Oxidative stress is a very important but far more complicated topic than the average person is made to believe.
Here's what you need to know.
Thread🧵



Here's what you need to know.
Thread🧵




*Standard disclaimer that this does not constitute medical advice*
Oxidative stress is characterized by the overproduction of reactive oxygen species (ROS), which can induce mitochondrial DNA mutations, damage the mitochondrial respiratory chain, alter membrane permeability, and influence Ca2+ homeostasis and mitochondrial defense systems.
Calcium homeostasis refers to the maintenance of a constant concentration of calcium ions in the extracellular fluid.
It includes all of the processes that contribute to maintaining calcium at its “set point.”
Because plasma [Ca2+] rapidly equilibrates with the extracellular fluid, ECF [Ca2+] is kept constant by keeping the plasma [Ca2+] constant.
Oxidative stress is characterized by the overproduction of reactive oxygen species (ROS), which can induce mitochondrial DNA mutations, damage the mitochondrial respiratory chain, alter membrane permeability, and influence Ca2+ homeostasis and mitochondrial defense systems.
Calcium homeostasis refers to the maintenance of a constant concentration of calcium ions in the extracellular fluid.
It includes all of the processes that contribute to maintaining calcium at its “set point.”
Because plasma [Ca2+] rapidly equilibrates with the extracellular fluid, ECF [Ca2+] is kept constant by keeping the plasma [Ca2+] constant.

Maintaining a constant plasma [Ca2+] is important for things such as nerve transmission and conduction, cardigan contractility, blood clotting, cell to cell adhesion and of course bone formation.
Now a free radical attack occurs directly at complexes in the mitochondrial respiratory chain.
Mitochondria are normally protected from oxidative damage by a multilayer network of mitochondrial antioxidant systems which consist of superoxide dismutase, catalase, glutathione peroxidase and glutathione reductase together with a number of low molecular weight antioxidants such as α-tocopherol and ubiquinol.
These molecules are particularly effective in scavenging lipid peroxyl radicals and preventing free radical chain reactions of lipid peroxidation.
Cumulative oxidative injuries to mitochondria, triggered by endogenous metabolic processes and/or exogenous oxidative influences, cause mitochondria to progressively become less efficient.
Now a free radical attack occurs directly at complexes in the mitochondrial respiratory chain.
Mitochondria are normally protected from oxidative damage by a multilayer network of mitochondrial antioxidant systems which consist of superoxide dismutase, catalase, glutathione peroxidase and glutathione reductase together with a number of low molecular weight antioxidants such as α-tocopherol and ubiquinol.
These molecules are particularly effective in scavenging lipid peroxyl radicals and preventing free radical chain reactions of lipid peroxidation.
Cumulative oxidative injuries to mitochondria, triggered by endogenous metabolic processes and/or exogenous oxidative influences, cause mitochondria to progressively become less efficient.

As mitochondria progressively lose their functional integrity, ever-greater proportions of oxygen molecules reaching them are converted to ROS.
So the numerous and disparate mitochondrial functions include the synthesis of most of the ATP present in the cell, apoptosis, ion homeostasis, cellular stress response, antioxidant control, redox regulation, mitophagy and the involvement in various biosynthetic pathways.
Oxidative stress occurs when there is an imbalance between free radical production and their detoxification.
So the numerous and disparate mitochondrial functions include the synthesis of most of the ATP present in the cell, apoptosis, ion homeostasis, cellular stress response, antioxidant control, redox regulation, mitophagy and the involvement in various biosynthetic pathways.
Oxidative stress occurs when there is an imbalance between free radical production and their detoxification.

Free radicals are unstable compounds that lead to cell destruction and chronic inflammation.
An atom or group of atoms with an unpaired electron is called a free radical.
A free radical can steal electrons from a stable molecule, creating a new free radical and initiating a chain reaction.
This electron-grabbing is called oxidation and can set up a chain reaction, creating new free radicals and damaging important molecules along the way, similar to how one falling domino can bring down countless more.
