🧵 Why you cannot be oedematous and hypovolaemic at steady state
“Puffy but intravascularly dry”?
⚠️The most persistent myth in IV fluid therapy
#FOAMed #physiology #MedX
“Puffy but intravascularly dry”?
⚠️The most persistent myth in IV fluid therapy
#FOAMed #physiology #MedX
2/
Capillaries filter fluid continuously.
Lymphatics return that filtered fluid continuously.
Daily:
• Filtration ≈ several litres
• Lymph return ≈ several litres
• Net plasma loss ≈ zero
No oedema. No hypovolaemia.
Capillaries filter fluid continuously.
Lymphatics return that filtered fluid continuously.
Daily:
• Filtration ≈ several litres
• Lymph return ≈ several litres
• Net plasma loss ≈ zero
No oedema. No hypovolaemia.
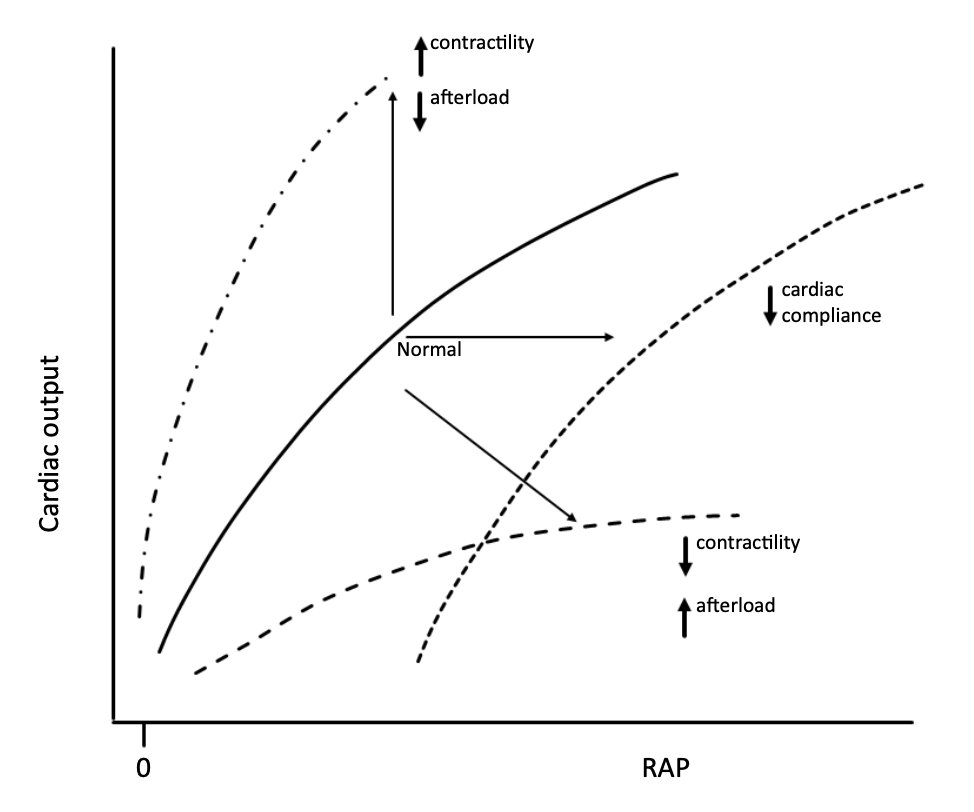
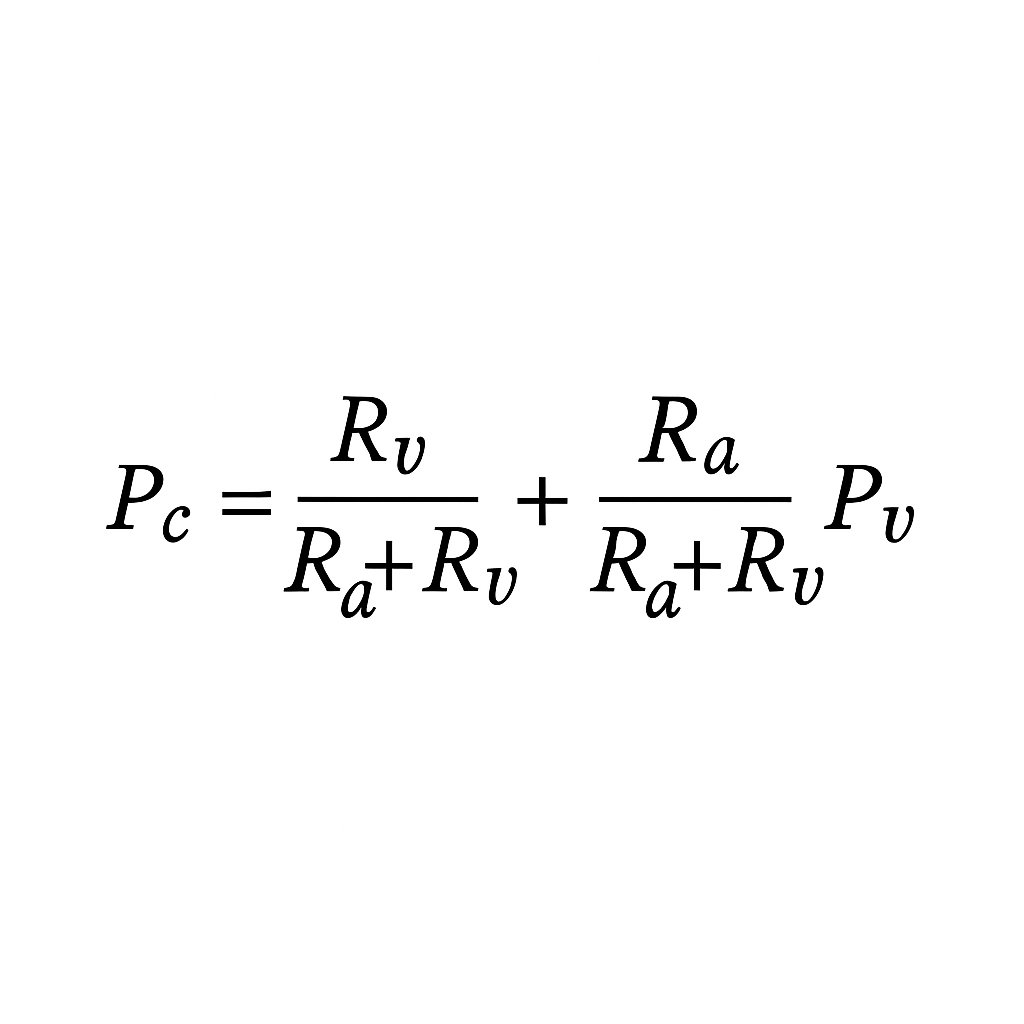
3/
Two states exist:
High capillary pressure (Pc) → ↑ filtration (Jv) → lymph works harder → oedema only when filtration exceeds lymph drainage.
Low Pc → filtration ↓ towards zero → lymph dominates → plasma volume ↑ → oedema resolves.
You cannot occupy both states at once.
Two states exist:
High capillary pressure (Pc) → ↑ filtration (Jv) → lymph works harder → oedema only when filtration exceeds lymph drainage.
Low Pc → filtration ↓ towards zero → lymph dominates → plasma volume ↑ → oedema resolves.
You cannot occupy both states at once.
4/
In true hypovolaemia:
• Pc is low
• Jv ≈ zero
• Lymph returns a few hundred mL/h
• Plasma volume is defended (transient reabsorption, continued lymph return)
Any oedema shrinks, not grows
In true hypovolaemia:
• Pc is low
• Jv ≈ zero
• Lymph returns a few hundred mL/h
• Plasma volume is defended (transient reabsorption, continued lymph return)
Any oedema shrinks, not grows
5/ The 1/3–2/3 myth
We were all taught: “Only 1/3 of crystalloid stays intravascular; 2/3 goes interstitial.”
