2 may act as an oncovirus.
👇The figure illustrates various key oncogenic signaling molecules or pathways targeted by SARS-CoV-2 NSP, N, M and S protein. The activation of oncogenic pathways can lead to the conversion of a normal cell into a cancer cell. 2/

The shared mechanisms between SARS-CoV-2 and key hallmarks of cancer including sustained proliferative signaling, resisting cell death, genomic instability, dysregulated cellular metabolism and epigenetic reprogramming.
👇The figure highlights how SARS-CoV-2 interacts with critical oncogenic signaling molecules or pathways. Specific SARS-CoV-2 proteins involved in these processes are marked. 3/
👇The figure highlights how SARS-CoV-2 interacts with critical oncogenic signaling molecules or pathways. Specific SARS-CoV-2 proteins involved in these processes are marked. 3/

Understanding these pathways is important to guide COVID-19 and cancer research and to develop strategies to reduce its long-term cancer impact.
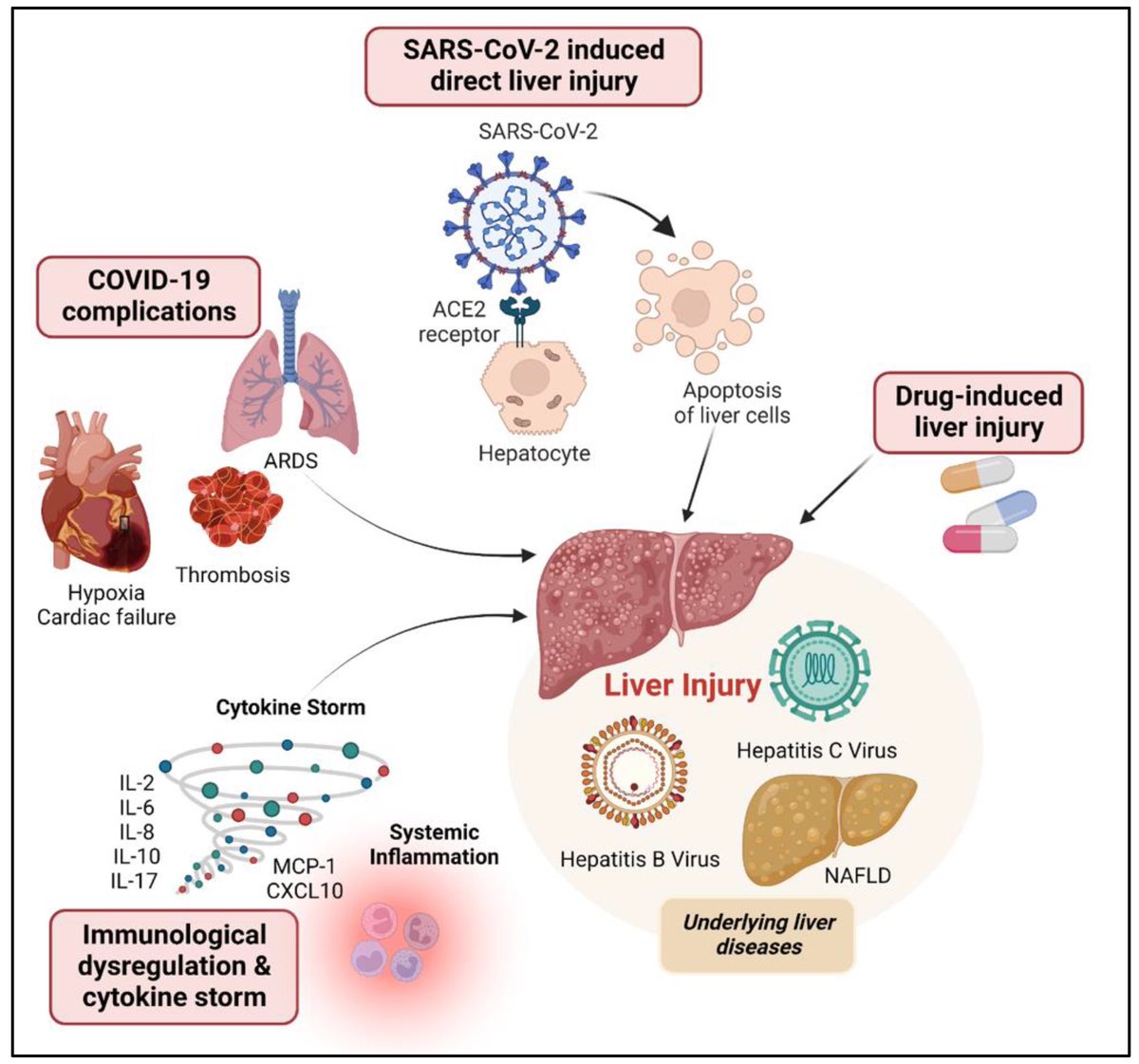
👇 The impact of SARS-CoV-2 on tumor-related inflammatory markers and mechanisms of immune evasion is depicted in the figure, illustrating how viral proteins interact with critical molecular targets within inflammatory and immune pathways. 4/
👇 The impact of SARS-CoV-2 on tumor-related inflammatory markers and mechanisms of immune evasion is depicted in the figure, illustrating how viral proteins interact with critical molecular targets within inflammatory and immune pathways. 4/