Antioxidants are molecules that can donate an electron to stabilize and neutralize free radicals.
An antioxidant can "stop" the free radical chain reaction in its tracks by donating an electron and then the antioxidant itself becomes a free radical.
But antioxidants are not very reactive themselves and have processes for quick stabilization.
An atom or group of atoms with an unpaired electron is called a free radical.
A free radical can steal electrons from a stable molecule, creating a new free radical and initiating a chain reaction.
This electron-grabbing is called oxidation and can set up a chain reaction, creating new free radicals and damaging important molecules along the way, similar to how one falling domino can bring down countless more.
Antioxidants are molecules that can donate an electron to stabilize and neutralize free radicals.
An antioxidant can "stop" the free radical chain reaction in its tracks by donating an electron and then the antioxidant itself becomes a free radical.
But antioxidants are not very reactive themselves and have processes for quick stabilization.

Free radicals are a natural byproduct of metabolic reactions and of exercise, and it’s normal to have low levels of free radicals in the body.
With enough antioxidants present, free radicals can be kept in check so that they aren’t dangerous.
However, too many free radicals and not enough protection from antioxidants creates a situation called oxidative stress.
Free radical development is unavoidable, but human bodies have adapted by setting up and maintaining defense mechanisms that reduce their impact.
The body’s two major defense systems are free radical detoxifying enzymes and antioxidants.
With enough antioxidants present, free radicals can be kept in check so that they aren’t dangerous.
However, too many free radicals and not enough protection from antioxidants creates a situation called oxidative stress.
Free radical development is unavoidable, but human bodies have adapted by setting up and maintaining defense mechanisms that reduce their impact.
The body’s two major defense systems are free radical detoxifying enzymes and antioxidants.

Free radical detoxifying enzyme systems are responsible for protecting the insides of cells from free radical damage.
An antioxidant is any molecule that can block free radicals from stealing electrons. antioxidants act both inside and outside of cells.
The three major enzyme systems and the chemical reactions they catalyze are:
1)Superoxide Dismutases (SOD).
They are essential for free radical detoxification and these enzymes either have manganese, copper or zinc as a cofactor.
2)Catalase.
These enzymes convert hydrogen peroxide to water and oxygen and finish the detoxification process that SOD starts.
3)Glutathione Peroxidases.
These selenium dependent enzymes also convert hydrogen peroxide to water and oxygen.
An antioxidant is any molecule that can block free radicals from stealing electrons. antioxidants act both inside and outside of cells.
The three major enzyme systems and the chemical reactions they catalyze are:
1)Superoxide Dismutases (SOD).
They are essential for free radical detoxification and these enzymes either have manganese, copper or zinc as a cofactor.
2)Catalase.
These enzymes convert hydrogen peroxide to water and oxygen and finish the detoxification process that SOD starts.
3)Glutathione Peroxidases.
These selenium dependent enzymes also convert hydrogen peroxide to water and oxygen.

The body can synthesize some antioxidants, but others must be obtained from the diet.
There are two antioxidants that the body synthesize:
1) Glutathione (which contains a sulfur group that can donate an electron to a free radical, thereby stabilizing it).
2) Uric acid.
There are many different antioxidants in food as well.
-Antioxidant vitamins (Vitamin E, Vitamin C) donate their electrons to free radicals to stabilize them.
-Antioxidant phytochemicals (beta-carotene and other carotenoids) may inhibit the oxidation of lipids or donate electrons.
-Antioxidant minerals act as cofactors within complex antioxidant enzyme systems (superoxide dismutases, catalase, glutathione peroxidases described earlier) to convert free radicals to less damaging substances that can be excreted.
There are two antioxidants that the body synthesize:
1) Glutathione (which contains a sulfur group that can donate an electron to a free radical, thereby stabilizing it).
2) Uric acid.
There are many different antioxidants in food as well.
-Antioxidant vitamins (Vitamin E, Vitamin C) donate their electrons to free radicals to stabilize them.
