
MD PhD, Harvard-Oxford. Metabolic Health Enthusiast. “Stay Curious” Letter: https://t.co/YoPdkV6tkd YouTube: https://t.co/mnop8pYnkq
15 subscribers
How to get URL link on X (Twitter) App



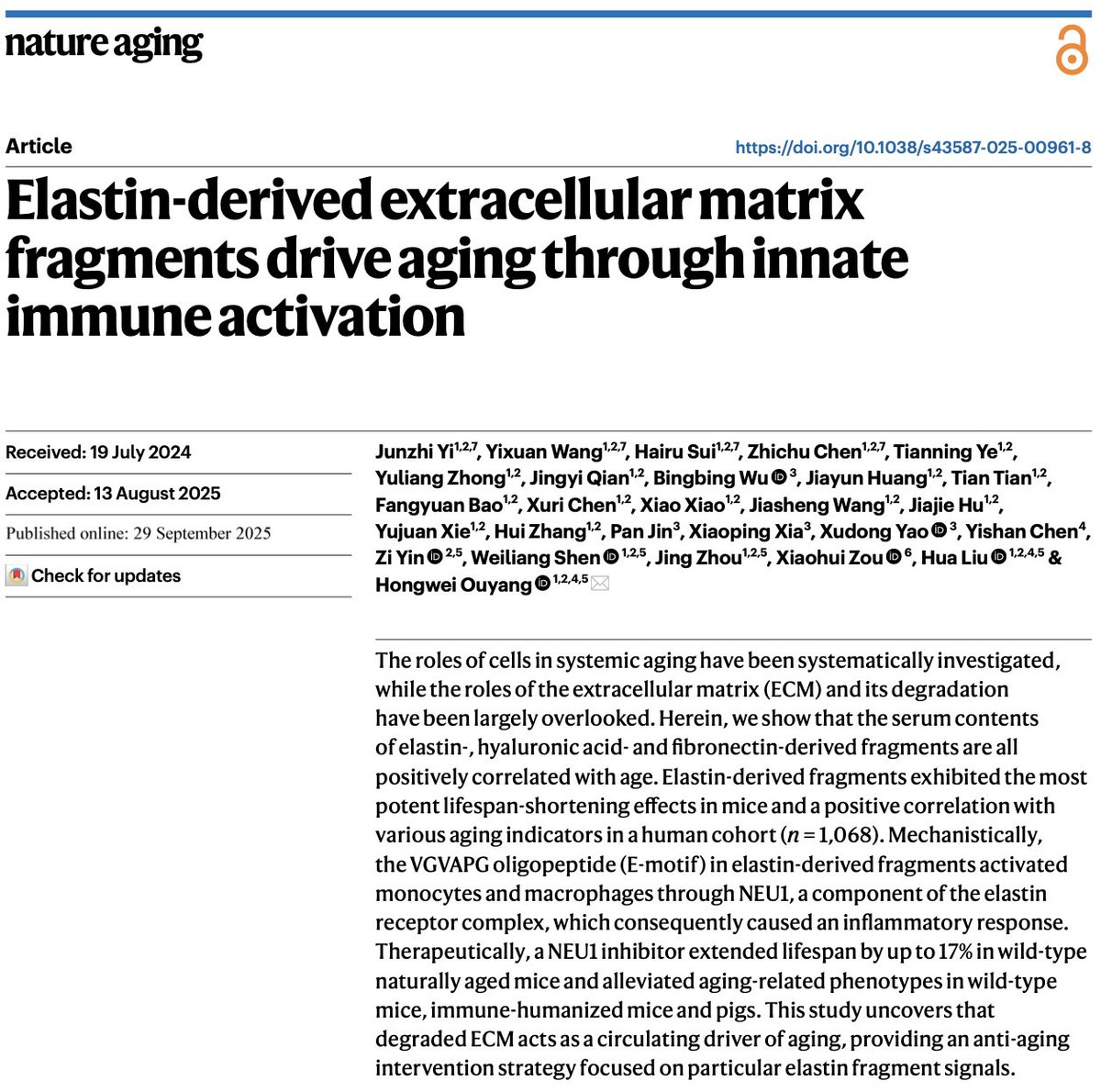 2/6) The scaffolding beneath your skin, made of collagen, elastin, and other proteins is called the “Extracellular Matrix” (ECM).
2/6) The scaffolding beneath your skin, made of collagen, elastin, and other proteins is called the “Extracellular Matrix” (ECM).