🧵“100 Named Clinical Signs — Hutchison’s Clinical Methods (25th Edition)”
AI detects patterns.
Hutchison detected patients.
Here are 100 named clinical signs that still shape bedside diagnosis —
signs that live in the wards, not in the algorithms.
The lost language of observation begins below 👇
@DrAkhilX @IhabFathiSulima @drkeithsiau @ArunInamadar @nirmalregency #MedTwitter
AI detects patterns.
Hutchison detected patients.
Here are 100 named clinical signs that still shape bedside diagnosis —
signs that live in the wards, not in the algorithms.
The lost language of observation begins below 👇
@DrAkhilX @IhabFathiSulima @drkeithsiau @ArunInamadar @nirmalregency #MedTwitter
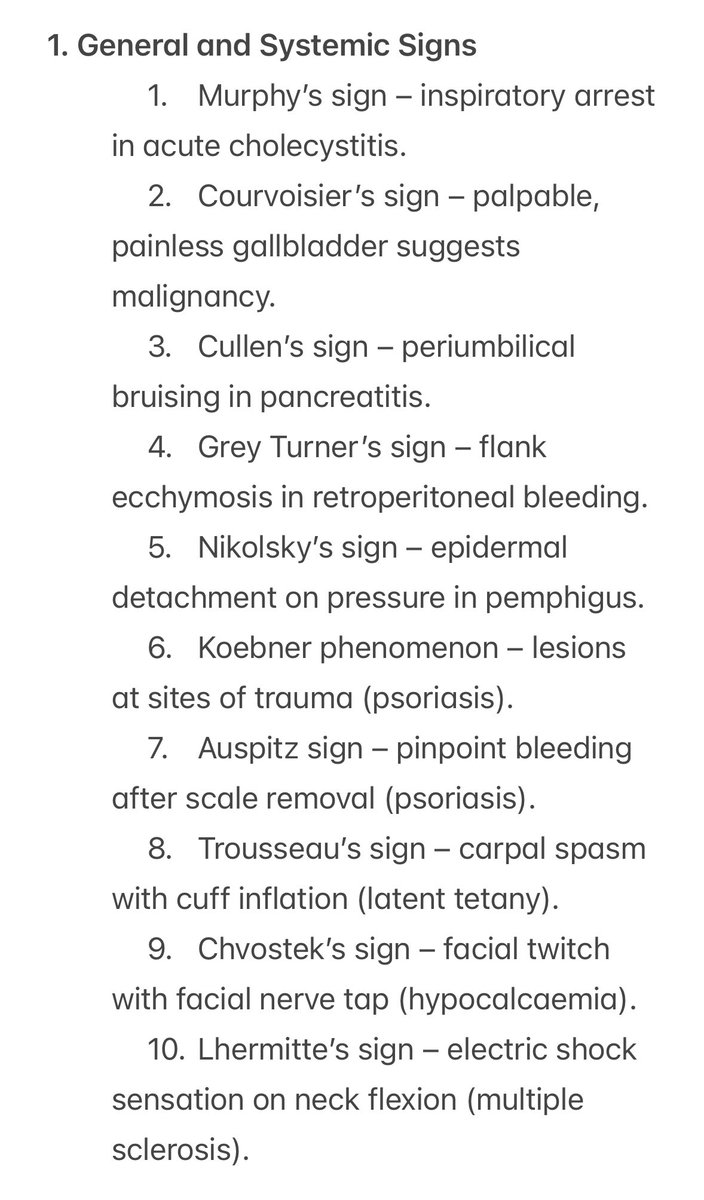
General and Systemic Signs
1️⃣ The body speaks before the lab does.
From Murphy’s to Nikolsky’s — every sign here was discovered by listening to the patient, not the monitor.
The skin, breath, and reflex still tell the truth first.
1️⃣ The body speaks before the lab does.
From Murphy’s to Nikolsky’s — every sign here was discovered by listening to the patient, not the monitor.
The skin, breath, and reflex still tell the truth first.