-Antioxidant phytochemicals (beta-carotene and other carotenoids) may inhibit the oxidation of lipids or donate electrons.
-Antioxidant minerals act as cofactors within complex antioxidant enzyme systems (superoxide dismutases, catalase, glutathione peroxidases described earlier) to convert free radicals to less damaging substances that can be excreted.
1)Vitamin E
Functions: Protects cellular membranes and prevents glutathione depletion.
Because vitamin E is fat-soluble, its antioxidant capacity is especially important to lipids, including those in cell membranes and lipoproteins.
For example, free radicals can oxidize LDL cholesterol (stealing an electron from it), and it is this damaged LDL that lodges in blood vessels and forms the fatty plaques characteristic of atherosclerosis, increasing the risk of heart attack, stroke, and other complications of cardiovascular disease.
After alpha-tocopherol interacts with a free radical it is no longer capable of acting as an antioxidant unless it is enzymatically regenerated.
2)Vitamin C
Functions: Protects DNA, RNA, proteins and lipids and aids in regenerating vitamin E. Vitamin C’s ability to easily donate electrons makes it a highly effective antioxidant.
Since it is water-soluble, it acts both inside and outside cells to protect molecules in aqueous environments.
Vitamin C also plays a vital role in regenerating vitamin E after it has acted as an antioxidant, allowing it to be recycled and used again.
3)Selenium
Functions: Cofactor of free radical detoxifying enzymes, maintains glutathione levels, aids in regeneration of vitamins C and E.
Selenium is an essential trace mineral that is part of the structure of at least 25 proteins in the body with functions in thyroid hormone metabolism, DNA synthesis, reproduction and protecting the immune system.
As part of antioxidant enzymes, selenium helps to regenerate other antioxidants, including vitamin C.
These enzymes also protect lipids from free radicals, and, in doing so, spare vitamin E.
4) Carotenoids from sources such as pumpkin, squash, peaches, apricots which function as free radical scavengers.
5) CO2
C02 besides being a great antioxidant, is very essential for our metabolic health since it stabilizes and even activates mitochondria.
CO2 is a great anti-inflammatory, a great tool for someone to protect himself against ammonia and its byproducts, it can speed up the detoxification of polyunsaturated fatty acids and it’s a great tool to boost your performance (both mental and physical) as well.
How to increase CO2?
Two quick ways are:
1)The Buteyko breathing technique which is great for asthma, will help you with increasing CO2 levels.
2) Thiamine (B1) (especially pre workout)
3) Bag breathing
Functions: Protects cellular membranes and prevents glutathione depletion.
Because vitamin E is fat-soluble, its antioxidant capacity is especially important to lipids, including those in cell membranes and lipoproteins.
For example, free radicals can oxidize LDL cholesterol (stealing an electron from it), and it is this damaged LDL that lodges in blood vessels and forms the fatty plaques characteristic of atherosclerosis, increasing the risk of heart attack, stroke, and other complications of cardiovascular disease.
After alpha-tocopherol interacts with a free radical it is no longer capable of acting as an antioxidant unless it is enzymatically regenerated.
2)Vitamin C
Functions: Protects DNA, RNA, proteins and lipids and aids in regenerating vitamin E. Vitamin C’s ability to easily donate electrons makes it a highly effective antioxidant.
Since it is water-soluble, it acts both inside and outside cells to protect molecules in aqueous environments.
Vitamin C also plays a vital role in regenerating vitamin E after it has acted as an antioxidant, allowing it to be recycled and used again.
3)Selenium
Functions: Cofactor of free radical detoxifying enzymes, maintains glutathione levels, aids in regeneration of vitamins C and E.
Selenium is an essential trace mineral that is part of the structure of at least 25 proteins in the body with functions in thyroid hormone metabolism, DNA synthesis, reproduction and protecting the immune system.
As part of antioxidant enzymes, selenium helps to regenerate other antioxidants, including vitamin C.
These enzymes also protect lipids from free radicals, and, in doing so, spare vitamin E.
