Cholesterol Confessions of an MD PhD Lean Mass Hyper-Responder. (link at the end)
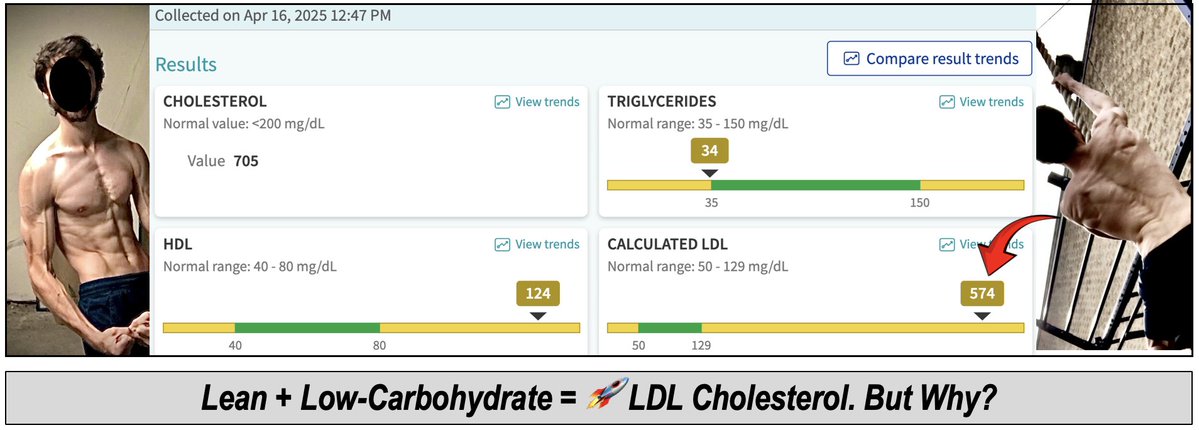
1/7) I gave my cardiologist a heart attack. Well—not literally. But when a cardiologist sees an LDL cholesterol of 574 mg/dL, their eyes bug out like they’re a human-sized fruit fly.
And I understand why.
That number is higher than anything most doctors have seen in their entire careers. And it’s scary. It is.
It rivals levels found in “homozygous familial hypercholesterolemia,” a rare genetic disorder—occurring in ~1 in a million—that can cause fatal heart attacks in children as young as eight.
But I don’t have familial hypercholesterolemia.
Something very different is going on inside my body…
1/7) I gave my cardiologist a heart attack. Well—not literally. But when a cardiologist sees an LDL cholesterol of 574 mg/dL, their eyes bug out like they’re a human-sized fruit fly.
And I understand why.
That number is higher than anything most doctors have seen in their entire careers. And it’s scary. It is.
It rivals levels found in “homozygous familial hypercholesterolemia,” a rare genetic disorder—occurring in ~1 in a million—that can cause fatal heart attacks in children as young as eight.
But I don’t have familial hypercholesterolemia.
Something very different is going on inside my body…
2/7) Today’s letter is an overdue ~3000-word essay on:
🩸My lipid levels
🩸Background on people like me
🩸Disclosure on my personal choices
🩸What I'm doing next
staycuriousmetabolism.substack.com/p/im-a-harvard…
Warning: It’s intense. And it’s only the beginning.
Caution: Please do not take this as medical advice or even the suggestion of such. Instead, my purpose is providing discloses it to reveal how I think, not what to think.
Note: The back half of the letter is currently only available for premium subscribers. For now, I’m reserving the most complex and intense details for a smaller, highly committed audience. Call it an intellectual stress test.
🩸My lipid levels
🩸Background on people like me
🩸Disclosure on my personal choices
🩸What I'm doing next
staycuriousmetabolism.substack.com/p/im-a-harvard…
Warning: It’s intense. And it’s only the beginning.
Caution: Please do not take this as medical advice or even the suggestion of such. Instead, my purpose is providing discloses it to reveal how I think, not what to think.