The alterations in mechanisms within normal cells infected with SARS-CoV-2, drawing parallels to changes observed in cancer cells.
👇The figure emphasizes the relationship of the alterations to key cancer-related processes, including metastasis, invasion and angiogenesis. Specific pathways and molecular changes induced by SARS-CoV-2 infection that mirror oncogenic transformations are highlighted. 5/
👇The figure emphasizes the relationship of the alterations to key cancer-related processes, including metastasis, invasion and angiogenesis. Specific pathways and molecular changes induced by SARS-CoV-2 infection that mirror oncogenic transformations are highlighted. 5/

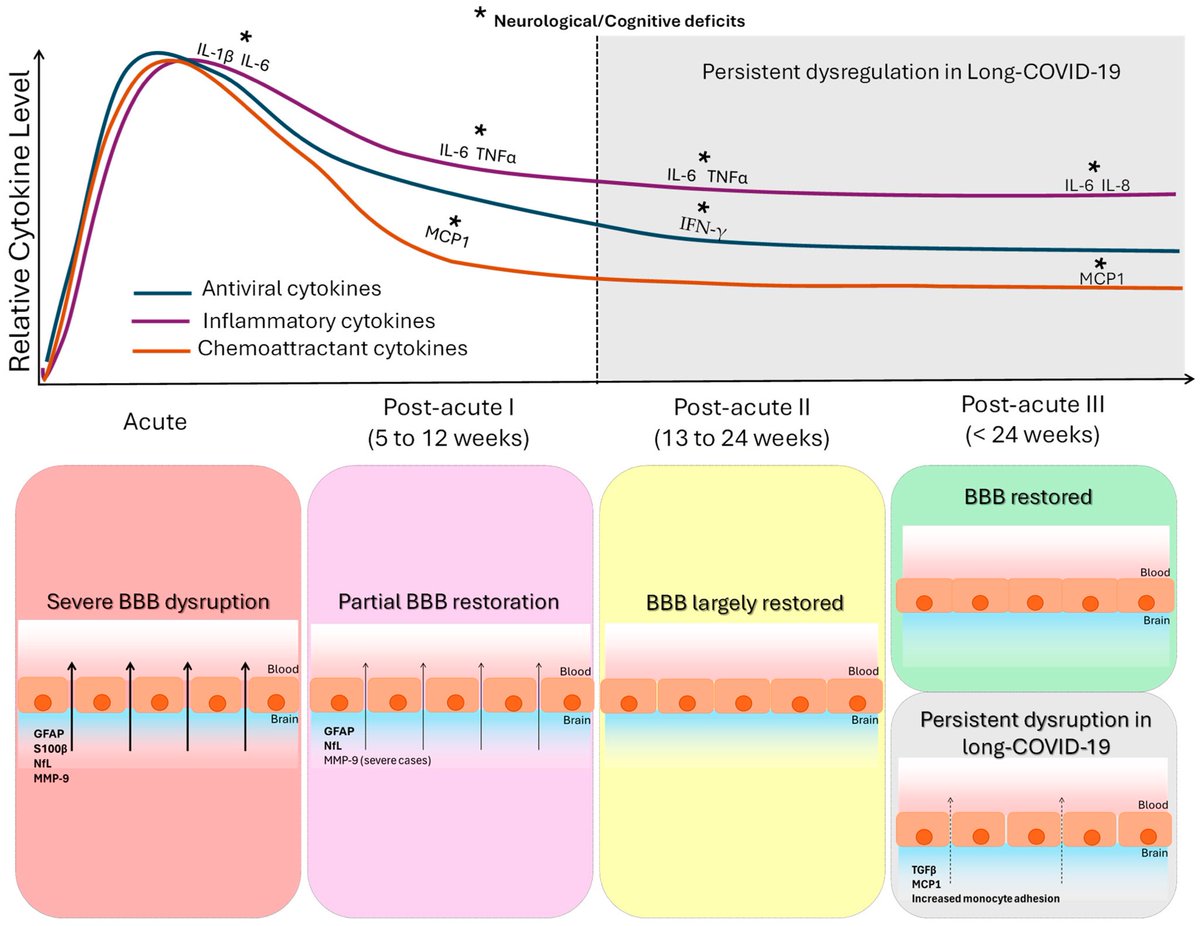
The activation of NLRP3 inflammasomes by the N protein of SARS-CoV-2 and the dysregulation of the Renin–Angiotensin–Aldosterone System (RAAS). The activation of NLRP3 led to the cancer-causing hallmarks.
👇The figure details how these pathways contribute to processes such as deregulated cellular metabolism, tumor-promoting inflammation, inducing angiogenesis and metastasis. 6/
👇The figure details how these pathways contribute to processes such as deregulated cellular metabolism, tumor-promoting inflammation, inducing angiogenesis and metastasis. 6/

The correlation of COVID-19 and cancer poses significant challenges, as cancer patients are immunocompromised and more susceptible to viral infections. This dual burden has spurred extensive research to understand the correlation between the two diseases and to develop suitable therapeutic strategies. 7/

While no direct link between COVID and cancer has been proven, the researchers call for careful monitoring of long-term survivors for potential malignancy risk.
👉 Takeaway: SARS-CoV-2 proteins can interfere with tumor suppressors and activate pro-cancer pathways, suggesting a potential role in carcinogenesis that needs further study. 8/8
H/T: @CatchTheBaby
biosignaling.biomedcentral.com/articles/10.11…
👉 Takeaway: SARS-CoV-2 proteins can interfere with tumor suppressors and activate pro-cancer pathways, suggesting a potential role in carcinogenesis that needs further study. 8/8
H/T: @CatchTheBaby
biosignaling.biomedcentral.com/articles/10.11…

• • •
Missing some Tweet in this thread? You can try to
force a refresh