4) Carotenoids from sources such as pumpkin, squash, peaches, apricots which function as free radical scavengers.
5) CO2
C02 besides being a great antioxidant, is very essential for our metabolic health since it stabilizes and even activates mitochondria.
CO2 is a great anti-inflammatory, a great tool for someone to protect himself against ammonia and its byproducts, it can speed up the detoxification of polyunsaturated fatty acids and it’s a great tool to boost your performance (both mental and physical) as well.
How to increase CO2?
Two quick ways are:
1)The Buteyko breathing technique which is great for asthma, will help you with increasing CO2 levels.
2) Thiamine (B1) (especially pre workout)
3) Bag breathing

BUT, the most powerful antioxidant is not vitamin C, E or even glutathione.
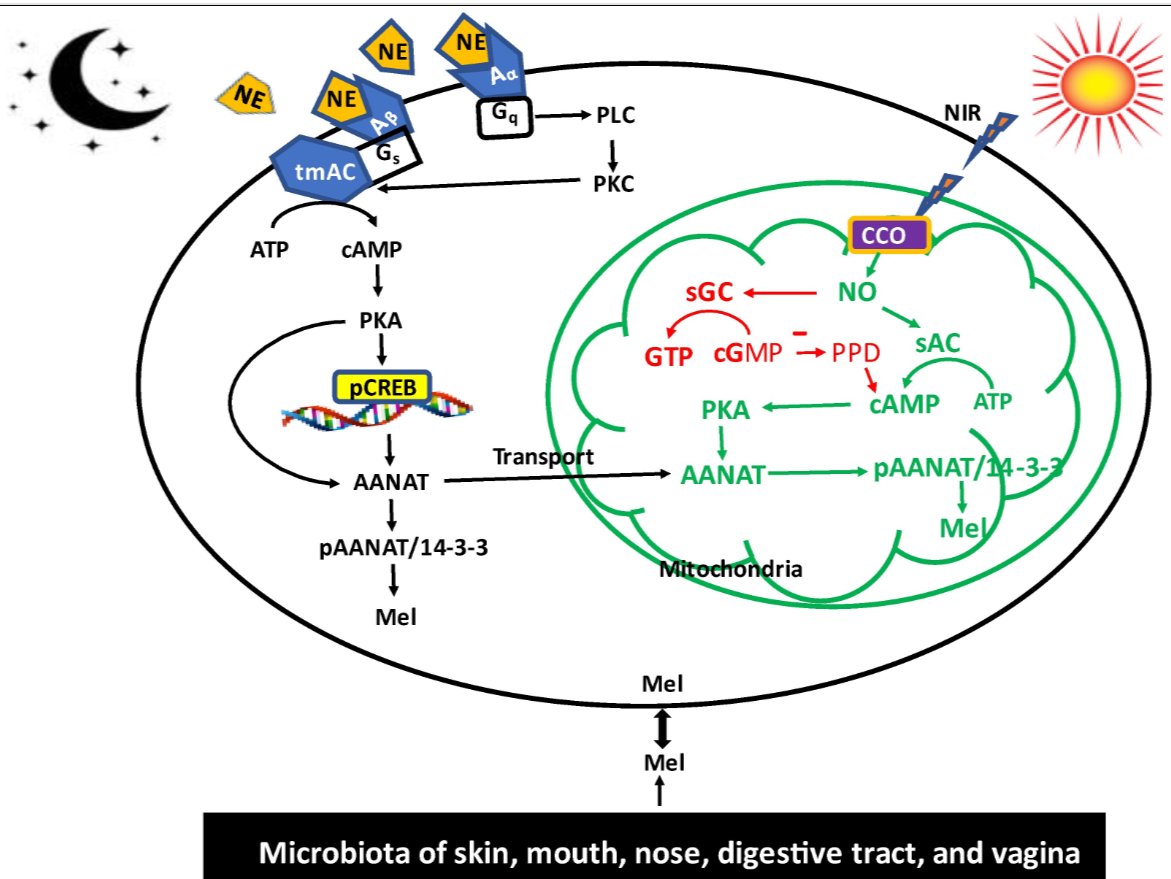
Even though all of these are extremely important since each one has unique roles within the human body (for example, glutathione is critical for detoxification) the most powerful antioxidant is free and it's called melatonin.