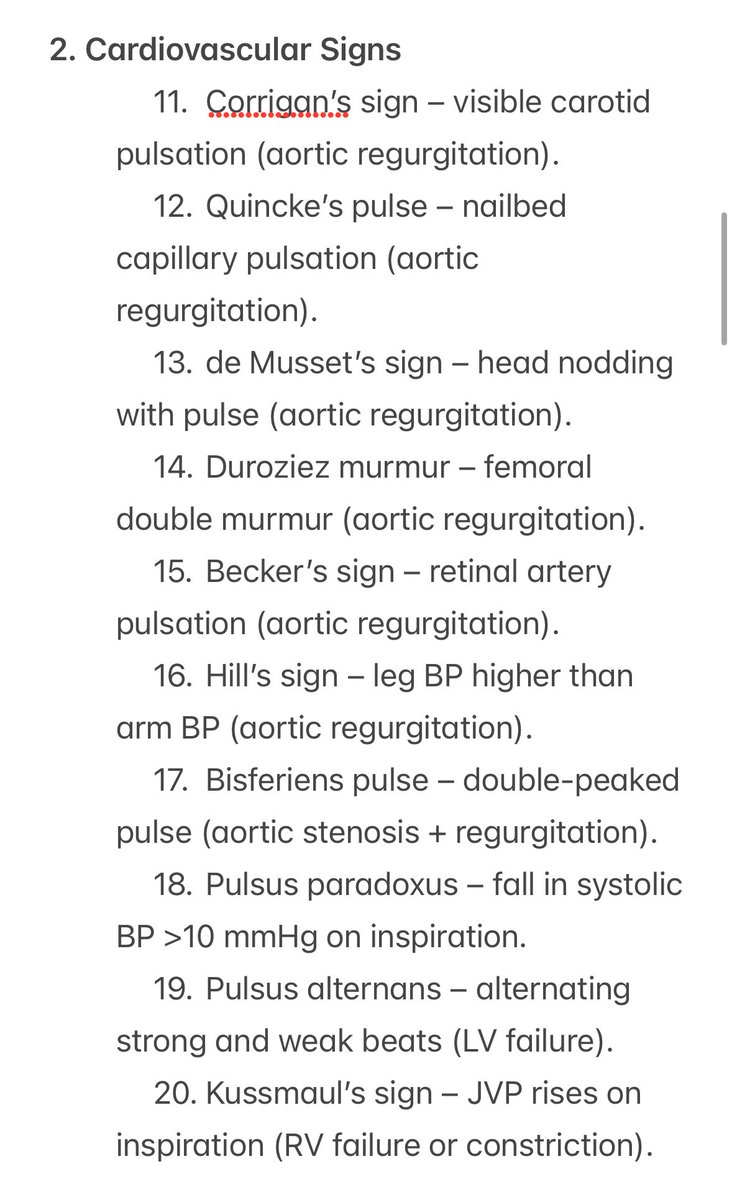
Cardiovascular Signs
2️⃣ The pulse has poetry.
Corrigan, Quincke, de Musset — names that still echo with each beat.
You don’t need an echo when your fingers already know.
2️⃣ The pulse has poetry.
Corrigan, Quincke, de Musset — names that still echo with each beat.
You don’t need an echo when your fingers already know.
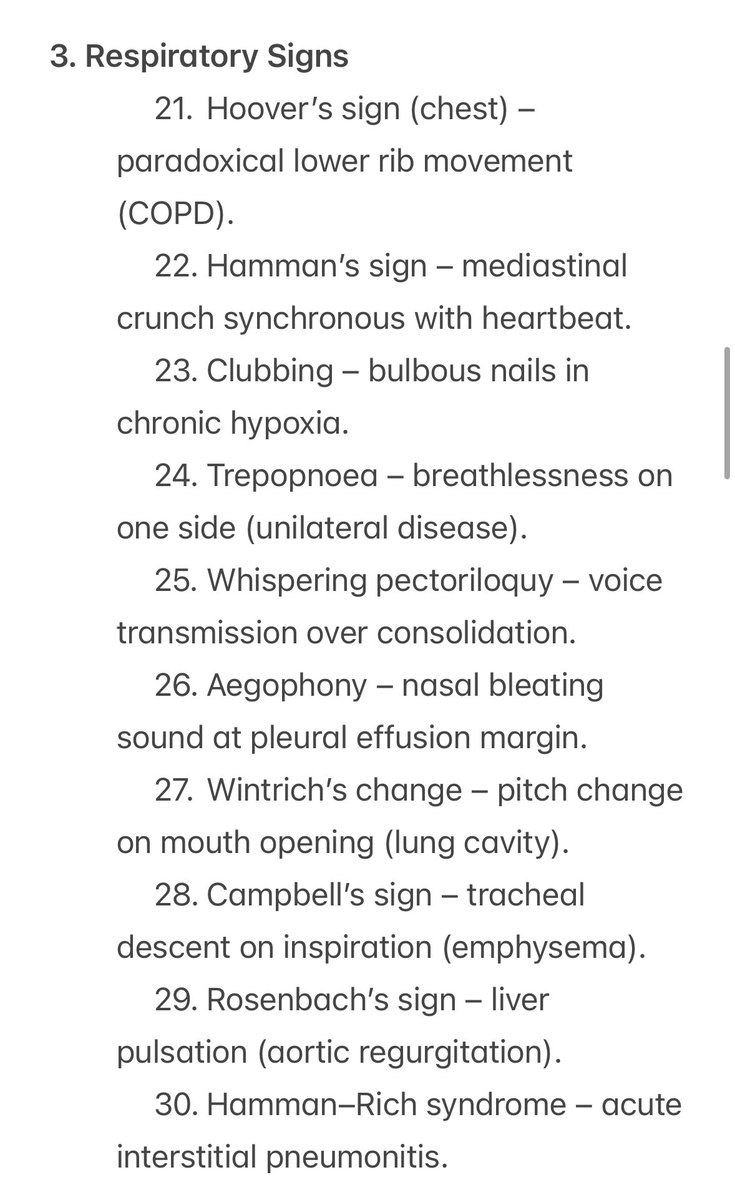
Respiratory Signs
3️⃣ The chest is a percussion instrument — and you’re the musician.
Hoover, Hamman, Aegophony, Whispering Pectoriloquy — each note carries a clue.