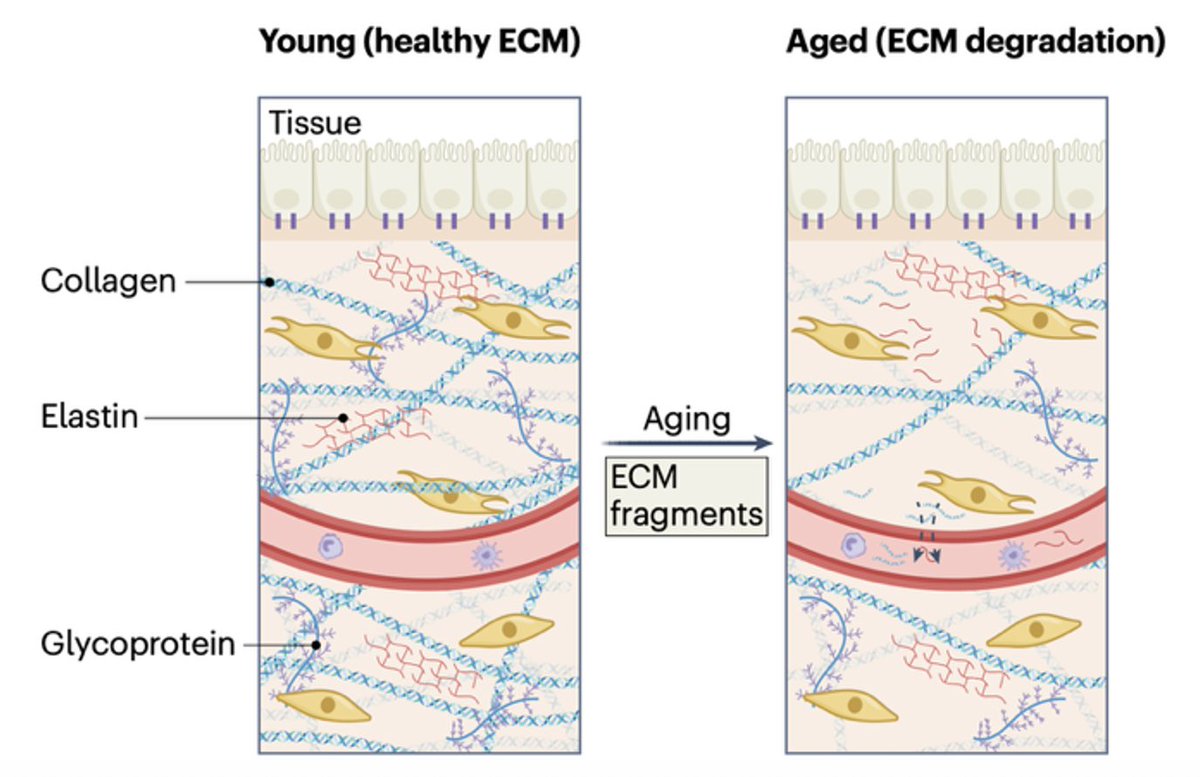
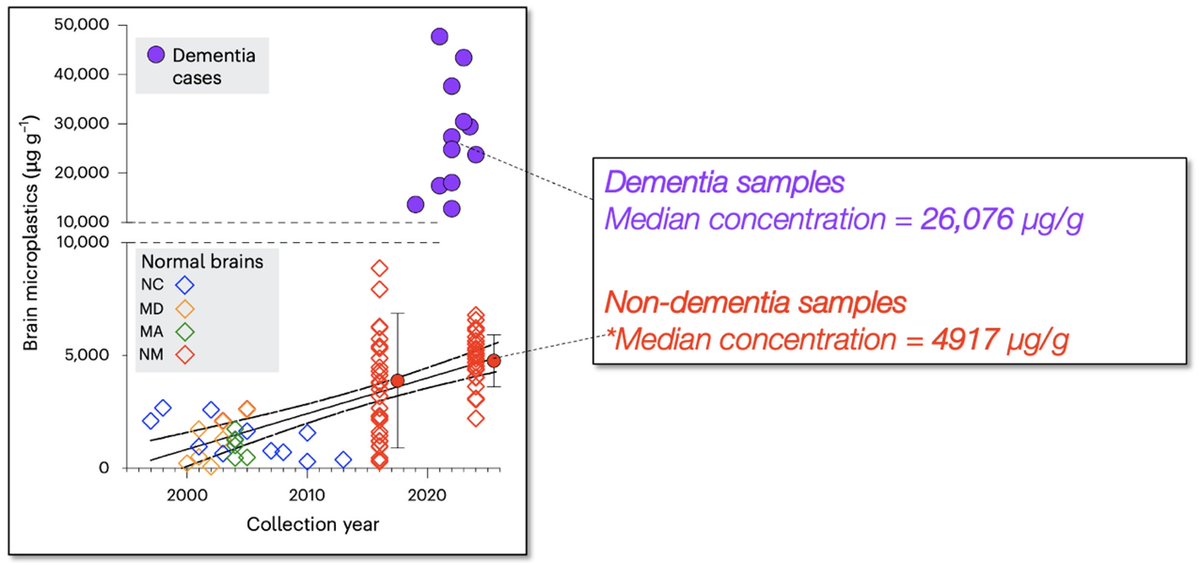
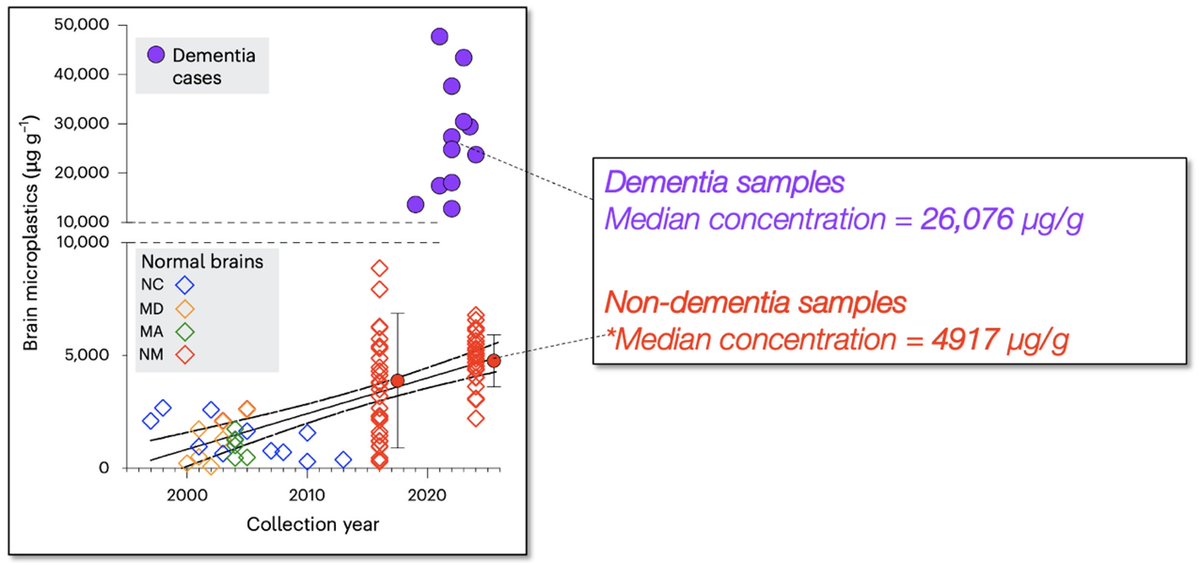 2/5) The researchers behind this work hypothesize that the exponentially increasing concentrations of micro- and nanoplastics in the environment are driving a parallel increase in plastic accumulation in the human brain.