Melatonin, chemically known as N-acetyl-5-methoxytryptamine, is classified as an indoleamine that is derived from the amino acid tryptophan.
It is evolutionarily ancient and present in organisms from bacteria to humans.
Now technically speaking, since it is synthesized in many non-endocrine organs and doesn't target a specific organ it’s not a hormone (melatonin fits this in the pineal context only).
So melatonin also acts as a paracrine and autocrine signaling molecule, influencing cellular processes across multiple tissues without requiring endocrine-specific pathways.
-It inhibits cancer cell proliferation, induces apoptosis, and enhances immune surveillance.
Melatonin is crucial for our immune system, gut health, skin health, brain health and is even linked with erectile dysfunction.
For example:
-Melatonin regulates gut motility, protects the mucosal barrier and modulates the gut microbiota.
-It reduces hypertension, improves endothelial func
But it’s not hard to understand why melatonin has these effects.
For example, melatonin as an amphipathic free radical scavenger (it has hydrophilic and hydrophobic nature and this dual solubility gives it broader reach (it goes through membranes and blood alike for example)), neutralizes free radicals like:
-Hydroxyl radical: A ROS capable of damaging DNA, proteins, and lipids.
Melatonin neutralizes this with a reaction rate constant near the diffusion limit making it one of the most efficient scavengers of this radical.
-Superoxide anion : A precursor to other ROS, produced during ETC leakage.
-Hydrogen peroxide.
-Peroxynitrite.
Even though all of these are extremely important since each one has unique roles within the human body (for example, glutathione is critical for detoxification) the most powerful antioxidant is free and it's called melatonin.
Melatonin, chemically known as N-acetyl-5-methoxytryptamine, is classified as an indoleamine that is derived from the amino acid tryptophan.
It is evolutionarily ancient and present in organisms from bacteria to humans.
Now technically speaking, since it is synthesized in many non-endocrine organs and doesn't target a specific organ it’s not a hormone (melatonin fits this in the pineal context only).
So melatonin also acts as a paracrine and autocrine signaling molecule, influencing cellular processes across multiple tissues without requiring endocrine-specific pathways.
-It inhibits cancer cell proliferation, induces apoptosis, and enhances immune surveillance.
Melatonin is crucial for our immune system, gut health, skin health, brain health and is even linked with erectile dysfunction.
For example:
-Melatonin regulates gut motility, protects the mucosal barrier and modulates the gut microbiota.
-It reduces hypertension, improves endothelial func
But it’s not hard to understand why melatonin has these effects.
For example, melatonin as an amphipathic free radical scavenger (it has hydrophilic and hydrophobic nature and this dual solubility gives it broader reach (it goes through membranes and blood alike for example)), neutralizes free radicals like:
-Hydroxyl radical: A ROS capable of damaging DNA, proteins, and lipids.
Melatonin neutralizes this with a reaction rate constant near the diffusion limit making it one of the most efficient scavengers of this radical.
-Superoxide anion : A precursor to other ROS, produced during ETC leakage.
-Hydrogen peroxide.
-Peroxynitrite.

"Is melatonin that effective?"
Yes.
A single melatonin molecule can neutralize up to 10 ROS/RNS through its metabolites compared to classical antioxidants like vitamin C (1:1 scavenging ratio).
Not only that but unlike other antioxidants, melatonin does not exhibit significant pro-oxidant activity.
After donating electrons, its reaction products such as N1-acetyl-N2-formyl-5-methoxykynuramine, or AFMK are either inert or continue to scavenge radicals, creating a “cascade” effect.
It also enhances the body’s endogenous antioxidant defenses by upregulating key enzymes and molecules such as the GSH system (glutathione) where melatonin increases GSH levels and the activity of GSH-related enzymes such as γ-Glutamylcysteine ligase, glutathione peroxidase, glutathione reductase, superoxide dismutase, catalase and heme oxygenase-1.
