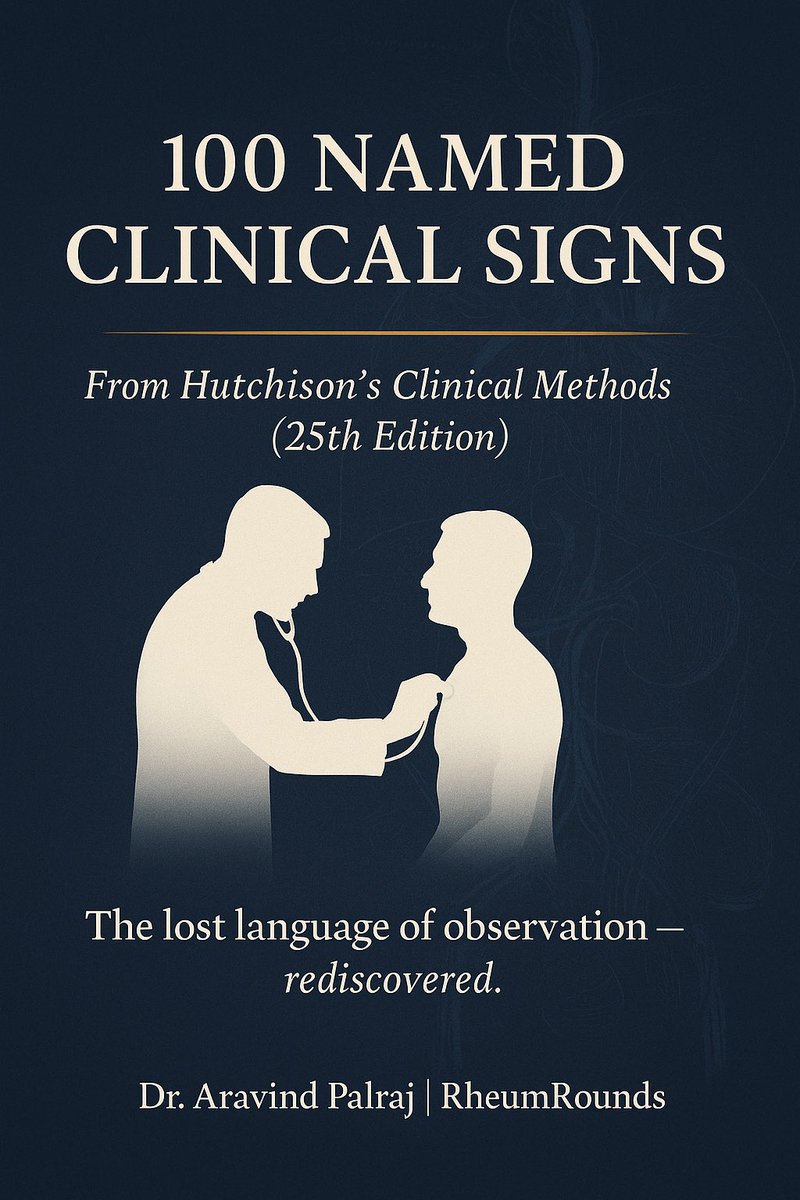
🧵100 timeless bedside gems every doctor should know.
Straight from Hutchison’s Clinical Methods — distilled into 10 clean infographics.
If you love real clinical medicine, this thread will remind you why you chose it.
🩺 Let’s bring back the art of examination 👇
(Save this thread — it’ll outlive most AI tools.) #MedTwitter #MedEd #FOAMed @DrAkhilX @IhabFathiSulima @drkeithsiau @DurgaPrasannaM1 @JasmineNephro
Straight from Hutchison’s Clinical Methods — distilled into 10 clean infographics.
If you love real clinical medicine, this thread will remind you why you chose it.
