
Intensivist ⚕️ POCUS | Hemodynamics | Innovation
Co-founder of https://t.co/A68FZcHc6b -AI research assistant
Hemodynamic Calculators: https://t.co/3MMlpWXhRM
4 subscribers
How to get URL link on X (Twitter) App


 Episode 1: Myth: Volume Status is a single clinical entity.
Episode 1: Myth: Volume Status is a single clinical entity.

 (2/x) Shock is inadequate tissue perfusion (think end organs).
(2/x) Shock is inadequate tissue perfusion (think end organs).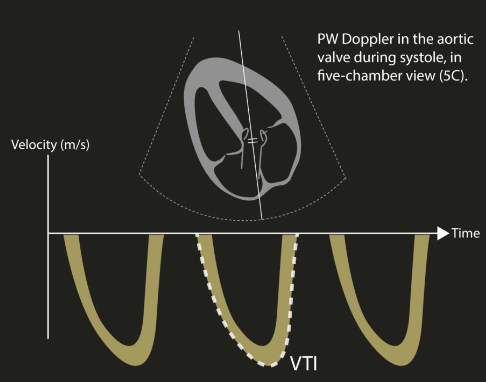

 (2/x) Tip: Goal of diuresis is not just to produce lots of urine... its to produce lots of salty (high Na) urine.
(2/x) Tip: Goal of diuresis is not just to produce lots of urine... its to produce lots of salty (high Na) urine. 
 (2/x) For context, AS-2 was a 1500 patient RCT of a 6 hour resuscitation window compared to standard care in septic shock.
(2/x) For context, AS-2 was a 1500 patient RCT of a 6 hour resuscitation window compared to standard care in septic shock.

 (2/x) At the core of AS2 is the concept of ‘microcirculation’ or that hemodynamic interventions we perform should improve tissue level perfusion.
(2/x) At the core of AS2 is the concept of ‘microcirculation’ or that hemodynamic interventions we perform should improve tissue level perfusion.
 (2/9) Learn from your patients
(2/9) Learn from your patients

 (1/x) I start with a scene survey.
(1/x) I start with a scene survey. 

 (1/x) Deeming a patient impossible to wean should only be done by groups of clinicians with extensive experience in this.
(1/x) Deeming a patient impossible to wean should only be done by groups of clinicians with extensive experience in this. 
 Tip 1: Just go see the patient.
Tip 1: Just go see the patient.
 (1/x) If you missed the webinar, check it out here 👇- it is one of our best.
(1/x) If you missed the webinar, check it out here 👇- it is one of our best.
 (2/x) In medical school, septic shock is described as a distributive shock where patients have hyperdynamic circulation with bounding pulses and warm extremities.
(2/x) In medical school, septic shock is described as a distributive shock where patients have hyperdynamic circulation with bounding pulses and warm extremities.

 (1/5) Cognitive Trap: Search Satisficing Bias.
(1/5) Cognitive Trap: Search Satisficing Bias.
https://twitter.com/ross_prager/status/1935671737485504561(2/x) Of course, fluids may be beneficial in sepsis for some patients! However, this requires a few things to be true.
 (2/x) Don't yell 'everyone who doesn't need to be here leave'.
(2/x) Don't yell 'everyone who doesn't need to be here leave'.
 (2/x) The reason why clinicians feel for the pulse makes sense - we want our CPR to be generating enough stroke volume to create a palpable pulse.
(2/x) The reason why clinicians feel for the pulse makes sense - we want our CPR to be generating enough stroke volume to create a palpable pulse.
 (1/5) Start by assessing the microcirculation (and its surrogates) to determine how severely end organs are impacted. This should help guide how aggressive you are at its management.
(1/5) Start by assessing the microcirculation (and its surrogates) to determine how severely end organs are impacted. This should help guide how aggressive you are at its management.
 (1/10) Patients don't care how much you know, but rather, how you make them feel.
(1/10) Patients don't care how much you know, but rather, how you make them feel.
 (2/x) Who’s being sued?
(2/x) Who’s being sued?
 (2/x) To start, if a non-invasive ventilation (NIV) mask has a good seal, there are really only two key differences between invasive and non-invasive ventilation
(2/x) To start, if a non-invasive ventilation (NIV) mask has a good seal, there are really only two key differences between invasive and non-invasive ventilation

 (2/x) A systematic review with meta-analysis of RCTs by Liu et al. 2021 in Critical Care Medicine demonstrated ....
(2/x) A systematic review with meta-analysis of RCTs by Liu et al. 2021 in Critical Care Medicine demonstrated ....