Melatonin’s hydrophobic properties also make it especially effective at preventing lipid peroxidation (a chain reaction where ROS damage polyunsaturated fatty acids in cell membranes) where melatonin interrupts the propagation phase of lipid peroxidation by neutralizing lipid peroxyl radicals and stabilizing membrane fluidity.
And finally when it comes to libido and reproduction melatonin can modulate gonadotropin-releasing hormone (GnRH) secretion from the hypothalamus for example.
It also reduces amyloid-beta production by inhibiting β-secretase (BACE1) (an enzyme that cleaves amyloid precursor protein (APP) into Aβ) and enhancing Aβ clearance by upregulating enzymes like neprilysin.
Or, when it comes to the immune system it stimulates the production of several types of immune system cells such as natural killer cells and CD4+ cells but also it inhibits Warburg metabolism by keeping pyruvate flowing into the TCA cycle and when the immune response is overactive, melatonin reduces inflammatory mediators and neutrophil infiltration.
Yes.
A single melatonin molecule can neutralize up to 10 ROS/RNS through its metabolites compared to classical antioxidants like vitamin C (1:1 scavenging ratio).
Not only that but unlike other antioxidants, melatonin does not exhibit significant pro-oxidant activity.
After donating electrons, its reaction products such as N1-acetyl-N2-formyl-5-methoxykynuramine, or AFMK are either inert or continue to scavenge radicals, creating a “cascade” effect.
It also enhances the body’s endogenous antioxidant defenses by upregulating key enzymes and molecules such as the GSH system (glutathione) where melatonin increases GSH levels and the activity of GSH-related enzymes such as γ-Glutamylcysteine ligase, glutathione peroxidase, glutathione reductase, superoxide dismutase, catalase and heme oxygenase-1.
Melatonin’s hydrophobic properties also make it especially effective at preventing lipid peroxidation (a chain reaction where ROS damage polyunsaturated fatty acids in cell membranes) where melatonin interrupts the propagation phase of lipid peroxidation by neutralizing lipid peroxyl radicals and stabilizing membrane fluidity.
And finally when it comes to libido and reproduction melatonin can modulate gonadotropin-releasing hormone (GnRH) secretion from the hypothalamus for example.
It also reduces amyloid-beta production by inhibiting β-secretase (BACE1) (an enzyme that cleaves amyloid precursor protein (APP) into Aβ) and enhancing Aβ clearance by upregulating enzymes like neprilysin.
Or, when it comes to the immune system it stimulates the production of several types of immune system cells such as natural killer cells and CD4+ cells but also it inhibits Warburg metabolism by keeping pyruvate flowing into the TCA cycle and when the immune response is overactive, melatonin reduces inflammatory mediators and neutrophil infiltration.

Wrapping up with diving a bit deeper into redox.
When we have an interaction where an oxidizing substance loses electrons and a reducing substance gains electrons, we have a redox reaction.
An easy-to-understand example of a redox reaction is the rusting of iron (where iron loses electrons and oxygen receives electrons (and thus acts as an oxidizing agent)).
So in a redox reaction -> both reduction and oxidation occur.
Also terms such as oxidation, oxidizing agent, reduction, reducing agent and redox are not that hard to understand.
But this transfer of electrons is not a small thing. It's a fundamental process for life itself and when we interrupt it, problems will inevitably happen.
Even when our bodies break down glucose and fat redox reactions occur.
Now, ROS can in fact cause a lot of trouble but here's the deal, some of the them have beneficial roles and are necessary for processes such as apoptosis to run smoothly.
Otherwise we wouldn't adapt to literally having thousands of them.
Or you can think of it in terms of oxidative stress (something that harms the redox state of a cell) and oxidative eustress.
So when it comes to ROS, it's all about balance/the equilibrium.