🩺 Let’s bring back the art of examination 👇
(Save this thread — it’ll outlive most AI tools.) #MedTwitter #MedEd #FOAMed @DrAkhilX @IhabFathiSulima @drkeithsiau @DurgaPrasannaM1 @JasmineNephro
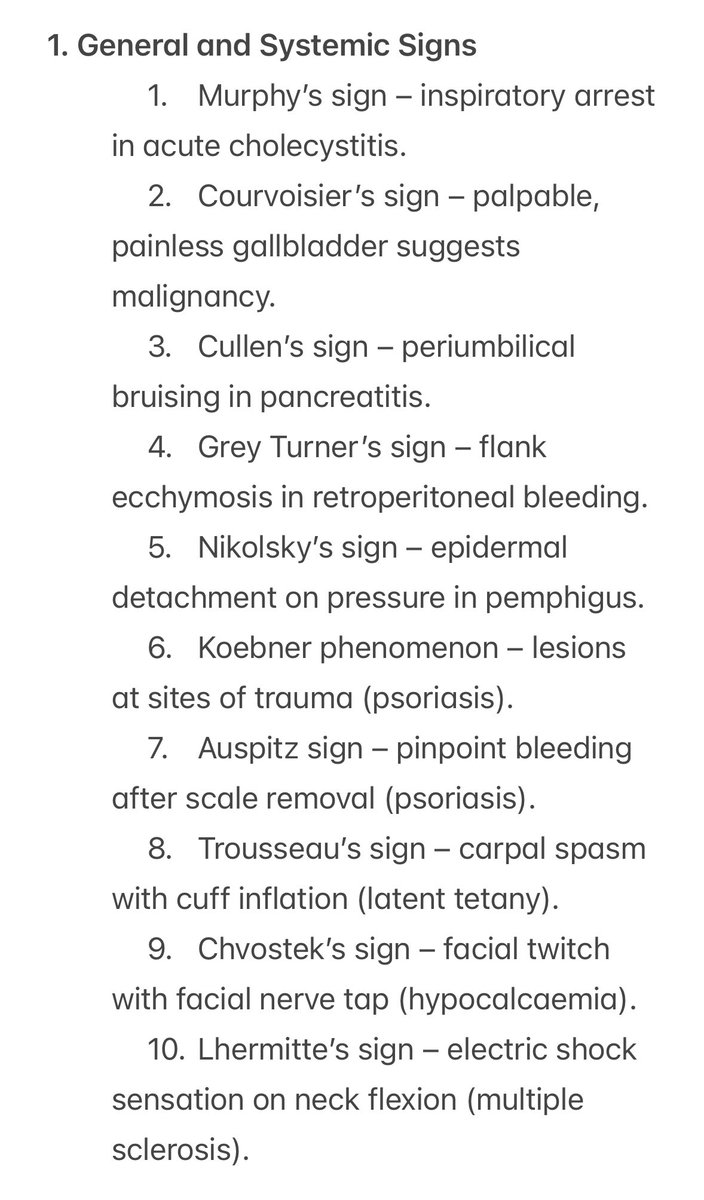
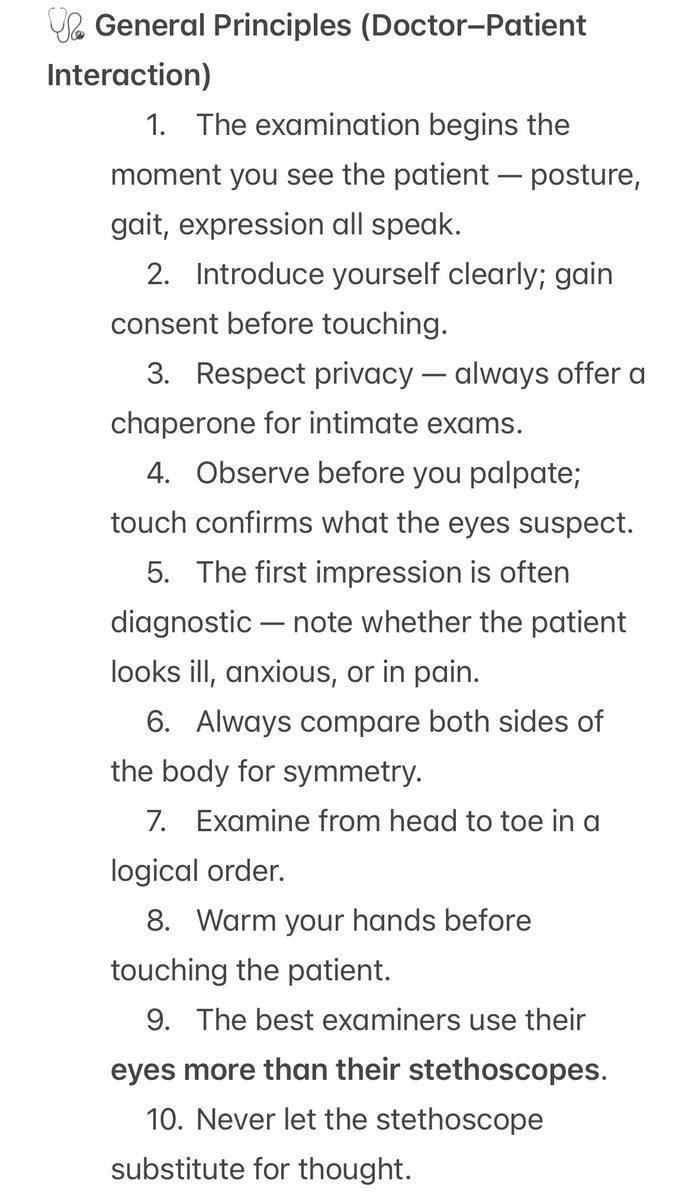
General Principles
1️⃣ The patient will tell you the diagnosis — if you learn to listen.
History first. Examination next. Investigations last.
🩺 The foundation Hutchison built 125 years ago still holds true.
1️⃣ The patient will tell you the diagnosis — if you learn to listen.
History first. Examination next. Investigations last.
🩺 The foundation Hutchison built 125 years ago still holds true.