2/5) The researchers behind this work hypothesize that the exponentially increasing concentrations of micro- and nanoplastics in the environment are driving a parallel increase in plastic accumulation in the human brain.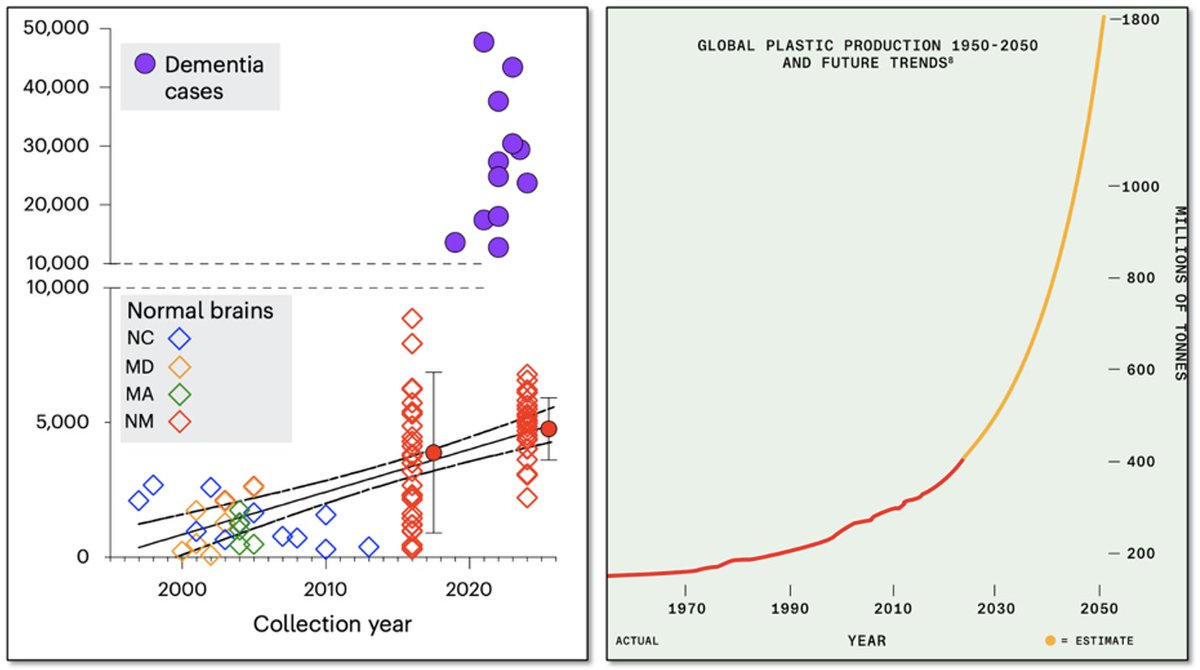
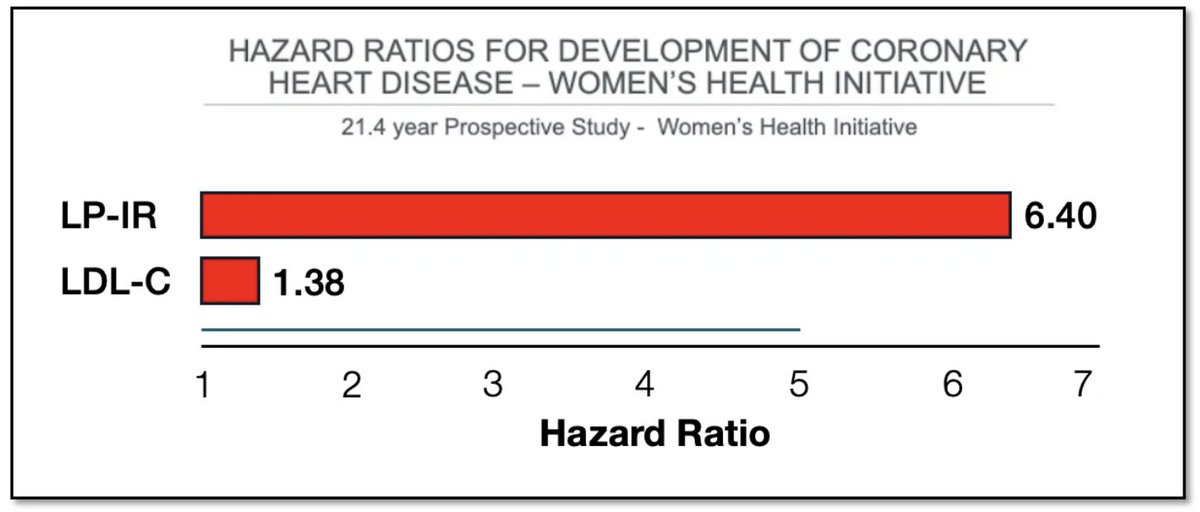
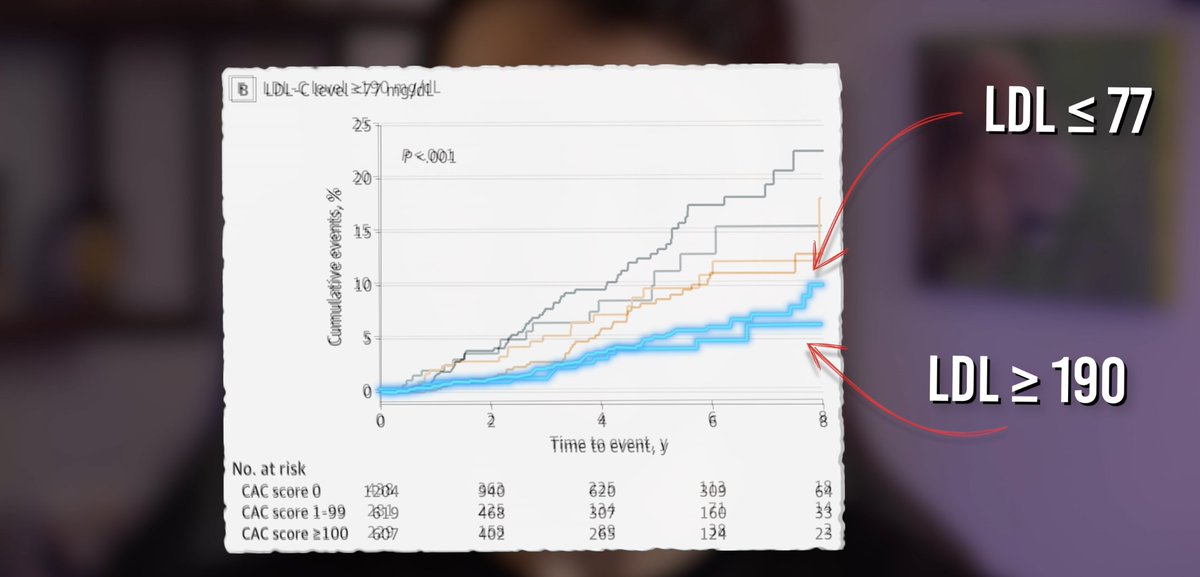
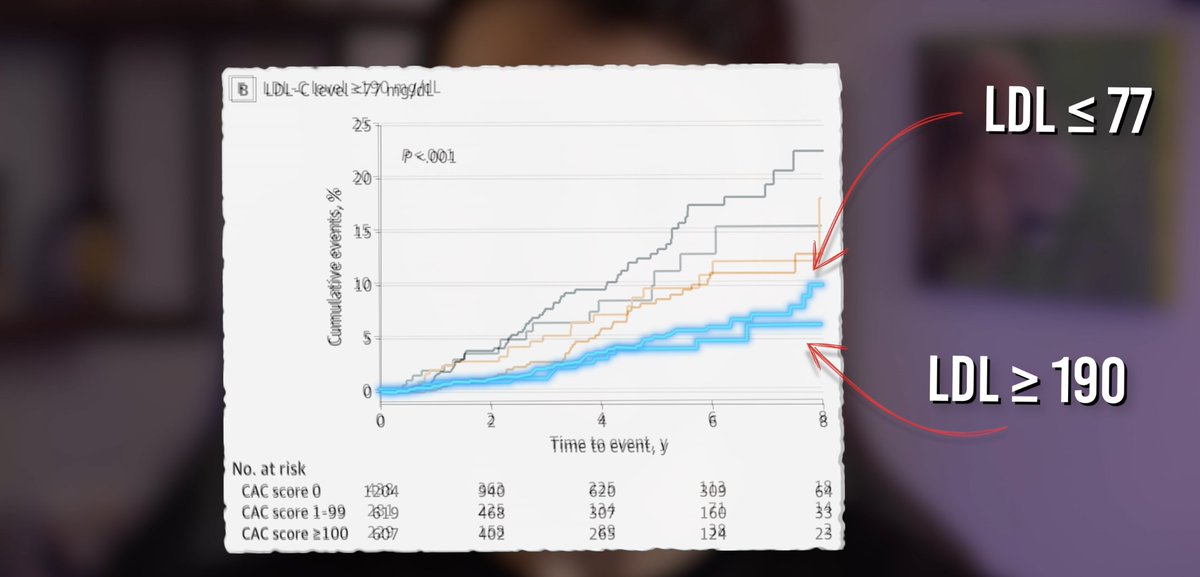
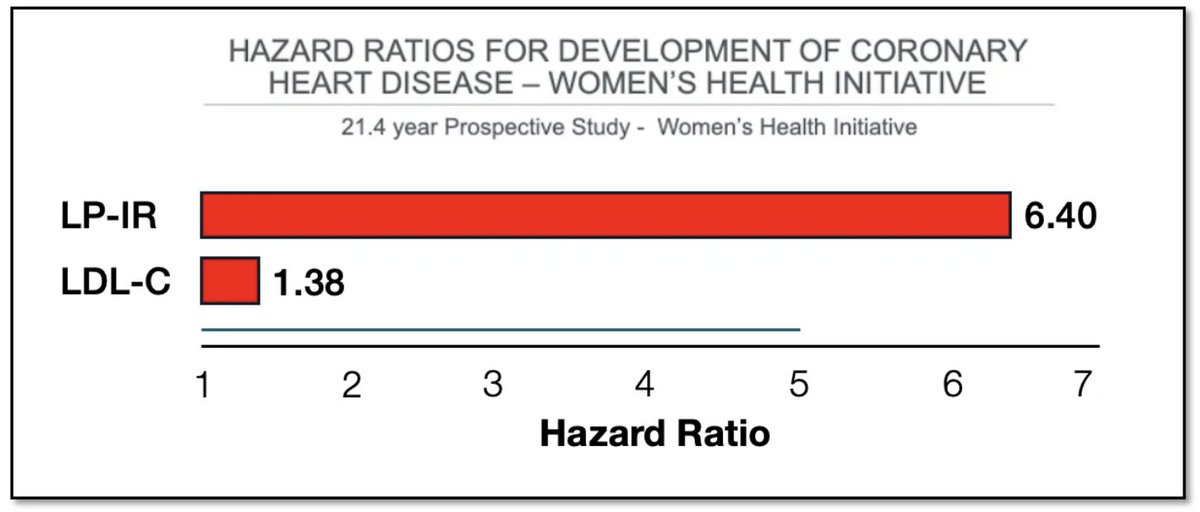 2/4) So why does LDL get all the attention?