In this journey redox cofactors or redox pairs (they participate in the transfer of electrons in a number of redox reactions ) such as:
-NAD and NADH
-NADP and NADPH
-Ubiquinone and ubiquinol
-GSSG and GSH
-FAD+ and FADH2
-FMN and FMN2
will be of vital importance.
Wtf are all these?
An easy place to start is with the following: NADH stands for "nicotinamide adenine dinucleotide plus hydrogen (H)" NADH (and FADH2) are generated for example during glucose metabolism via glycolysis and the tricarboxylic acid cycle or β-oxidation of fatty acids and are oxidized to NAD+ (and FAD) while protons are pumped to the inner mitochondrial membrane through respiratory complexes I, III, and IV (NADH is the product and NAD is the reactant)
NAD+ is synthesized from four precursors: tryptophan, nicotinic acid (pyridine-3-carboxylic acid), nicotinamide (nicotinic acid amide), nicotinamide mononucleotide (NMN) and nicotinamide riboside (NR).
So from the get go, two things you can do in order to support redox is trying to get off statins, not over consuming food and getting enough B vitamins.
Especially B2 since it's also essential to the formation of the coenzymes FMN and FAD and the synthesis of the niacin-containing coenzymes, NAD and NADP, from tryptophan involves the FAD-dependent enzyme, kynurenine 3-monooxygenase so a dietary deficiency of riboflavin can decrease the production of NAD as well.
When we have an interaction where an oxidizing substance loses electrons and a reducing substance gains electrons, we have a redox reaction.
An easy-to-understand example of a redox reaction is the rusting of iron (where iron loses electrons and oxygen receives electrons (and thus acts as an oxidizing agent)).
So in a redox reaction -> both reduction and oxidation occur.
Also terms such as oxidation, oxidizing agent, reduction, reducing agent and redox are not that hard to understand.
But this transfer of electrons is not a small thing. It's a fundamental process for life itself and when we interrupt it, problems will inevitably happen.
Even when our bodies break down glucose and fat redox reactions occur.
Now, ROS can in fact cause a lot of trouble but here's the deal, some of the them have beneficial roles and are necessary for processes such as apoptosis to run smoothly.
Otherwise we wouldn't adapt to literally having thousands of them.
Or you can think of it in terms of oxidative stress (something that harms the redox state of a cell) and oxidative eustress.
So when it comes to ROS, it's all about balance/the equilibrium.
In this journey redox cofactors or redox pairs (they participate in the transfer of electrons in a number of redox reactions ) such as:
-NAD and NADH
-NADP and NADPH
-Ubiquinone and ubiquinol
-GSSG and GSH
-FAD+ and FADH2
-FMN and FMN2
will be of vital importance.
Wtf are all these?
An easy place to start is with the following: NADH stands for "nicotinamide adenine dinucleotide plus hydrogen (H)" NADH (and FADH2) are generated for example during glucose metabolism via glycolysis and the tricarboxylic acid cycle or β-oxidation of fatty acids and are oxidized to NAD+ (and FAD) while protons are pumped to the inner mitochondrial membrane through respiratory complexes I, III, and IV (NADH is the product and NAD is the reactant)
NAD+ is synthesized from four precursors: tryptophan, nicotinic acid (pyridine-3-carboxylic acid), nicotinamide (nicotinic acid amide), nicotinamide mononucleotide (NMN) and nicotinamide riboside (NR).
So from the get go, two things you can do in order to support redox is trying to get off statins, not over consuming food and getting enough B vitamins.
Especially B2 since it's also essential to the formation of the coenzymes FMN and FAD and the synthesis of the niacin-containing coenzymes, NAD and NADP, from tryptophan involves the FAD-dependent enzyme, kynurenine 3-monooxygenase so a dietary deficiency of riboflavin can decrease the production of NAD as well.

Other things you can do in order to support these include:
-Getting quality sleep in a dark room + all the nutrients that are needed for melatonin such as vitamin D and B vitamins.
You can approach this from multiple angles but we will approach it through OXPHOS since a major function of it is to consume NADH and recycle NAD+.
Guess what increases OXPHOS? Melatonin.