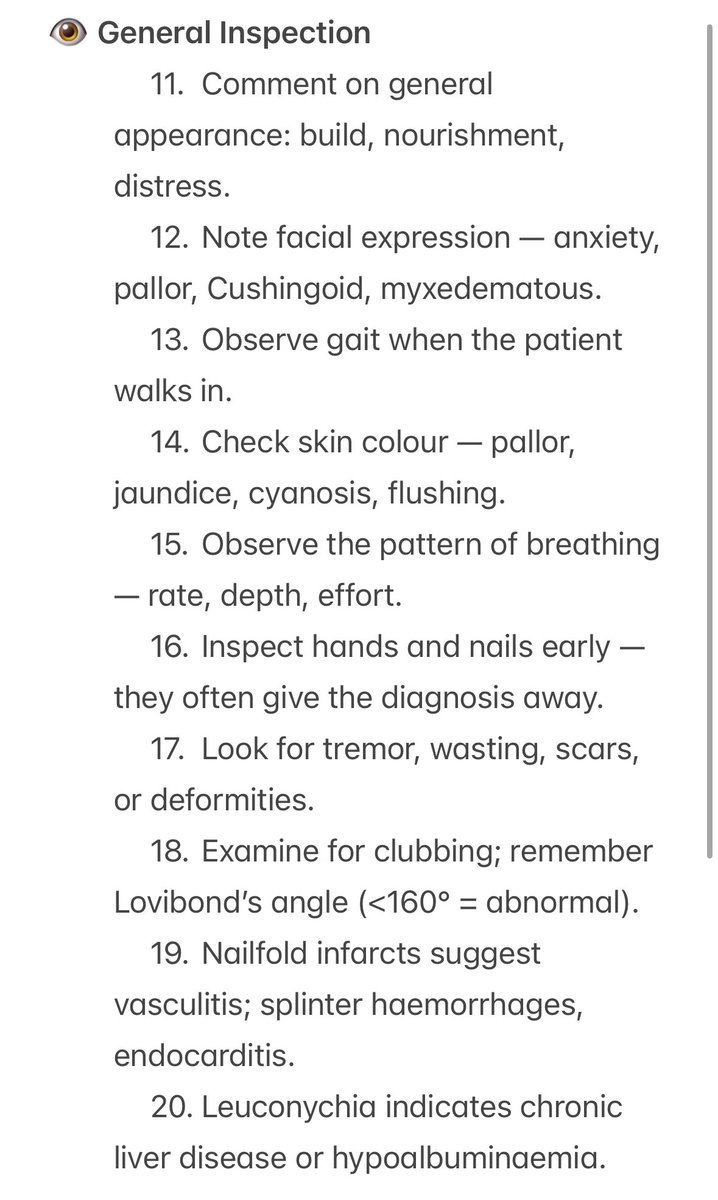
General Inspection
2️⃣ The first 10 seconds matter.
How they walk, talk, sit, breathe — that’s your first set of vitals.
The best clinicians diagnose before touching the patient.
2️⃣ The first 10 seconds matter.
How they walk, talk, sit, breathe — that’s your first set of vitals.
The best clinicians diagnose before touching the patient.
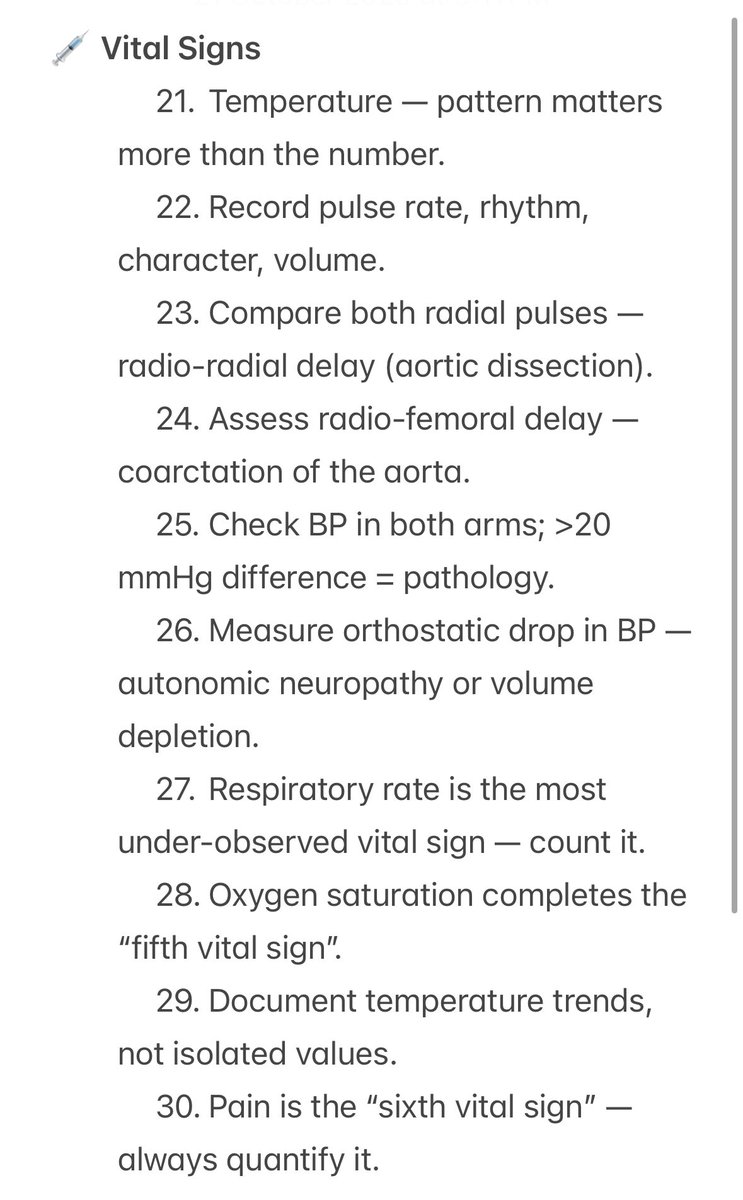
Vital Signs
3️⃣ “Count the pulse. Count the respirations. Feel the temperature.”