Hutchison still whispers through the stethoscope.
3️⃣ The chest is a percussion instrument — and you’re the musician.
Hoover, Hamman, Aegophony, Whispering Pectoriloquy — each note carries a clue.
Hutchison still whispers through the stethoscope.
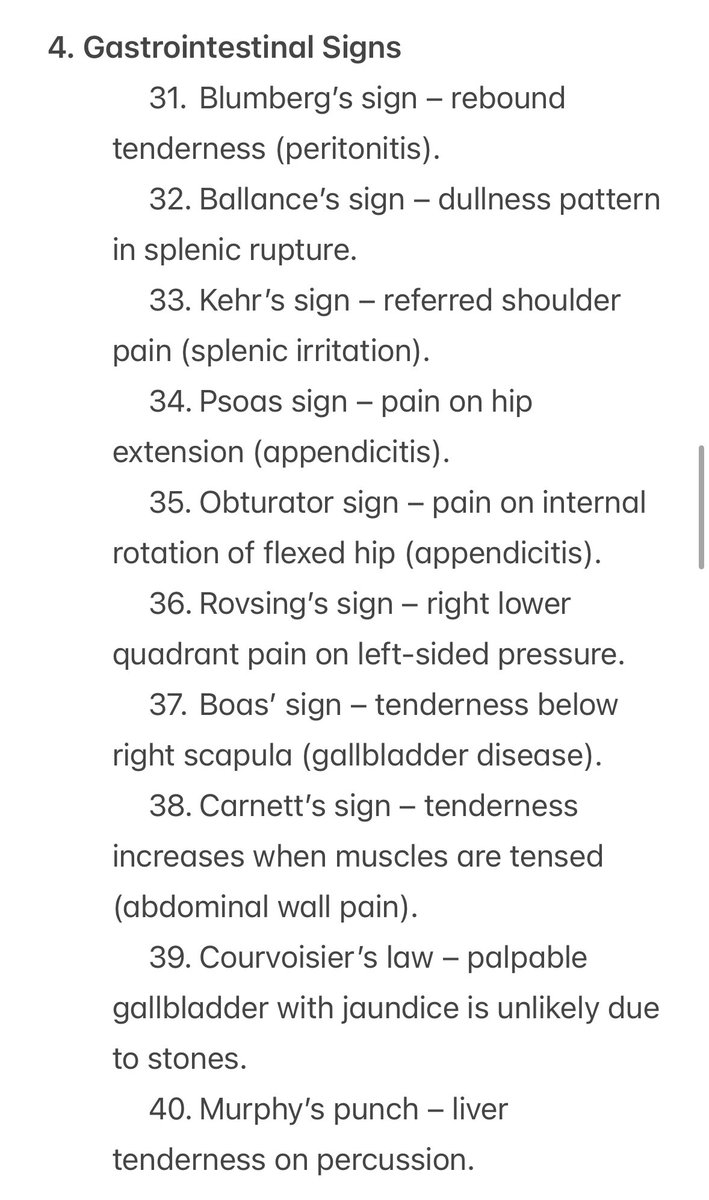
Gastrointestinal Signs
4️⃣ The abdomen hides nothing from patient hands that know where to press.
Murphy, Rovsing, Psoas, Boas — every test a silent conversation with peritoneum and pain.
4️⃣ The abdomen hides nothing from patient hands that know where to press.
Murphy, Rovsing, Psoas, Boas — every test a silent conversation with peritoneum and pain.
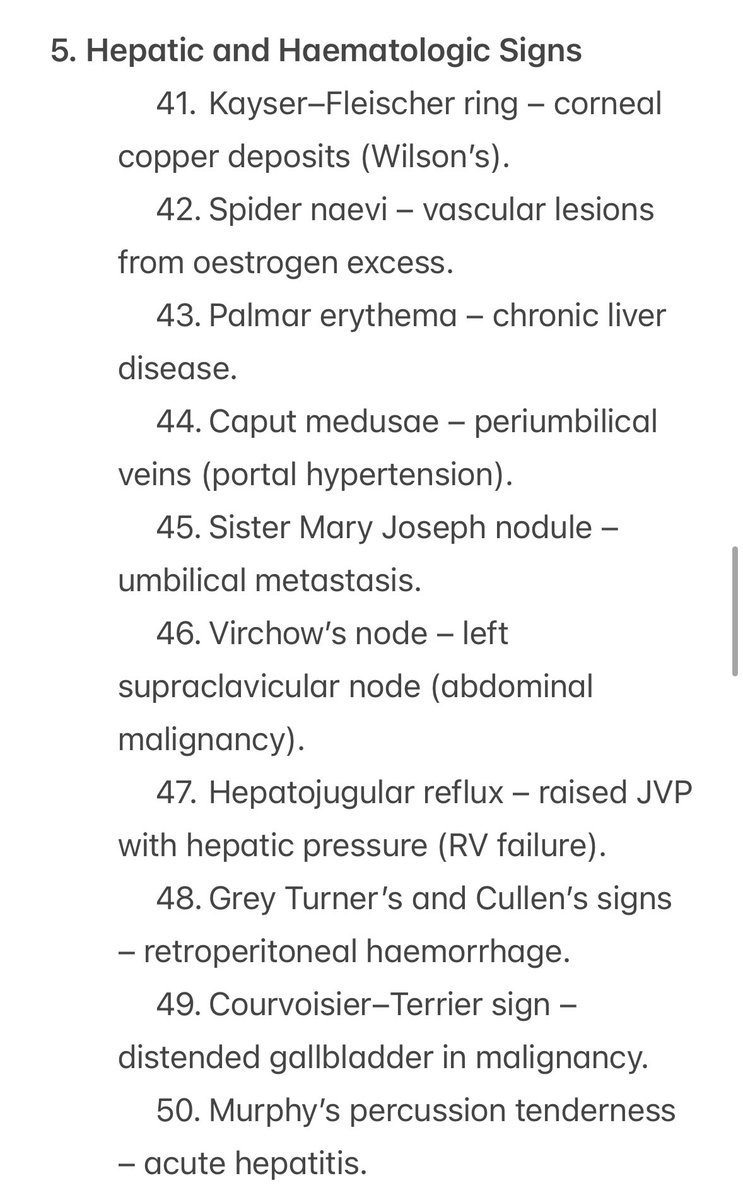
Hepatic and Haematologic Signs
5️⃣ The liver has no secrets from a watchful eye.