2/4) So why does LDL get all the attention?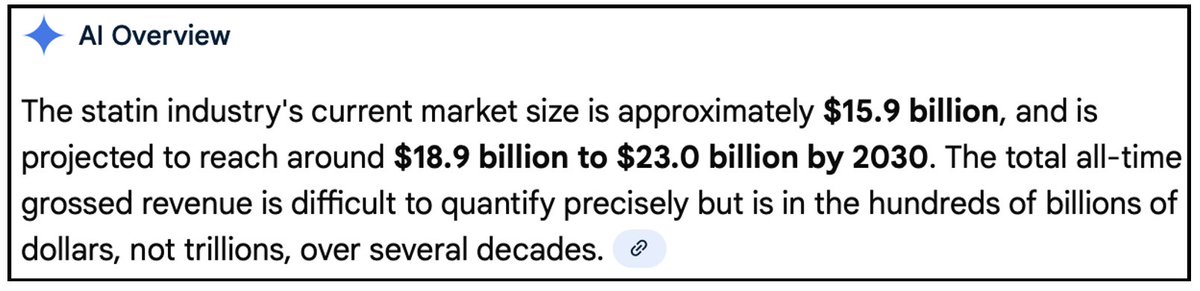

 2/8) Formulation: I’d give it a 3/10.
2/8) Formulation: I’d give it a 3/10.
 2/12) The Minnesota Coronary Experiment was a randomized controlled trial conducted between 1968 and 1973 that enrolled 9,423 men and women across six mental hospitals and one nursing home.
2/12) The Minnesota Coronary Experiment was a randomized controlled trial conducted between 1968 and 1973 that enrolled 9,423 men and women across six mental hospitals and one nursing home.
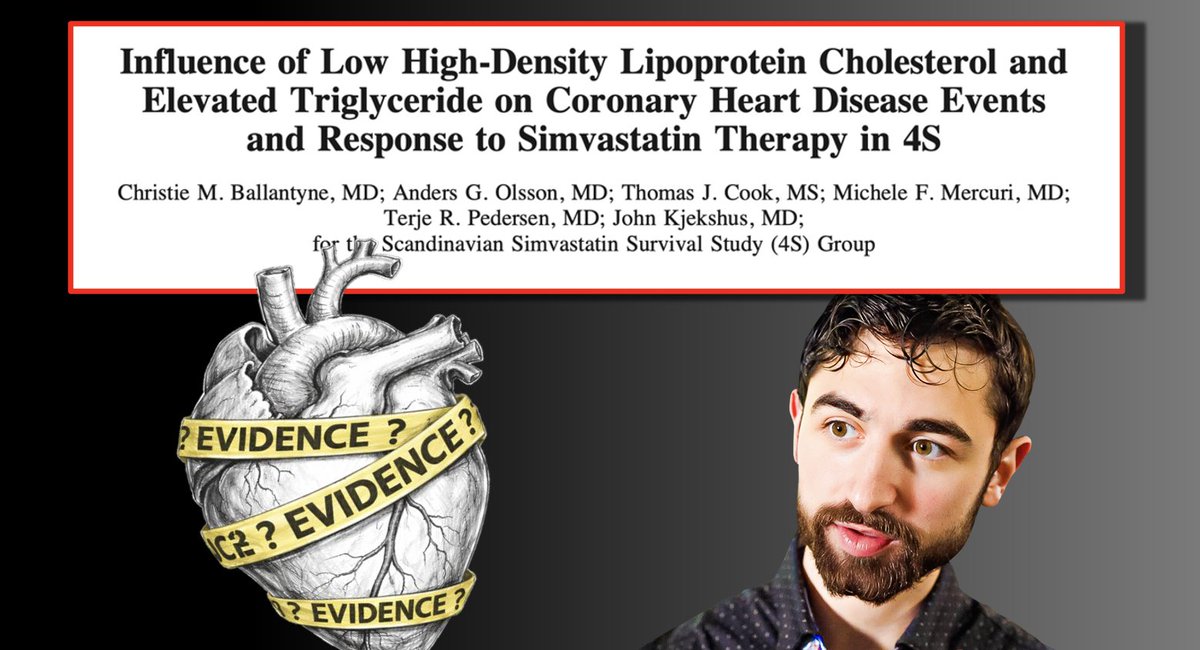
 2/12) According to cardiologists, the 4S trial is widely regarded as the study that launched the statin era.
2/12) According to cardiologists, the 4S trial is widely regarded as the study that launched the statin era.
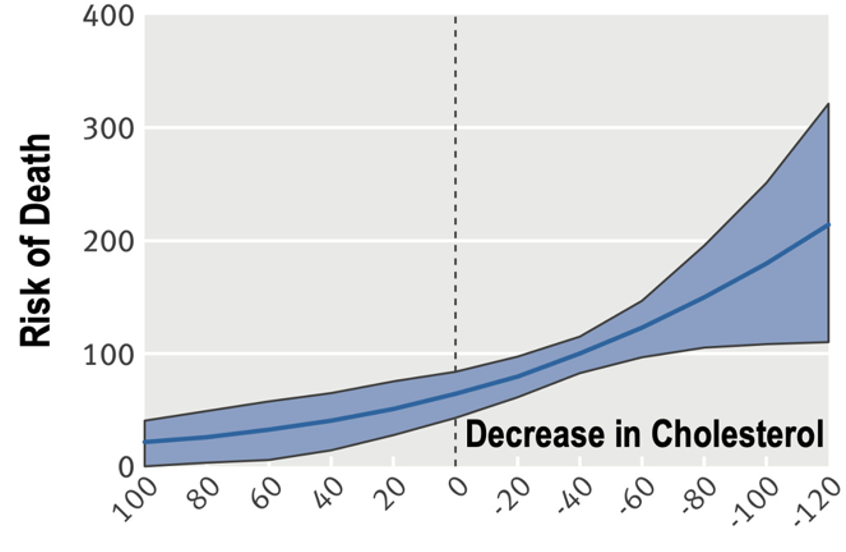
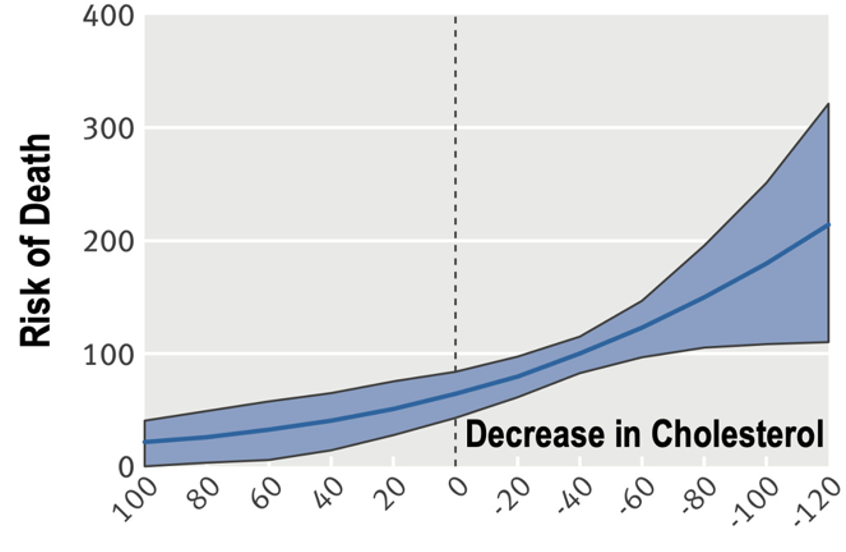
 2/9) Here's where I want to start: The three dumbest words in medicine are: “Lower is better.”