The basics we rush through are often the ones that save lives.
#ClinicalSkills
3️⃣ “Count the pulse. Count the respirations. Feel the temperature.”
The basics we rush through are often the ones that save lives.
#ClinicalSkills
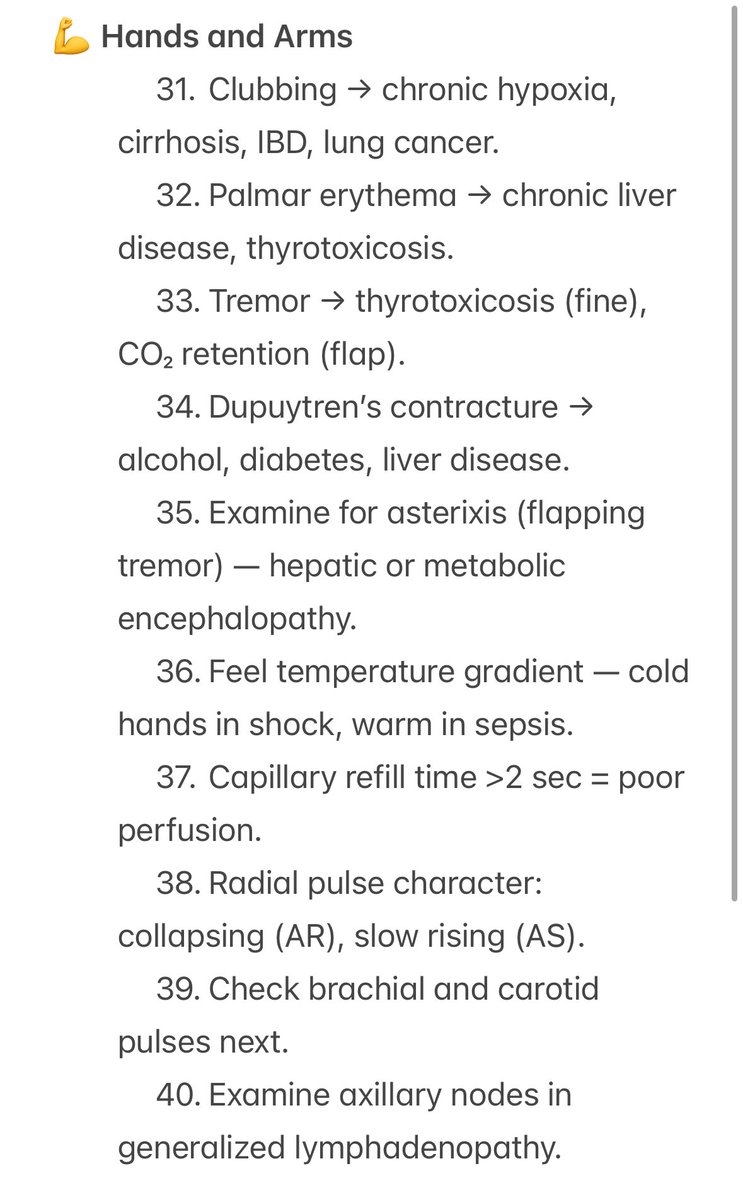
Hands and Arms
4️⃣ The hands are a diagnostic atlas.
Clubbing, tremor, palmar erythema, koilonychia — every sign tells a story.
👋 Start there.
4️⃣ The hands are a diagnostic atlas.
Clubbing, tremor, palmar erythema, koilonychia — every sign tells a story.
👋 Start there.
