(1/x) Andromeda-Shock 2 was just published in JAMA and is the most important septic shock trial in the past DECADE.
They found that phenotyped resuscitation improves the composite outcome of mortality, vital support, and hospital LOS.
Here's how you can apply this protocol to your practice 👇
They found that phenotyped resuscitation improves the composite outcome of mortality, vital support, and hospital LOS.
Here's how you can apply this protocol to your practice 👇

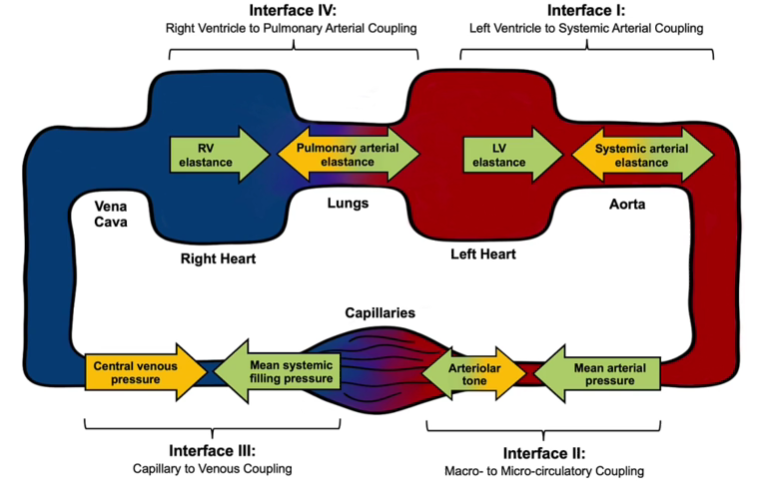
(2/x) At the core of AS2 is the concept of ‘microcirculation’ or that hemodynamic interventions we perform should improve tissue level perfusion.
To assess this, we can use the validated surrogate capillary refill time that helps approximate what is happening in the microcirculation.
Full article is here: jamanetwork.com/journals/jama/…
To assess this, we can use the validated surrogate capillary refill time that helps approximate what is happening in the microcirculation.
Full article is here: jamanetwork.com/journals/jama/…
(3/x) Andromeda-Shock 2 RCT used a tiered approach to guide resuscitation, all centered around cap refill time.
Tier 1:
Check Cap Refill - if normal, periodic monitoring (you can't be better than normal!!)
If abnormal, first check pulse pressure (PP), a surrogate for stroke volume.
If narrow PP, check for fluid responsive.
If wide PP, check diastolic blood pressure and if <50mmHg, augment with norepinephrine.
Repeat cap refill serially.
Tier 1:
Check Cap Refill - if normal, periodic monitoring (you can't be better than normal!!)
If abnormal, first check pulse pressure (PP), a surrogate for stroke volume.
If narrow PP, check for fluid responsive.
If wide PP, check diastolic blood pressure and if <50mmHg, augment with norepinephrine.
Repeat cap refill serially.

(4/x) If after Tier 1 the Cap Refill Time is still abnormal move on to Tier 2 which is echo driven:
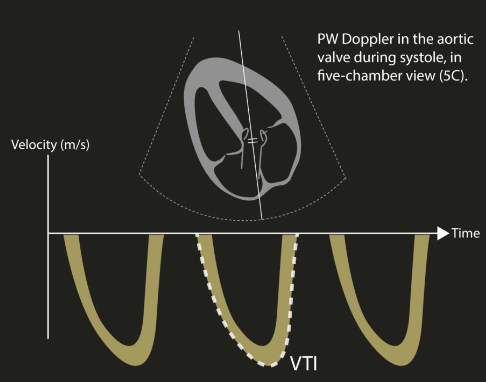
1. Cardiac dysfunction on echo? Inotropes.
2. Fluid responsive? Consider fluid bolus.
3. Still hypoperfused despite this? Consider MAP augmentation challenge.
The key here is that interventions are performed and then their impact on microcirculation assessed through cap refill time.
NO empiric 30ml/kg boluses.
1. Cardiac dysfunction on echo? Inotropes.
2. Fluid responsive? Consider fluid bolus.
3. Still hypoperfused despite this? Consider MAP augmentation challenge.
The key here is that interventions are performed and then their impact on microcirculation assessed through cap refill time.
NO empiric 30ml/kg boluses.

(5/x) So what did the primary outcome show?
A reduction in composite of mortality, vital support, and hospital LOS (driven primarily by vital support)
Directly from the abstract: “There were 131 131 wins (48.9%) in the CRT-PHR group vs 112 787 (42.1%) in the usual care group for the hierarchical composite primary outcome, with a win ratio of 1.16 (95%CI, 1.02-1.33; P = .04).”
A reduction in composite of mortality, vital support, and hospital LOS (driven primarily by vital support)
Directly from the abstract: “There were 131 131 wins (48.9%) in the CRT-PHR group vs 112 787 (42.1%) in the usual care group for the hierarchical composite primary outcome, with a win ratio of 1.16 (95%CI, 1.02-1.33; P = .04).”