2/9) Here's where I want to start: The three dumbest words in medicine are: “Lower is better.”
 2/8) The logic was straightforward:
2/8) The logic was straightforward:
 2/7) How can one recommend:
2/7) How can one recommend: 
 2/10) Main Point #1: Causality is Overrated
2/10) Main Point #1: Causality is Overrated

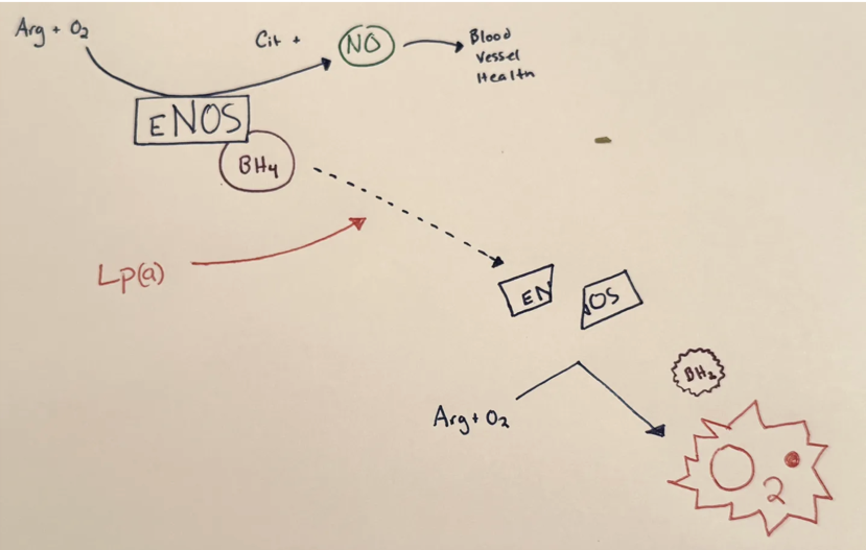