From Kayser–Fleischer rings to Sister Mary Joseph’s nodule —
each sign a quiet message from deep disease.
5️⃣ The liver has no secrets from a watchful eye.
From Kayser–Fleischer rings to Sister Mary Joseph’s nodule —
each sign a quiet message from deep disease.
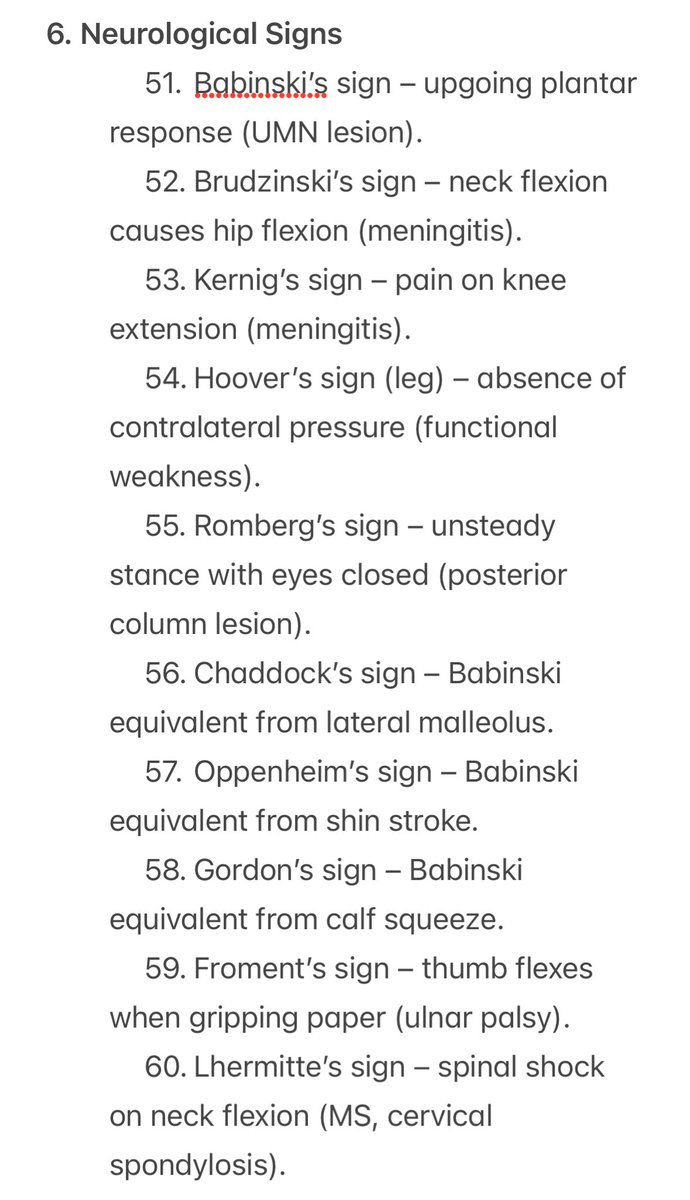
Neurological Signs
6️⃣ The nervous system doesn’t lie — it just hides in reflexes.
Babinski, Brudzinski, Froment — ancient signals of anatomy in action.
Clinical neurology is the original detective work.
6️⃣ The nervous system doesn’t lie — it just hides in reflexes.
Babinski, Brudzinski, Froment — ancient signals of anatomy in action.
Clinical neurology is the original detective work.