Note: The back half of the letter is currently only available for premium subscribers. For now, I’m reserving the most complex and intense details for a smaller, highly committed audience. Call it an intellectual stress test.
3/7) Still, at a high-level here in this thread, I want to reinforce a few points:
🚨First, people like me – lean mass hyper-responders (LMHR) on ketogenic diets – are unlike any other population ever studies with high LDL and ApoB.
🧬Our lipid levels are NOT the result of a congenital genetic lipid disorder (like familial hypercholesterolemia). And, generally, LMHR are in excellent metabolic health.
For these reasons, it’s in appropriate to extrapolate from the existing “preponderance of evidence” any certain claims with respect to cardiovascular risk to people like me.
🚨First, people like me – lean mass hyper-responders (LMHR) on ketogenic diets – are unlike any other population ever studies with high LDL and ApoB.
🧬Our lipid levels are NOT the result of a congenital genetic lipid disorder (like familial hypercholesterolemia). And, generally, LMHR are in excellent metabolic health.
For these reasons, it’s in appropriate to extrapolate from the existing “preponderance of evidence” any certain claims with respect to cardiovascular risk to people like me.
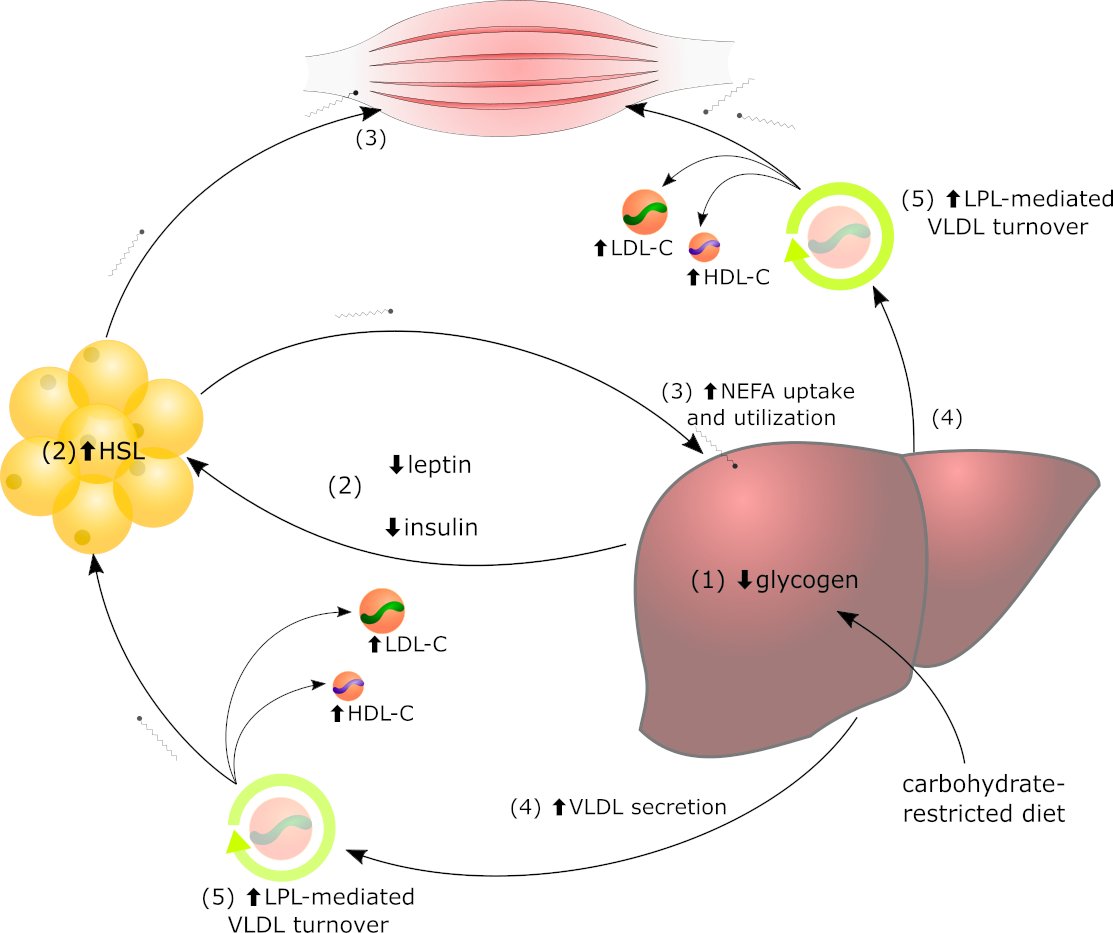
4/7) It’s also worth noting this is not simply a genetic saturated fat or fiber phenomenon.