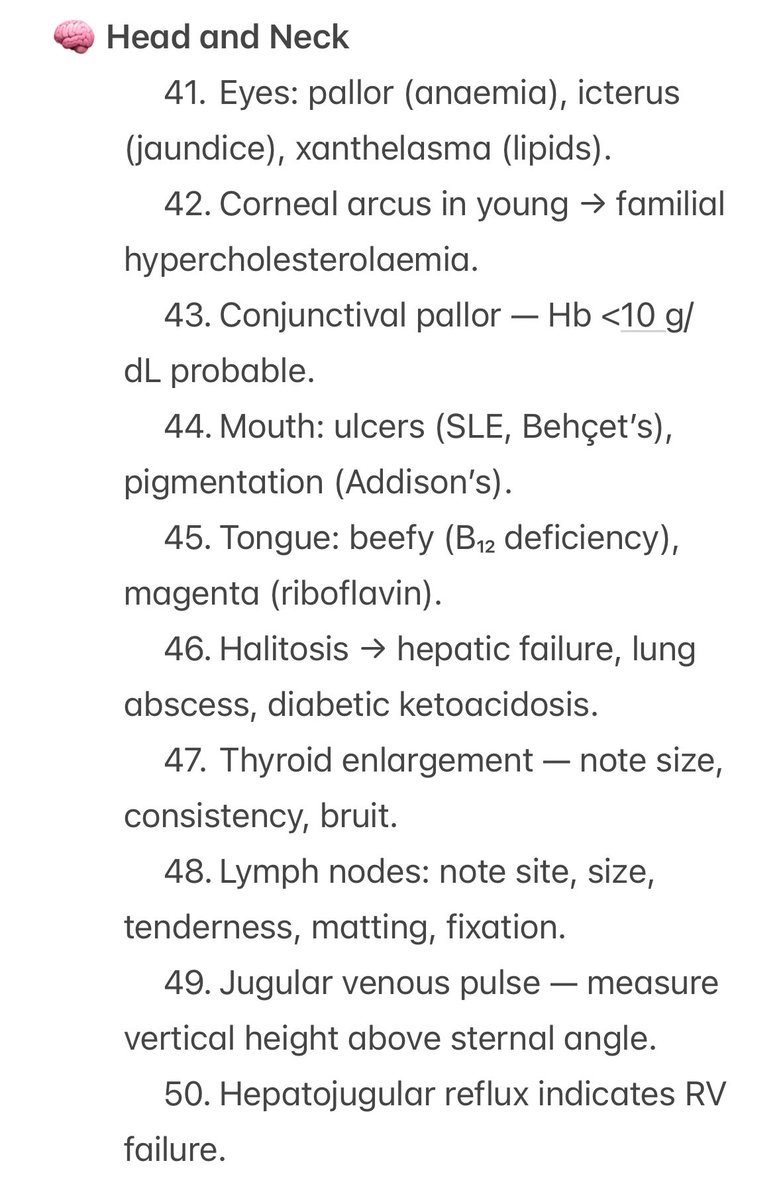
Head and Neck
5️⃣ The face is a mirror of disease.
Addison’s bronze, Cushing’s moon, thyrotoxicosis stare, myxoedematous puffiness —
the entire endocrine chapter is right there.
5️⃣ The face is a mirror of disease.
Addison’s bronze, Cushing’s moon, thyrotoxicosis stare, myxoedematous puffiness —
the entire endocrine chapter is right there.
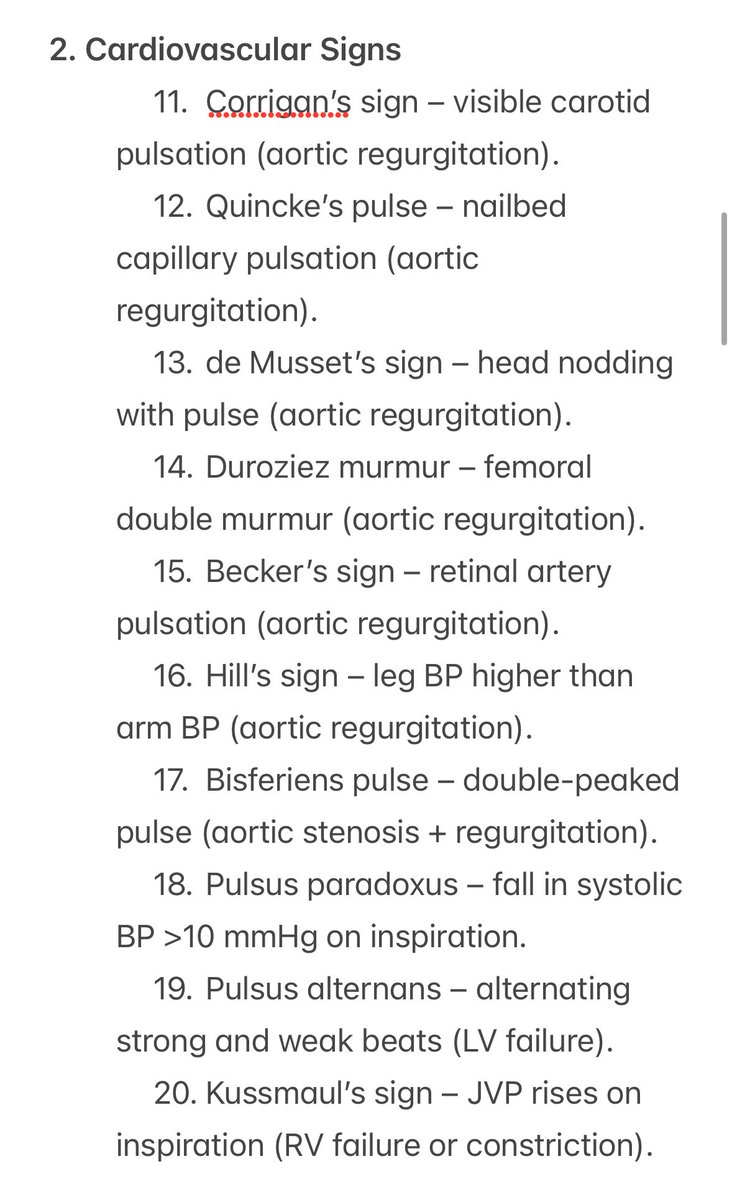
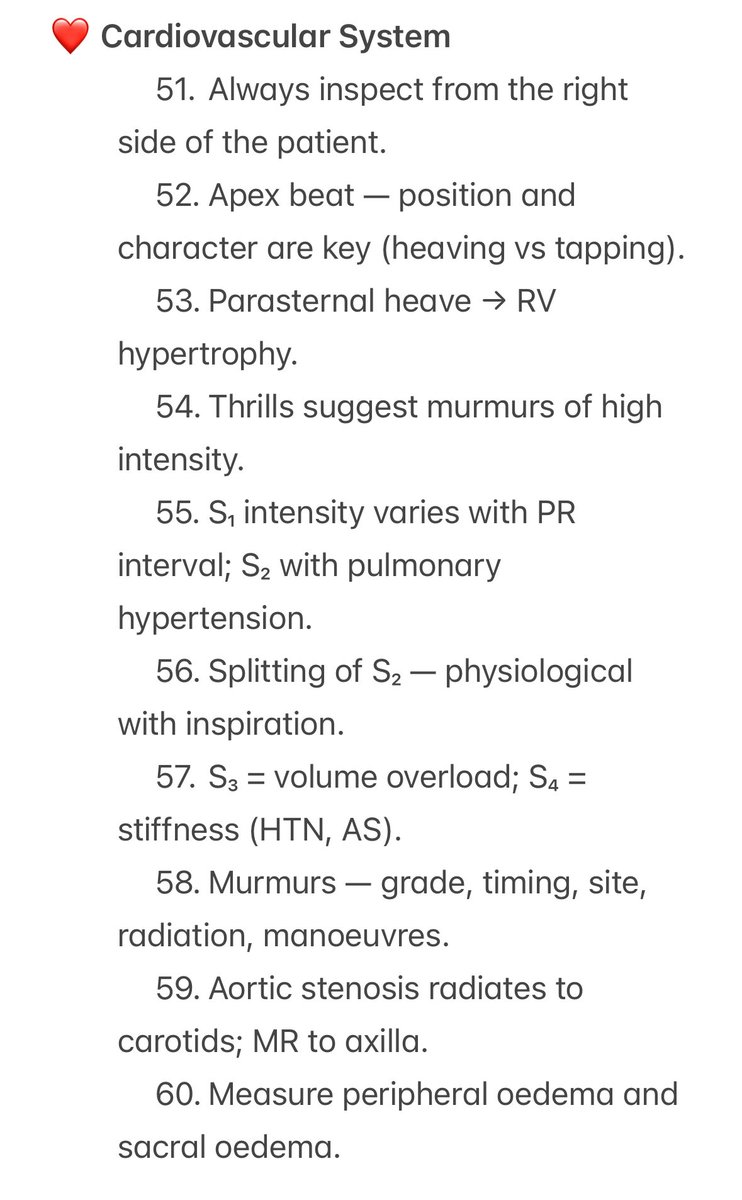