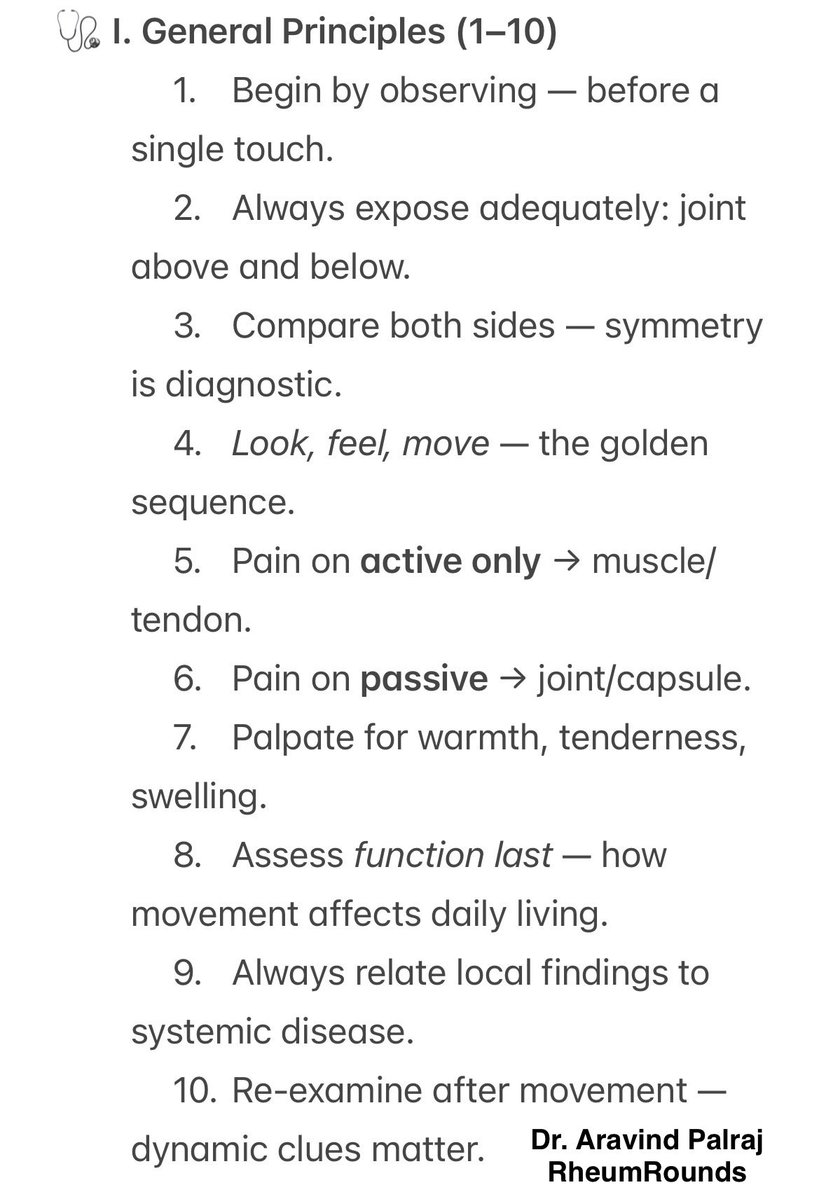
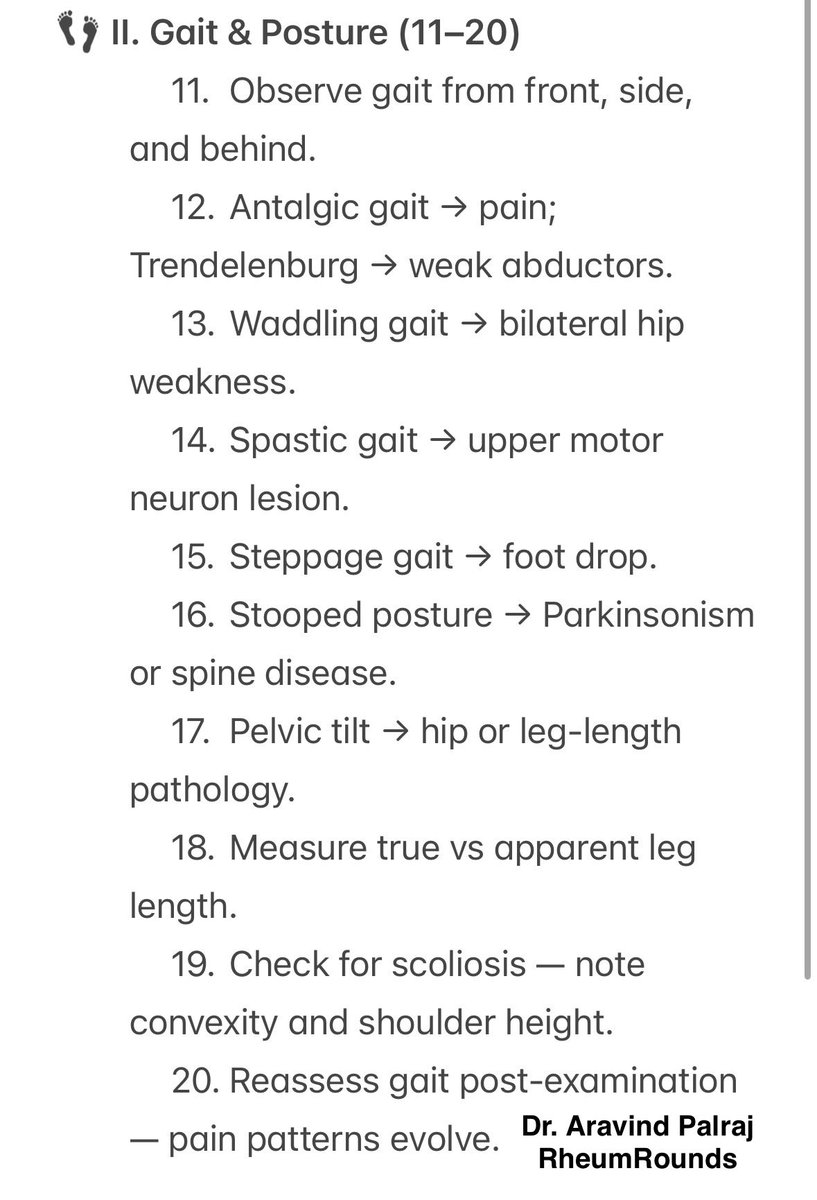
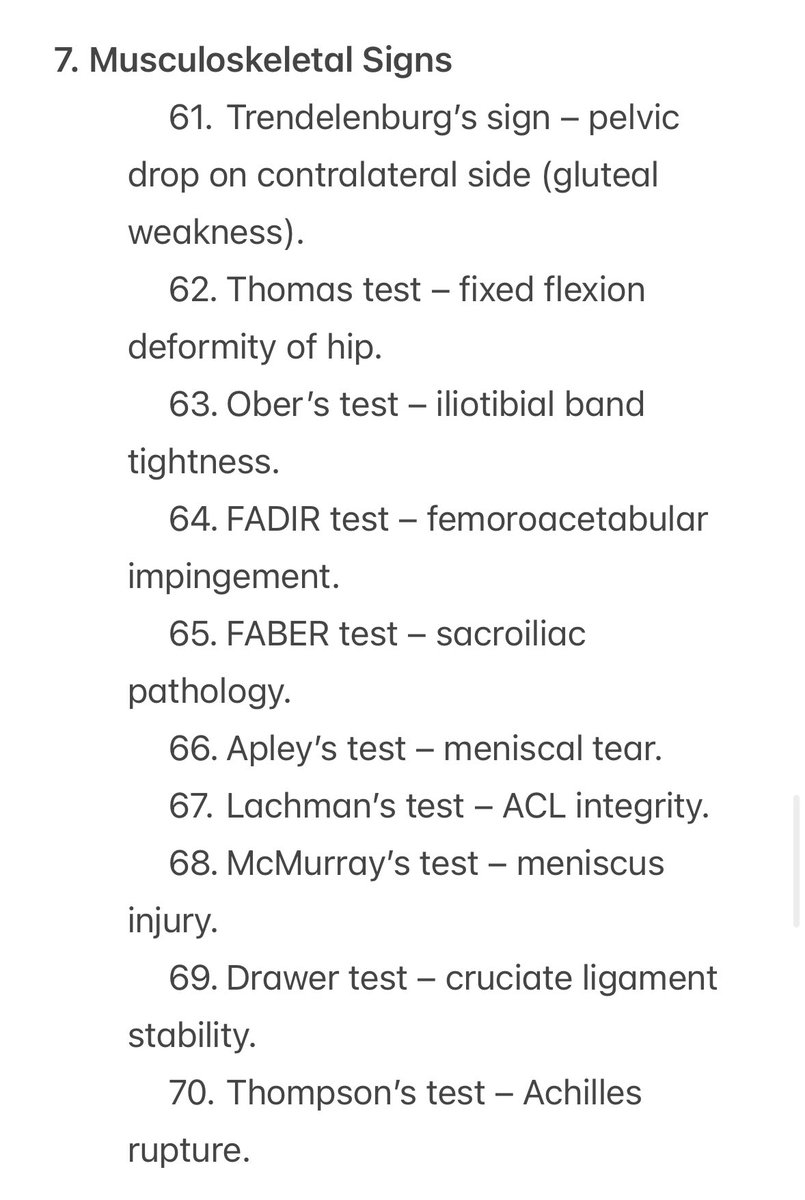
Musculoskeletal Signs
7️⃣ Movement is memory.
Trendelenburg, Thomas, Lachman, McMurray —
each test a choreography between pain, power, and precision.
The body never improvises; it remembers.
7️⃣ Movement is memory.
Trendelenburg, Thomas, Lachman, McMurray —
each test a choreography between pain, power, and precision.
The body never improvises; it remembers.
