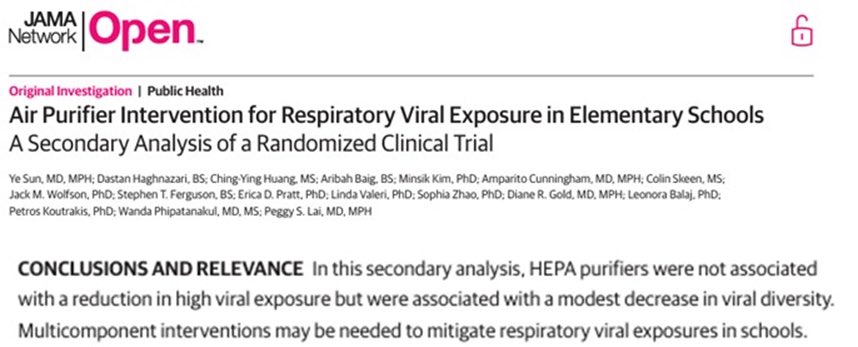
Another junk RCT came out
This time claiming "air purifiers don't reduce exposure to viruses in classrooms"
BOLLOCKS
This time claiming "air purifiers don't reduce exposure to viruses in classrooms"
BOLLOCKS
1st clue this was going to be a junk study: they did an RCT
Wrong tool
There is no equipoise, no unknown or barely discernible benefit to weigh against likely harm
Wrong tool
There is no equipoise, no unknown or barely discernible benefit to weigh against likely harm
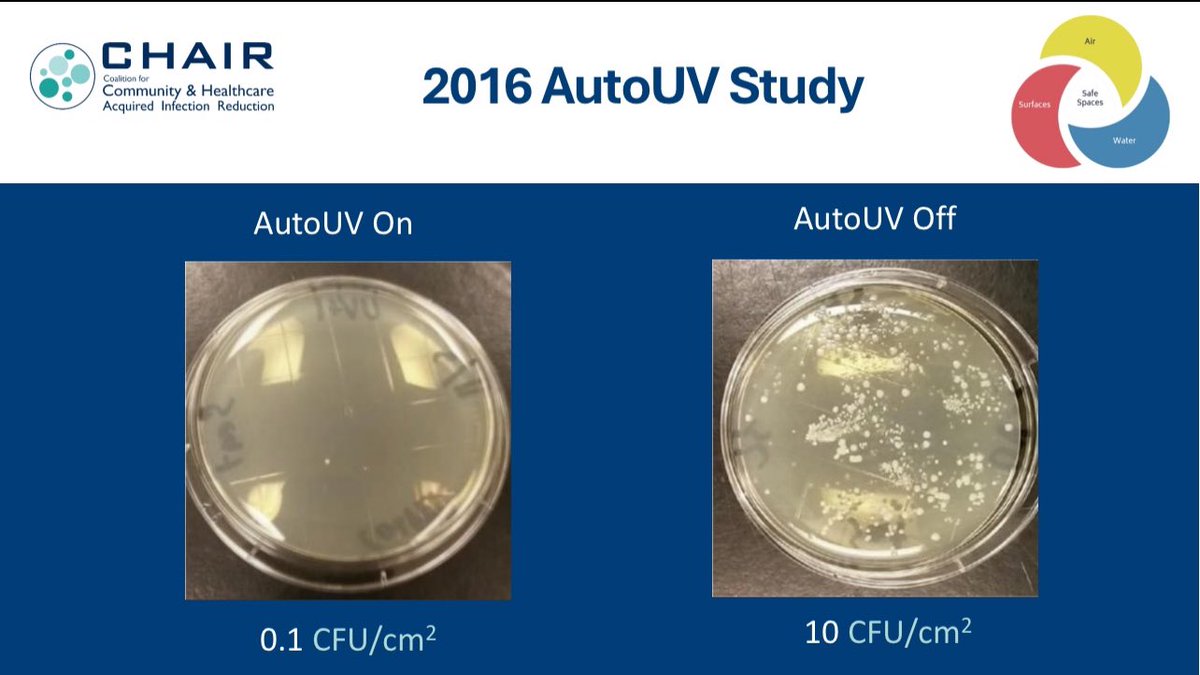
2nd - Many studies already show cause & effect & mathematically quantify the relationship between exposure levels / reduction levels of pathogens in air and infections
An RCT is two steps backwards at this point
And could be considered unethical
An RCT is two steps backwards at this point
And could be considered unethical
3rd - the conclusion is not supported by the data
Not even close
"The HEPA purifier intervention was not associated with lower odds of high viral exposure (odds ratio [OR], 0.50; 95% CI, 0.08-3.25; P = .46)"
What's wrong with this statement?
Let me tell you
Not even close
"The HEPA purifier intervention was not associated with lower odds of high viral exposure (odds ratio [OR], 0.50; 95% CI, 0.08-3.25; P = .46)"
What's wrong with this statement?
Let me tell you
An odds ratio of 0.50 means the intervention WAS ASSOCIATED with a 50% reduction
Pretty good, eh?
Except the range of 0.08 to 3.25 is bonkers
And a p value of .46 is garbage
It means the experiment was junk
The conclusion should have been, "we did something wrong"
Pretty good, eh?
Except the range of 0.08 to 3.25 is bonkers
And a p value of .46 is garbage
It means the experiment was junk
The conclusion should have been, "we did something wrong"
4th - There were many things they did wrong, starting with no scale or context or apples-to-apples standardization
Where is the detail showing base ACH and additional eACH provided by air purifiers?
🤷♂️
Where is the detail showing base ACH and additional eACH provided by air purifiers?
🤷♂️
Without that basic information, how do you know your intervention has the effect size it needs?
In this case, how do you know if the air purifiers have the CADR needed to see an effect?
🤷♂️
In this case, how do you know if the air purifiers have the CADR needed to see an effect?
🤷♂️
How do you know if you're meeting basic Standards guiding ventilation for infection prevention?
🤷♂️
🤷♂️
Answer is, you don't. And in this case, the air purifiers were clearly undersized
I don't mean physically, I mean CADR
So much so they put 4 of them into each classroom
They would have needed 12
I don't mean physically, I mean CADR
So much so they put 4 of them into each classroom
They would have needed 12
5th - kids are in classroom 5 days / week x 6h / day = 30 hours but the measurements were taken after one week of sampling = 24h / day x 7 days / week = 168 hours
30h / 168h = 18% of the time viruses are shed into the air
30h / 168h = 18% of the time viruses are shed into the air
So you're looking for a result while ignoring the fact that 82% of the time the air purifiers are just cleaning clean air
Ignoring the fact that there is a mismatch between shedding & sampling
Ignoring that whatever the result is, it's diluted 5-fold
Ignoring the fact that there is a mismatch between shedding & sampling
Ignoring that whatever the result is, it's diluted 5-fold
The units chosen were expensive, undersized, the application was impractical & not scalable, there was no reference to existing Standards, they used the wrong experimental tool, ignored fallow time, came to the wrong conclusion, & published inflammatory disinformation in a prestigious journal
I give it an F
We have to stop funding junk science with taxpayer dollars
We have to stop publishing junk science in prestigious journals
Or stop calling them prestigious journals
We have to stop junk science being weaponized to block real-world interventions that work to protect the public
We have to stop publishing junk science in prestigious journals
Or stop calling them prestigious journals
We have to stop junk science being weaponized to block real-world interventions that work to protect the public
Al Haddrell .@ukhadds has more to say on the matter
https://twitter.com/ukhadds/status/1977990481591078984
• • •
Missing some Tweet in this thread? You can try to
force a refresh