Cardiovascular
6️⃣ Before the ECG, there was the pulse.
Before the echo, there was the stethoscope.
Hutchison reminds us: the rhythm of the heart begins in the fingertips.
6️⃣ Before the ECG, there was the pulse.
Before the echo, there was the stethoscope.
Hutchison reminds us: the rhythm of the heart begins in the fingertips.
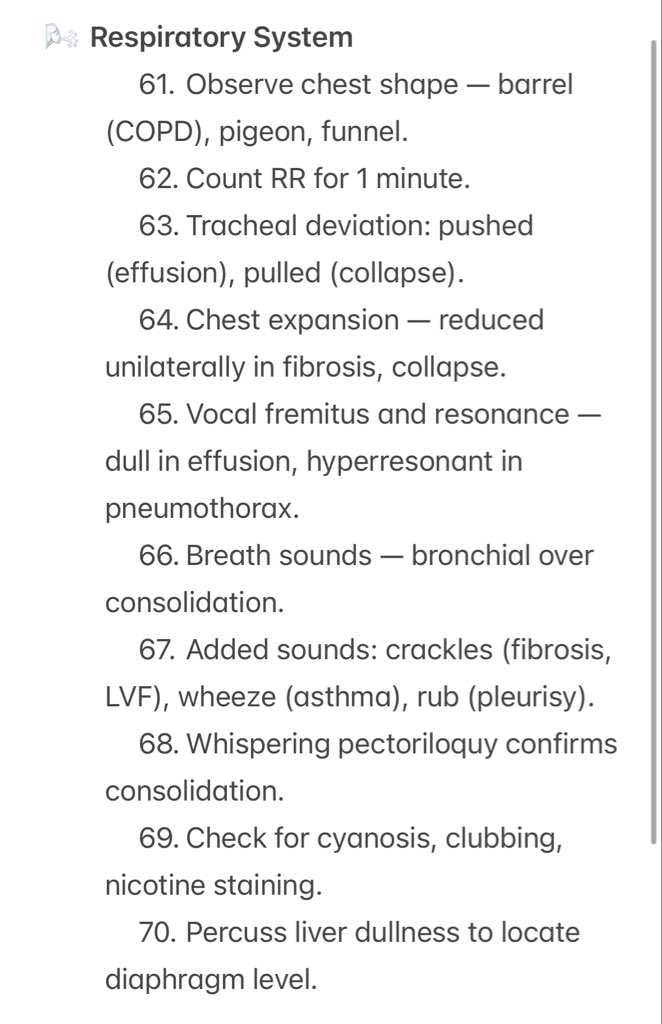
Respiratory
7️⃣ The percussion note tells the truth before the CT does.