 2/6) In atherosclerosis, macrophages in the artery wall take up too much oxidized LDL.
2/6) In atherosclerosis, macrophages in the artery wall take up too much oxidized LDL. 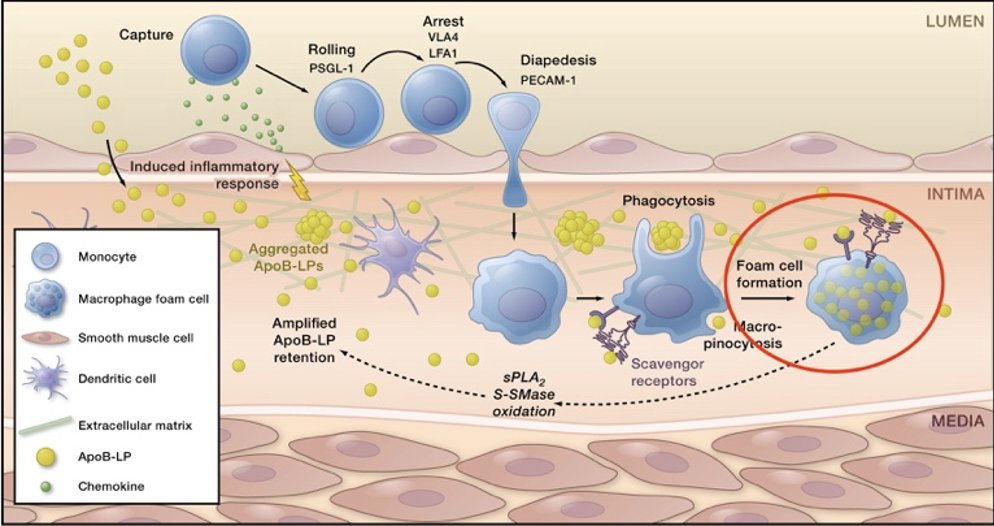
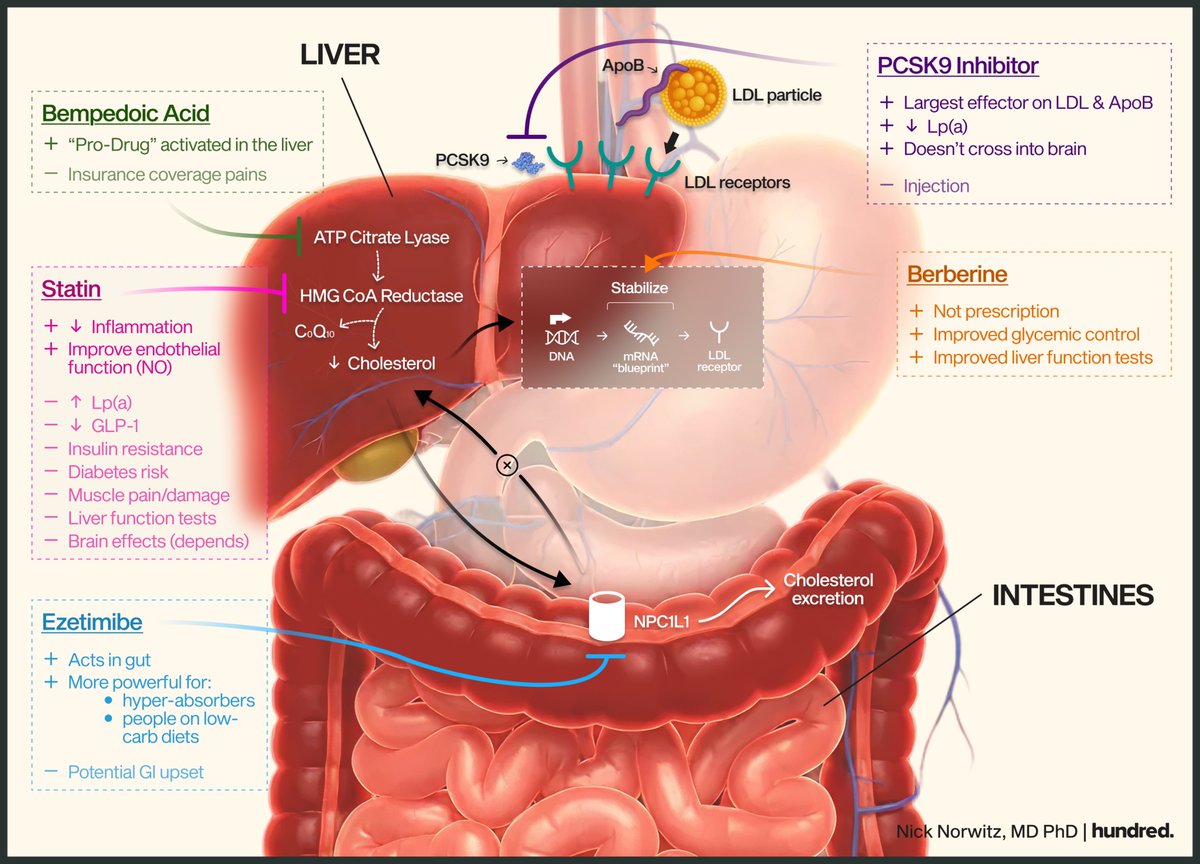
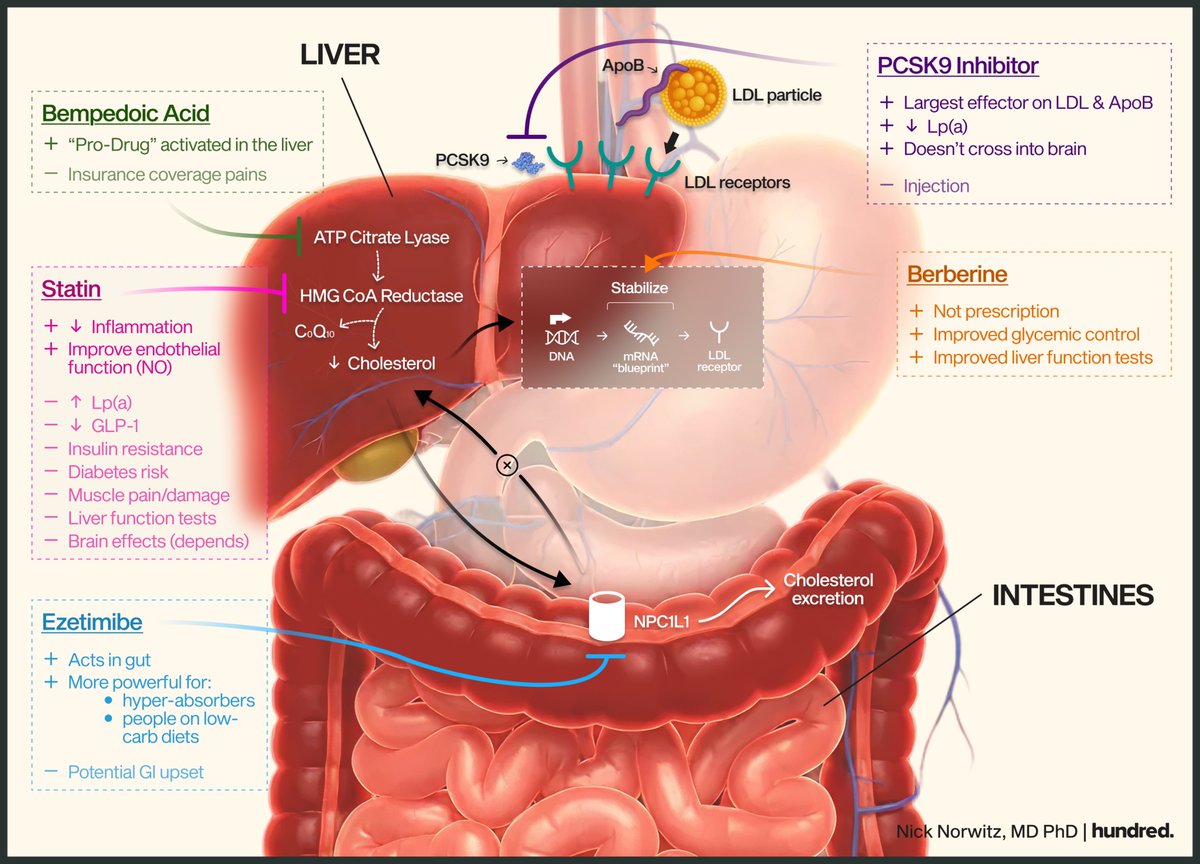
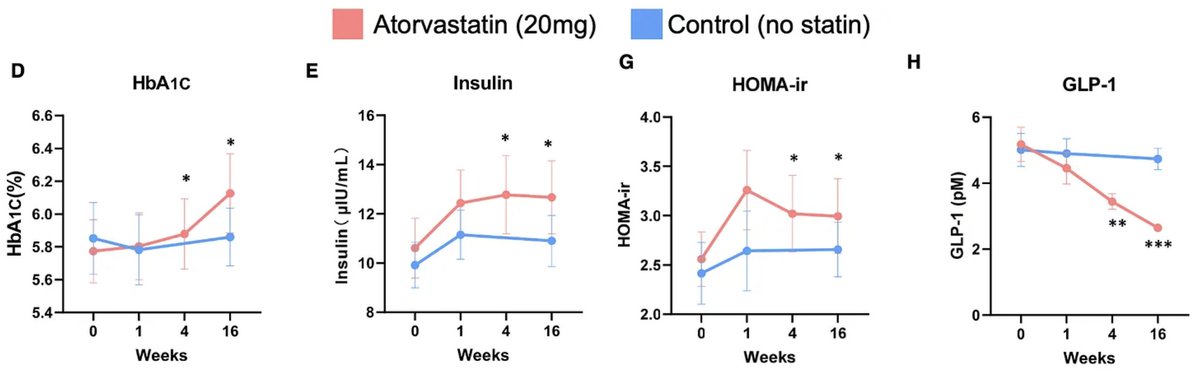
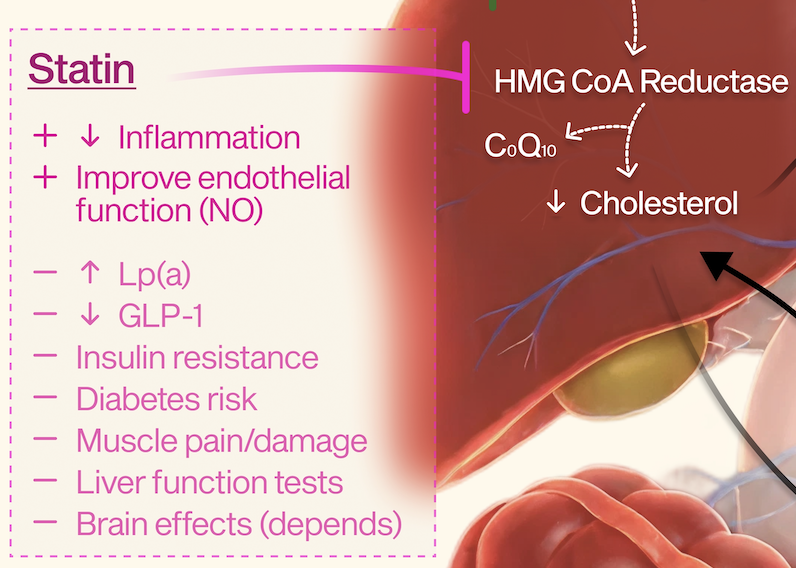 2/6) Lp(a) and Drug Effects
2/6) Lp(a) and Drug Effects