This is only true in euvolaemia, when Pc lies near the J-point and filtration is brisk.
In hypovolaemia, Pc sits below the J-point.
Filtration stops.
→ 100% of infused fluid stays intravascular until Pc rises back toward the J-point.
→ No oedema forms during this phase.
Ignoring this is the source of enormous iatrogenic overload.
We were all taught: “Only 1/3 of crystalloid stays intravascular; 2/3 goes interstitial.”
This is only true in euvolaemia, when Pc lies near the J-point and filtration is brisk.
In hypovolaemia, Pc sits below the J-point.
Filtration stops.
→ 100% of infused fluid stays intravascular until Pc rises back toward the J-point.
→ No oedema forms during this phase.
Ignoring this is the source of enormous iatrogenic overload.
6/
Once euvolaemia is restored, Pc moves back toward the J-point.
Any additional fluid now raises Pc and accelerates filtration.
Lymph flow increases, but it can only recirculate fluid – not remove the excess.
Total ECF volume expands, and oedema develops once enough extra volume has been added.
Once euvolaemia is restored, Pc moves back toward the J-point.
Any additional fluid now raises Pc and accelerates filtration.
Lymph flow increases, but it can only recirculate fluid – not remove the excess.
Total ECF volume expands, and oedema develops once enough extra volume has been added.
7/
Oedema therefore reflects normal or high intravascular volume + high Pc in the context of expanded ECF volume.
Even with high lymph flow, the surplus fluid has to sit somewhere – most ends up in the interstitium.
If oedema exists at equilibrium, the intravascular space cannot be depleted.
Hypovolaemia = Pc too low to drive filtration
Oedema = Pc high with excess ECF
These states cannot coexist at steady state.
Oedema therefore reflects normal or high intravascular volume + high Pc in the context of expanded ECF volume.