Hyperresonant, dull, stony — the chest speaks if you know the language.
🌬️ #MedTwitter
7️⃣ The percussion note tells the truth before the CT does.
Hyperresonant, dull, stony — the chest speaks if you know the language.
🌬️ #MedTwitter
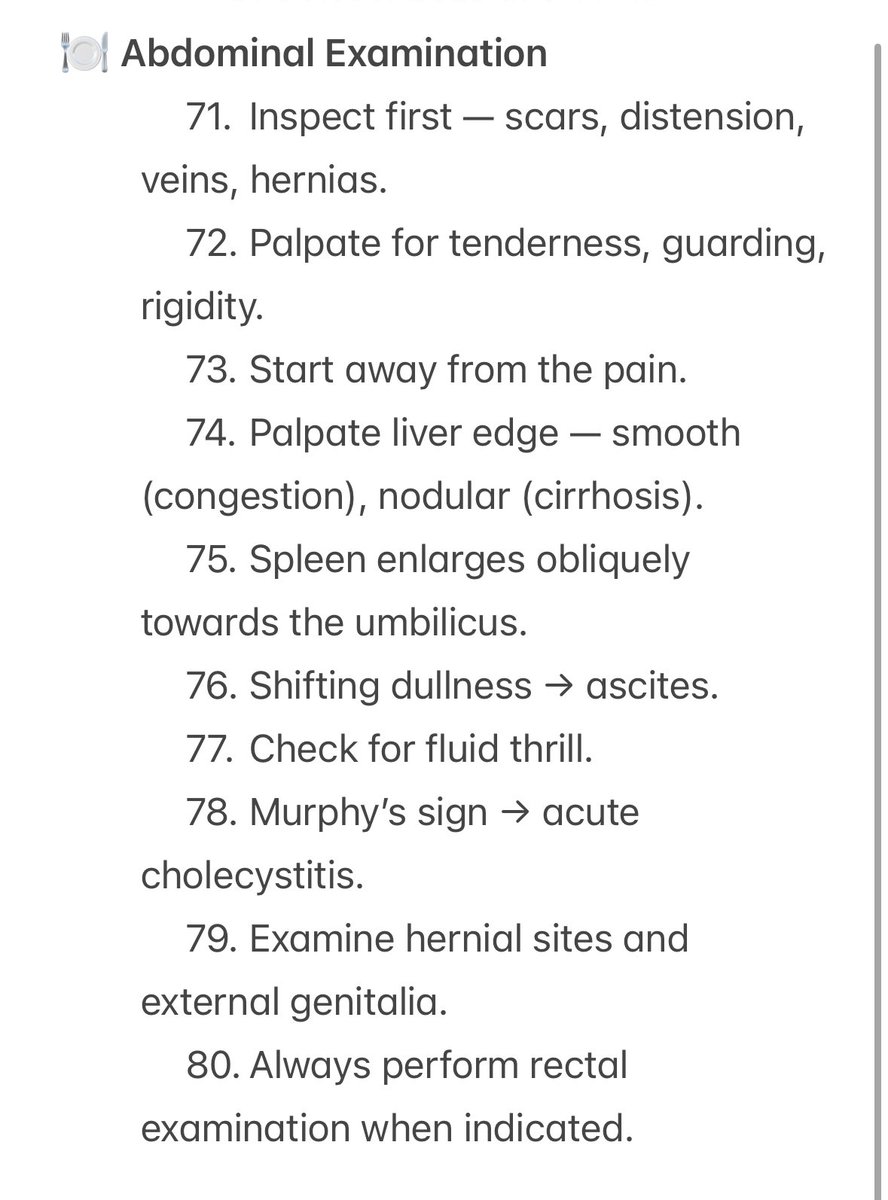
Abdominal
8️⃣ Inspection. Palpation. Percussion. Auscultation.
The four words that built internal medicine.
🩺 Each quadrant tells a story — you just have to listen.
8️⃣ Inspection. Palpation. Percussion. Auscultation.
The four words that built internal medicine.
🩺 Each quadrant tells a story — you just have to listen.