(6/x) What about secondary outcomes and other key takehomes?
CRT guided resus patients received less fluid (595 mL vs 847 mL;)
CRT guided resus patients received more dobutamine (84/684 [12.3%] vs 37/694 [5.3%])
CRT guided patients had lower CVP and lactate
CRT guided patients had less FR assessments and received less resuscitative IV fluids
CRT guided patients had greater improvement in SOFA score over 7 days
Across subgroups with greater acuity (high SOFA & lactate) seems to be more of an effect
CRT guided resus patients received less fluid (595 mL vs 847 mL;)
CRT guided resus patients received more dobutamine (84/684 [12.3%] vs 37/694 [5.3%])
CRT guided patients had lower CVP and lactate
CRT guided patients had less FR assessments and received less resuscitative IV fluids
CRT guided patients had greater improvement in SOFA score over 7 days
Across subgroups with greater acuity (high SOFA & lactate) seems to be more of an effect

(7/x) What does this mean for both the management and research of septic shock?
Despite decades of negative trials, we don’t have to be nihilistic. We CAN improve outcomes, but the key is in phenotyping our interventions to the patient in front of us.
We need to STOP performing ‘one-size-fits-all’ trials for a syndrome like sepsis that is so heterogenous.
Despite decades of negative trials, we don’t have to be nihilistic. We CAN improve outcomes, but the key is in phenotyping our interventions to the patient in front of us.
We need to STOP performing ‘one-size-fits-all’ trials for a syndrome like sepsis that is so heterogenous.
(8/x) How do the results of AS-2 change my practice?
1. Assess cap refill time - if normal, monitor periodically.
2. If abnormal, think about SV (e.g. narrow pulse pressure is a low SV surrogate) and if low, consider fluids if fluids responsive. If high pulse pressure and a low diastolic, augment the MAP.
REPEAT THE CRT SERIALLY.
3. If this isn’t working and still abnormal CRT, we need to echo the patient as cardiac dysfunction (and congestion) prevalent. This is a echo (+ VeXUS - our Andromeda-VEXUS paper will help color this in a bit more) and then treat the underlying cardiac dysfunction.
Empiric fluid loading (30ml/kg), one-size fits all resuscitation is not the answer in 2025.
1. Assess cap refill time - if normal, monitor periodically.
2. If abnormal, think about SV (e.g. narrow pulse pressure is a low SV surrogate) and if low, consider fluids if fluids responsive. If high pulse pressure and a low diastolic, augment the MAP.
REPEAT THE CRT SERIALLY.
3. If this isn’t working and still abnormal CRT, we need to echo the patient as cardiac dysfunction (and congestion) prevalent. This is a echo (+ VeXUS - our Andromeda-VEXUS paper will help color this in a bit more) and then treat the underlying cardiac dysfunction.
Empiric fluid loading (30ml/kg), one-size fits all resuscitation is not the answer in 2025.

(9/x) A huge shoutout is needed for all the AS2 investigators, particularly @AndromedaShock @edu_kattan Jan Bakker, Nico Orozco but so many more.
They started this study without funding, and with sheer passion managed to get hundreds of centers worldwide to recruit 1500 patients with phenotyped resuscitation. With this passion, funding, support, and collaborators came to support this vision.
For my friends and colleagues here on X, please read this study and share broadly as I think it has the potential to change how we resuscitate septic shock!!
Full article: (the supplement has a ton of incredible stuff too!) jamanetwork.com/journals/jama/…
Super excited to start analyzing our Andromeda-VEXUS data not that the embargo is lifted, stay tuned!
@NephroP @ArgaizR @ThinkingCC @katiewiskar @KiranRikhraj @nickmmark @TheSGEM @emcrit @PulmCrit @john_basmaji @MaratSlessarev @HoosierPocus @Bram_Rochwerg
They started this study without funding, and with sheer passion managed to get hundreds of centers worldwide to recruit 1500 patients with phenotyped resuscitation. With this passion, funding, support, and collaborators came to support this vision.
For my friends and colleagues here on X, please read this study and share broadly as I think it has the potential to change how we resuscitate septic shock!!
Full article: (the supplement has a ton of incredible stuff too!) jamanetwork.com/journals/jama/…
Super excited to start analyzing our Andromeda-VEXUS data not that the embargo is lifted, stay tuned!
@NephroP @ArgaizR @ThinkingCC @katiewiskar @KiranRikhraj @nickmmark @TheSGEM @emcrit @PulmCrit @john_basmaji @MaratSlessarev @HoosierPocus @Bram_Rochwerg
@AndromedaShock @edu_kattan Pinging a few more to join in the discussion here!!
@icmteaching @DrAkhilX @cardiacACCP @cliffreid @CharlesLutzMD @FH_Verbrugge @jeffgadsden @CriticalCareNow
@icmteaching @DrAkhilX @cardiacACCP @cliffreid @CharlesLutzMD @FH_Verbrugge @jeffgadsden @CriticalCareNow
• • •
Missing some Tweet in this thread? You can try to
force a refresh