Then supplemental tools regarding the NADH/NAD + ratio in general include:
-Quercetin
-Blackseed oil
-M. Blue
So if you want to add something extra choose the one that's more suitable for you.
Things such as hesperidin and naringenin are also shown to help with it but not a lot and can have a bigger downside in the doses that need to be used compared to these 3.
Now what are potential symptoms of messed up redox?
*First you can test the erythrocyte sedimentation rate if you want.
Then, symptoms include things such as anemia, inability to detox properly that can show in the skin and liver, fatigue, low libido/energy in general, very low LDL, sleep issues, dry skin, high cortisol and getting sick very often are the classic ones.
So what you can do in order to improve your redox potential besides the things already mentioned?
-Get natural sunlight first thing in the morning
-Get enough vitamin K and CoQ10
-Avoid pesticides
-Quality seafood
-Avoid alcohol
-Moderate exercise (just get about and walk every day, lift, run/fight/swim etc 3-4/week)
-Blue light blocking programs/glasses
-Some molybdenum since it also is needed for FAD and FMN
-Remember that zinc and BCAAs are crucial for α-MSH
-Avoid things that have sodium fluoride
-Avoid heavy metals
-Ground
-Get thyroid supportive nutrients such as vitamin D, selenium, zinc, iodine etc since thyroid hormones affect flavokinase activity quite a lot and FAD synthetase a bit.
-Lower stress
-Sweat
-Potassium (very very high redox potential).
-Support acetyl-CoA, GGCX etc with other means could also come into play.
-Magnesium
-Regulate iron properly (besides nutrients such as magnesium, B vitamins, copper, zinc, vitamin D etc you'll have to fix your gut if you've been struggling with anemia for a long time)
-Some cold exposure
-Getting quality sleep in a dark room + all the nutrients that are needed for melatonin such as vitamin D and B vitamins.
You can approach this from multiple angles but we will approach it through OXPHOS since a major function of it is to consume NADH and recycle NAD+.
Guess what increases OXPHOS? Melatonin.
Then supplemental tools regarding the NADH/NAD + ratio in general include:
-Quercetin
-Blackseed oil
-M. Blue
So if you want to add something extra choose the one that's more suitable for you.
Things such as hesperidin and naringenin are also shown to help with it but not a lot and can have a bigger downside in the doses that need to be used compared to these 3.
Now what are potential symptoms of messed up redox?
*First you can test the erythrocyte sedimentation rate if you want.
Then, symptoms include things such as anemia, inability to detox properly that can show in the skin and liver, fatigue, low libido/energy in general, very low LDL, sleep issues, dry skin, high cortisol and getting sick very often are the classic ones.
So what you can do in order to improve your redox potential besides the things already mentioned?
-Get natural sunlight first thing in the morning
-Get enough vitamin K and CoQ10
-Avoid pesticides
-Quality seafood
-Avoid alcohol
-Moderate exercise (just get about and walk every day, lift, run/fight/swim etc 3-4/week)
-Blue light blocking programs/glasses
-Some molybdenum since it also is needed for FAD and FMN
-Remember that zinc and BCAAs are crucial for α-MSH
-Avoid things that have sodium fluoride
-Avoid heavy metals
-Ground
-Get thyroid supportive nutrients such as vitamin D, selenium, zinc, iodine etc since thyroid hormones affect flavokinase activity quite a lot and FAD synthetase a bit.
-Lower stress
-Sweat
-Potassium (very very high redox potential).
-Support acetyl-CoA, GGCX etc with other means could also come into play.
-Magnesium
-Regulate iron properly (besides nutrients such as magnesium, B vitamins, copper, zinc, vitamin D etc you'll have to fix your gut if you've been struggling with anemia for a long time)
-Some cold exposure
I hope that you enjoyed this thread.
If you did, make sure to leave a like/RT.
If you did, make sure to leave a like/RT.
https://x.com/Helios_Movement/status/1986801086058111431
• • •
Missing some Tweet in this thread? You can try to
force a refresh