 2/11) There are several mechanisms through which it can support muscle growth (a.k.a. hypertrophy):
2/11) There are several mechanisms through which it can support muscle growth (a.k.a. hypertrophy):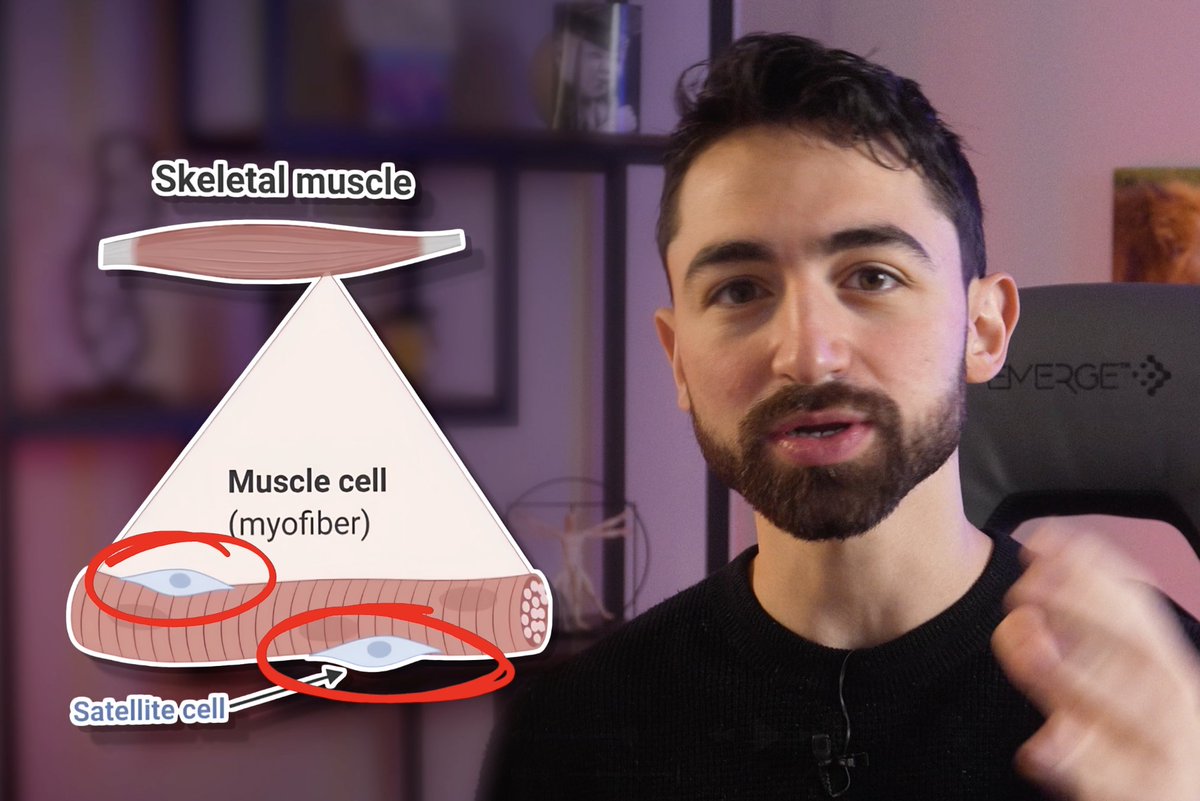
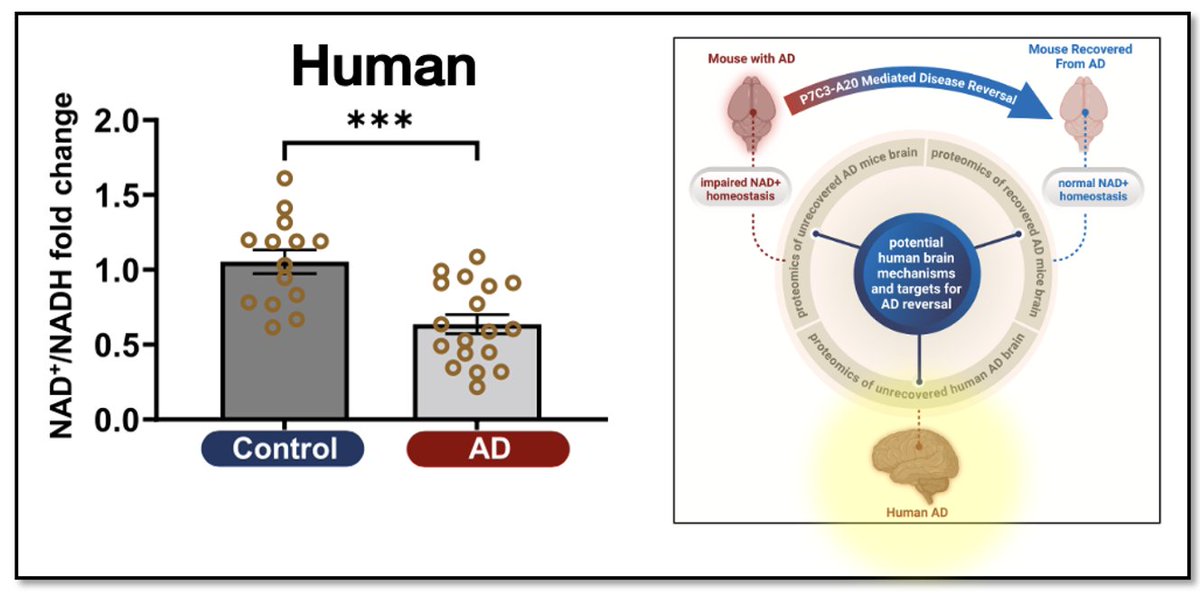
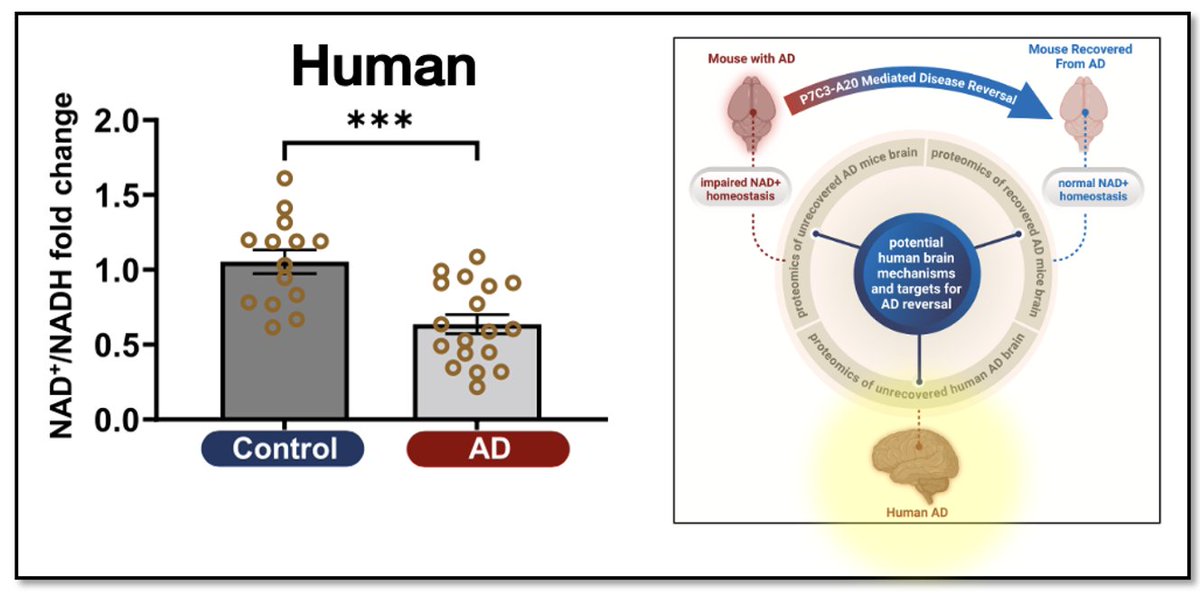 2/9) What is NAD+? NAD+ is an essential energy carrying molecule in the brain.