I can drop saturated fat and fiber and increase my cholesterol or increase saturated fat and fiber and drop my cholesterol.
Instead, the phenomenon appears to be the results of an adaptive lipid energy-trafficking system (The lipid energy model).

I can drop saturated fat and fiber and increase my cholesterol or increase saturated fat and fiber and drop my cholesterol.
Instead, the phenomenon appears to be the results of an adaptive lipid energy-trafficking system (The lipid energy model).

5/7) Also interesting, it appears patients can interconvert from overweight to LMHR. here are numerous examples, but here is one that I have permission to share:
My colleague, Dr Professor @AdrianSotoMota MD PhD, cared for a 60-year-old male patient with type 2 diabetes. The patient adopted a ketogenic diet and his BMI steadily decreased from 29.5 kg/m2 to 24.5g/m2. During his weight loss journey, his LDL-C remained ~95 mg/dl until he reached the “healthy” BMI range (< 25 kg/m2). Then, his LDL-C jumped to 183 mg/dl.
So, is this man’s heart healthier for having lost weight?
Or, in this case, did losing excess body fat increase his cardiovascular risk? Open question.
My colleague, Dr Professor @AdrianSotoMota MD PhD, cared for a 60-year-old male patient with type 2 diabetes. The patient adopted a ketogenic diet and his BMI steadily decreased from 29.5 kg/m2 to 24.5g/m2. During his weight loss journey, his LDL-C remained ~95 mg/dl until he reached the “healthy” BMI range (< 25 kg/m2). Then, his LDL-C jumped to 183 mg/dl.
So, is this man’s heart healthier for having lost weight?
Or, in this case, did losing excess body fat increase his cardiovascular risk? Open question.
6/7) Finally, before I direct you to the essay, please note Lipid Lowering Medications are NOT benign.
Statins and other cholesterol lowering drugs can have negative consequences. Some known, and some still unknown.
On the latter, powerful medications should not be innocent until proven guilty.
The result is that individuals within understudied populations are often left making difficult personal choices because the risk-benefit analysis is informed by unknown risks and unknown benefits.
Statins and other cholesterol lowering drugs can have negative consequences. Some known, and some still unknown.
On the latter, powerful medications should not be innocent until proven guilty.
The result is that individuals within understudied populations are often left making difficult personal choices because the risk-benefit analysis is informed by unknown risks and unknown benefits.
7/7) Today’s letter gets into the weeds. I discuss mechanisms, risks and personal decision making.
staycuriousmetabolism.substack.com/p/im-a-harvard…
I disclose why I’ve made the choices I’ve made (and am still making) and provide cautions on common logical traps. It’s a dense on.
It’s raw and honest and it’s going to upset some people. But to those who can check their gut reactions (MD, PhD and lay persons alike) and consider with curiosity, I think there is much to be learned…
staycuriousmetabolism.substack.com/p/im-a-harvard…
I disclose why I’ve made the choices I’ve made (and am still making) and provide cautions on common logical traps. It’s a dense on.
It’s raw and honest and it’s going to upset some people. But to those who can check their gut reactions (MD, PhD and lay persons alike) and consider with curiosity, I think there is much to be learned…
• • •
Missing some Tweet in this thread? You can try to
force a refresh