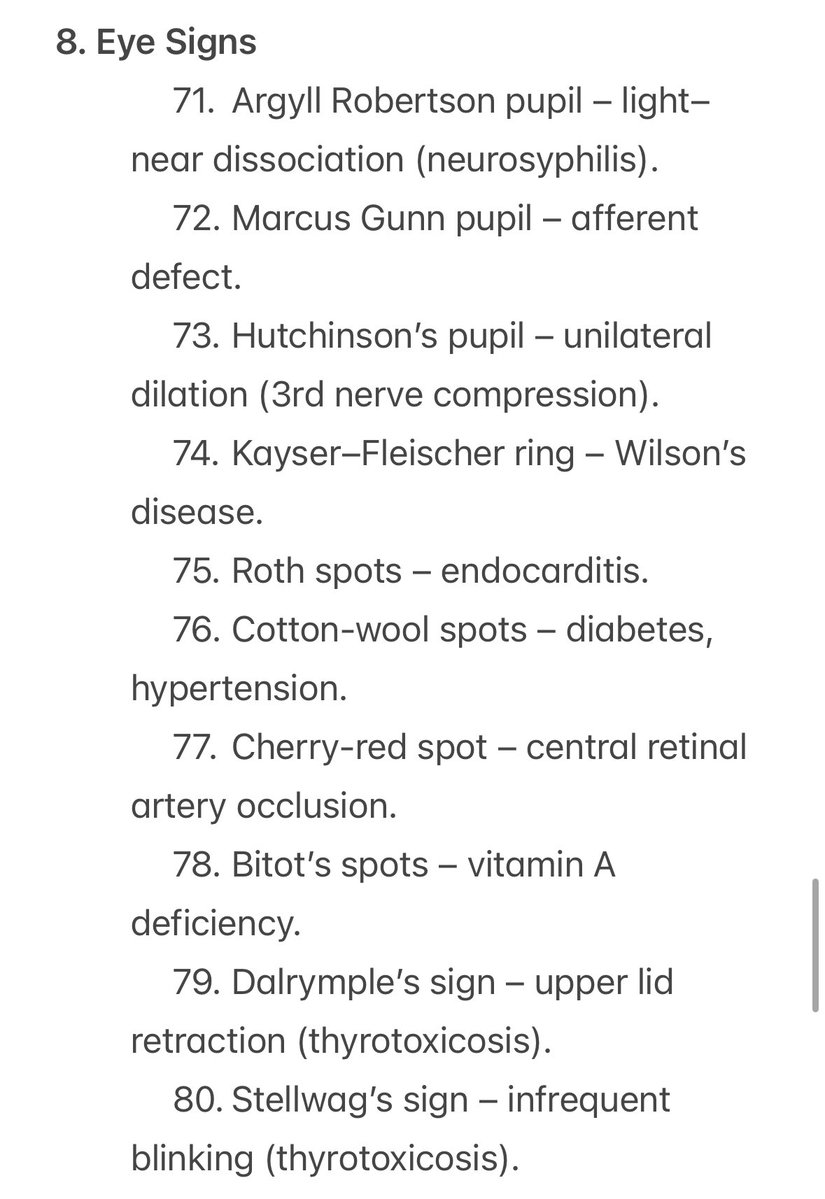
Eye Signs
8️⃣ The eyes are still the quickest exam in medicine.
Argyll Robertson, Hutchinson’s, Kayser–Fleischer —
the iris and cornea reveal what the rest of the body conceals.
8️⃣ The eyes are still the quickest exam in medicine.
Argyll Robertson, Hutchinson’s, Kayser–Fleischer —
the iris and cornea reveal what the rest of the body conceals.
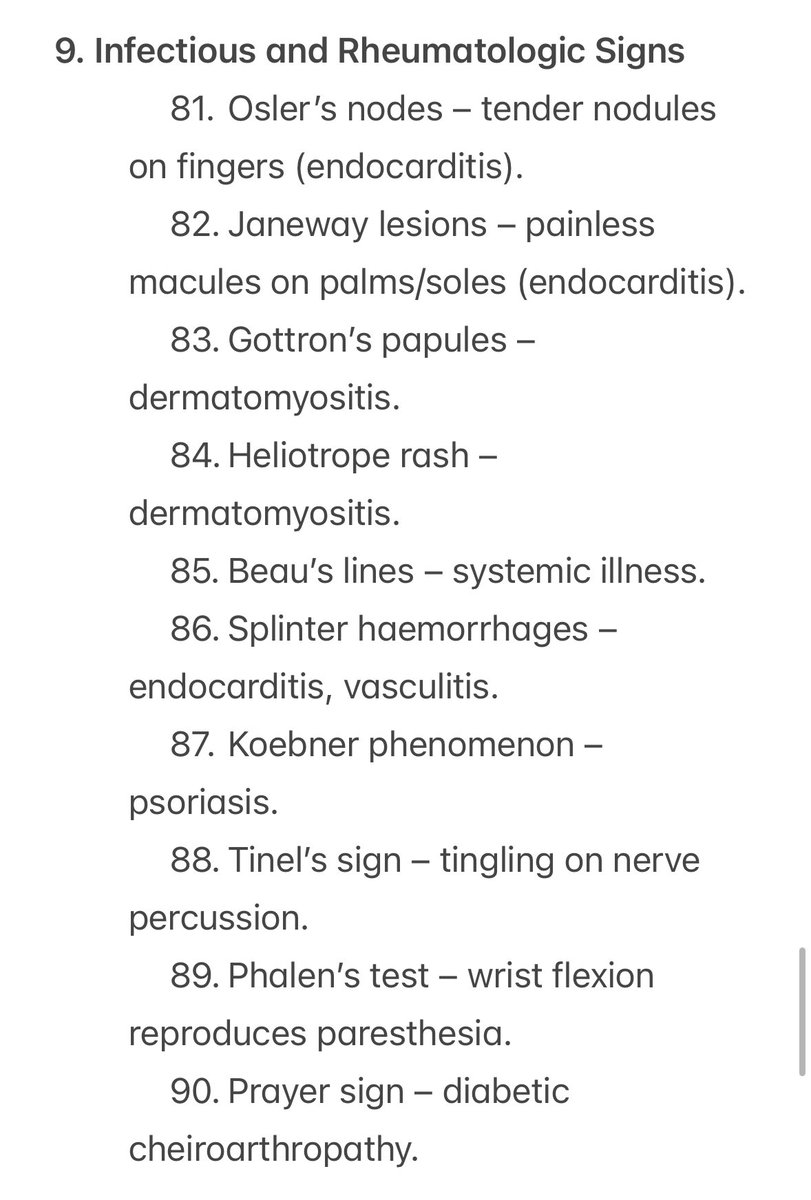
Infectious and Rheumatologic Signs
9️⃣ Infections and autoimmunity leave their signatures on the skin.