2/9) What is NAD+? NAD+ is an essential energy carrying molecule in the brain. 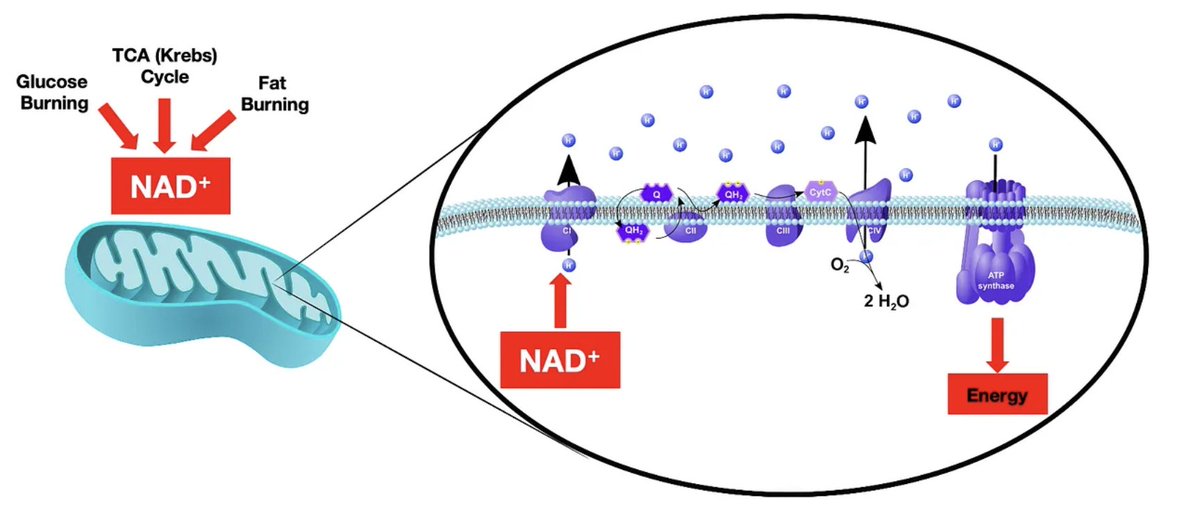


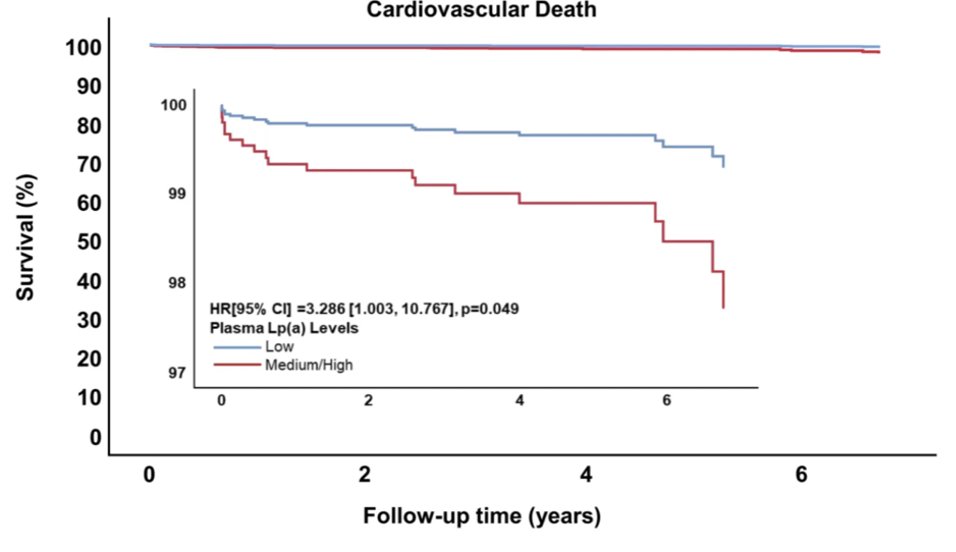
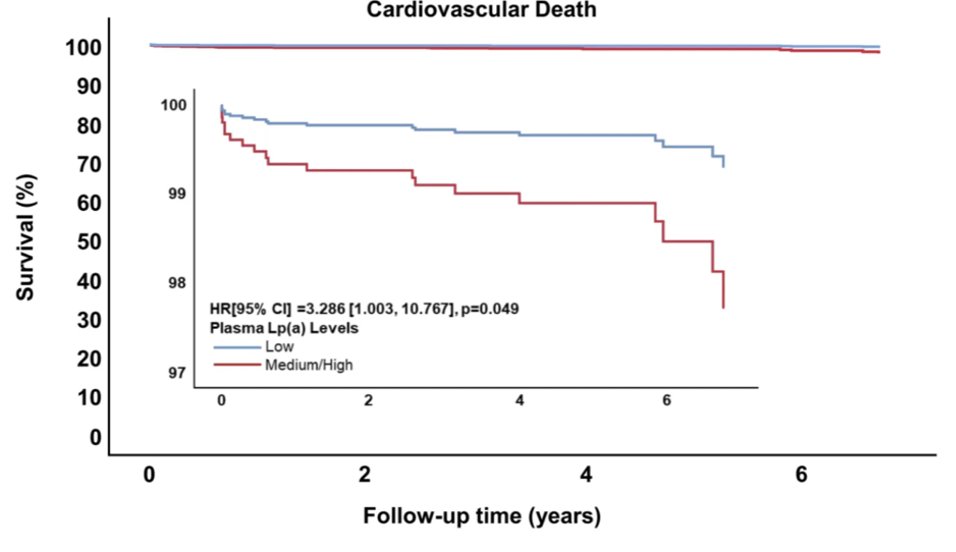
 2/9) The researchers studied 1,027 patients with advanced coronary artery disease who were undergoing cardiac surgery.
2/9) The researchers studied 1,027 patients with advanced coronary artery disease who were undergoing cardiac surgery.

 2/6) To be fair, this was modestly lower than the overall prevalence in the cohort (49%).
2/6) To be fair, this was modestly lower than the overall prevalence in the cohort (49%).
 2/6) Let’s start with some human data.
2/6) Let’s start with some human data.

 2/5) To explore this, researchers analyzed data from 4,652 participants in the Multi-Ethnic Study of Atherosclerosis (MESA), following them over a median of 17.4 years.
2/5) To explore this, researchers analyzed data from 4,652 participants in the Multi-Ethnic Study of Atherosclerosis (MESA), following them over a median of 17.4 years. 

 2/6) We’ll break this up by discussing the cross-sectional (single time point) and longitudinal (over time) results.
2/6) We’ll break this up by discussing the cross-sectional (single time point) and longitudinal (over time) results.