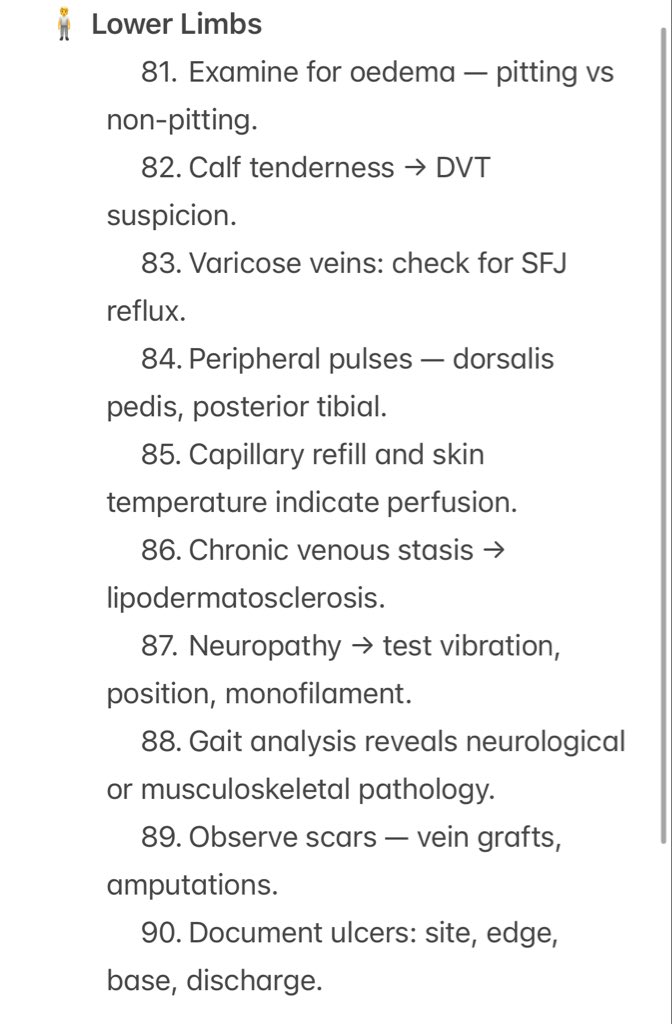
Lower Limbs
🦵 Lower limbs: don’t skip them.
Check pulses, temperature, capillary refill, calf tenderness (DVT), varicose changes, and neuropathic loss.
Small findings in the legs often explain big system problems — vascular, neuro, or metabolic.
🦵 Lower limbs: don’t skip them.
Check pulses, temperature, capillary refill, calf tenderness (DVT), varicose changes, and neuropathic loss.
Small findings in the legs often explain big system problems — vascular, neuro, or metabolic.
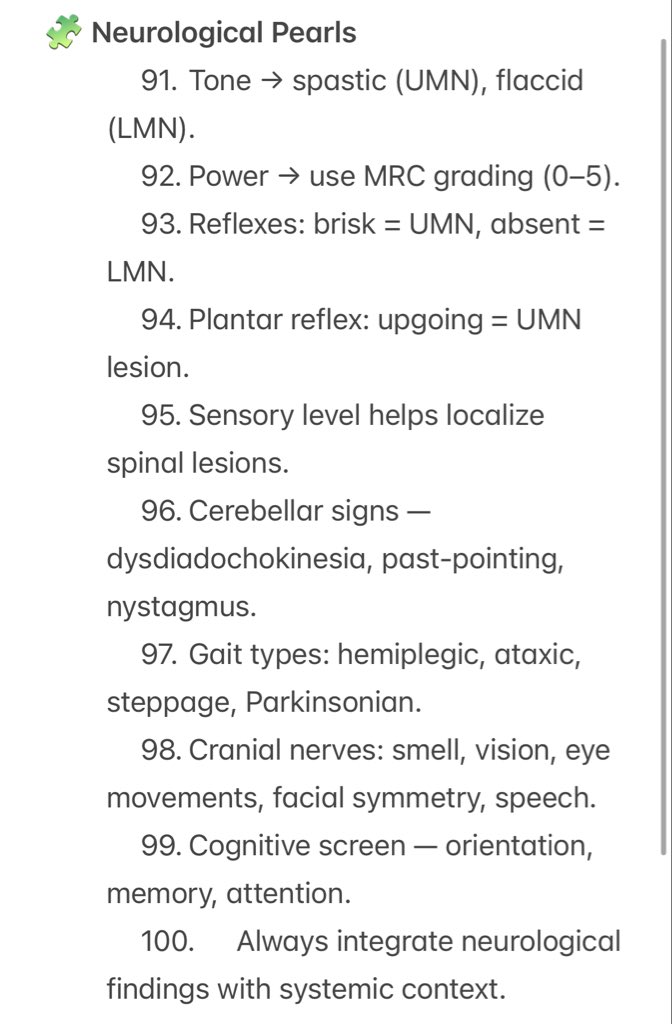
Neurology
1️⃣0️⃣ Examine the nervous system like poetry, not like code.
Tone, power, reflexes, coordination — rhythm and balance.
Hutchison called it “the art of pattern recognition.”
1️⃣0️⃣ Examine the nervous system like poetry, not like code.
Tone, power, reflexes, coordination — rhythm and balance.
Hutchison called it “the art of pattern recognition.”
Closing / Summary
💯 100 Gems. 10 Infographics. 1 timeless lesson.
Machines may assist.
But bedside medicine will always belong to the human mind.
🩺 Keep learning. Keep examining. Keep observing.
— Dr. Aravind Palraj | #RheumRounds
💯 100 Gems. 10 Infographics. 1 timeless lesson.
Machines may assist.
But bedside medicine will always belong to the human mind.
🩺 Keep learning. Keep examining. Keep observing.
— Dr. Aravind Palraj | #RheumRounds
• • •
Missing some Tweet in this thread? You can try to
force a refresh