Osler, Janeway, Gottron, Heliotrope —
eponyms that remind us inflammation always speaks in color and contour.
9️⃣ Infections and autoimmunity leave their signatures on the skin.
Osler, Janeway, Gottron, Heliotrope —
eponyms that remind us inflammation always speaks in color and contour.
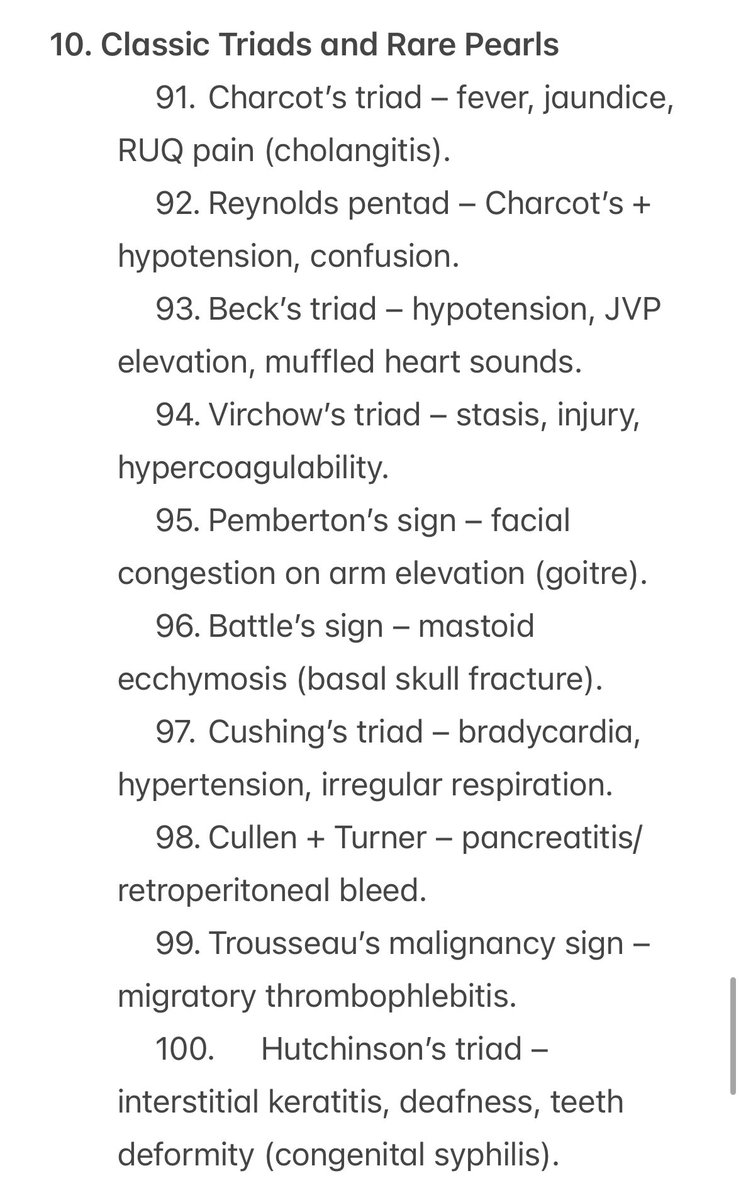
Classic Triads and Rare Pearls
10️⃣ Some signs survive centuries because they save seconds.
Charcot, Cushing, Beck, Virchow —
the giants who turned patterns into diagnosis.
Their language is still medicine’s heartbeat.
10️⃣ Some signs survive centuries because they save seconds.
Charcot, Cushing, Beck, Virchow —
the giants who turned patterns into diagnosis.
Their language is still medicine’s heartbeat.
Closing Line:
100 signs.
100 stories.
1 timeless lesson.
Technology can assist.
But only observation can understand.
— Dr. Aravind Palraj | RheumRounds
#MedTwitter #Hutchison #ClinicalSigns #BedsideMedicine #RheumRounds
100 signs.
100 stories.
1 timeless lesson.
Technology can assist.
But only observation can understand.
— Dr. Aravind Palraj | RheumRounds
#MedTwitter #Hutchison #ClinicalSigns #BedsideMedicine #RheumRounds
• • •
Missing some Tweet in this thread? You can try to
force a refresh