Even with high lymph flow, the surplus fluid has to sit somewhere – most ends up in the interstitium.
If oedema exists at equilibrium, the intravascular space cannot be depleted.
Hypovolaemia = Pc too low to drive filtration
Oedema = Pc high with excess ECF
These states cannot coexist at steady state.
8/
Transient ≠ steady state
• Significant haemorrhage
• Sudden aggressive UF
• First hours of severe burns
• Anaphylaxis / Clarkson’s
These are transition phases, not steady-state ICU physiology.
Transient ≠ steady state
• Significant haemorrhage
• Sudden aggressive UF
• First hours of severe burns
• Anaphylaxis / Clarkson’s
These are transition phases, not steady-state ICU physiology.
9/ The sepsis misconception
Septic patients on arrival are vasodilated and hypotensive, but not oedematous – and there is no haemoconcentration.
No Hb rise = no intravascular fluid loss.
They present with high Pc, high Jv, and matched lymph return: a high-flow circuit, not hypovolaemia.
They only become oedematous after we give litres of IV fluid.
Septic patients on arrival are vasodilated and hypotensive, but not oedematous – and there is no haemoconcentration.
No Hb rise = no intravascular fluid loss.
They present with high Pc, high Jv, and matched lymph return: a high-flow circuit, not hypovolaemia.
They only become oedematous after we give litres of IV fluid.
10/
What about studies showing that in early sepsis or burns, Pi becomes very negative and the lymphatic pump transiently weakens?
True – but these reflect the acute, non–steady-state phase (cytokine storm, NO surge) and are often based on modelled inferences, not direct multi-organ lymph-flow measurement.
Where lymph flow is measured directly (animal models), inflammation generally increases lymph flow, not decreases it.
These findings describe the transition, not equilibrium physiology.
What about studies showing that in early sepsis or burns, Pi becomes very negative and the lymphatic pump transiently weakens?
True – but these reflect the acute, non–steady-state phase (cytokine storm, NO surge) and are often based on modelled inferences, not direct multi-organ lymph-flow measurement.
Where lymph flow is measured directly (animal models), inflammation generally increases lymph flow, not decreases it.
These findings describe the transition, not equilibrium physiology.
11/
By the time the system reaches equilibrium, the picture is different.
Pc is high, Jv is high, and lymph flow is recirculating that filtrate – so intravascular volume is preserved unless extra fluid is added.
Oedema appears only after IV loading pushes Pc above the J-point.
Direct measurements support this; claims of sustained lymph failure are largely modelling artefacts, not steady-state human physiology.
This is why vasopressor-first is safe.
By the time the system reaches equilibrium, the picture is different.
Pc is high, Jv is high, and lymph flow is recirculating that filtrate – so intravascular volume is preserved unless extra fluid is added.
Oedema appears only after IV loading pushes Pc above the J-point.
Direct measurements support this; claims of sustained lymph failure are largely modelling artefacts, not steady-state human physiology.
This is why vasopressor-first is safe.
12/
If you see oedema plus hypotension, the issue isn’t “dryness” – it’s usually:
• High RAP
• Venous congestion
• Impaired lymph return
• Low SVR
• Low Pms
A fluid bolus may nudge Pms up for a few minutes, but it quickly raises Pc and congestion again.
Net effect: adding fluid worsens all of these.
If you see oedema plus hypotension, the issue isn’t “dryness” – it’s usually:
• High RAP
• Venous congestion
• Impaired lymph return
• Low SVR
• Low Pms
A fluid bolus may nudge Pms up for a few minutes, but it quickly raises Pc and congestion again.
Net effect: adding fluid worsens all of these.
13/
Conversely, in true hypovolaemia:
Any fluid – even water – stays intravascular until Pc reaches the J-point.
You cannot generate oedema while Pc remains low.
Conversely, in true hypovolaemia:
Any fluid – even water – stays intravascular until Pc reaches the J-point.
You cannot generate oedema while Pc remains low.
14/
So the rule becomes simple:
🟦 Oedema = high-pressure, high-volume physiology (expanded ECF)
🟥 Hypovolaemia = low-pressure, low-filtration physiology
You cannot be both at steady state unless lymphatics fail catastrophically – a rare extreme, not the pattern of routine sepsis.
So the rule becomes simple:
🟦 Oedema = high-pressure, high-volume physiology (expanded ECF)
🟥 Hypovolaemia = low-pressure, low-filtration physiology
You cannot be both at steady state unless lymphatics fail catastrophically – a rare extreme, not the pattern of routine sepsis.
15/ Takeaway
Oedema requires a high Pc state.
Hypovolaemia requires a low Pc state.
These cannot coexist at steady state with functioning lymphatics.
The “oedematous but dry” idea is a relic – and has driven decades of harmful fluid overload.
Oedema requires a high Pc state.
Hypovolaemia requires a low Pc state.
These cannot coexist at steady state with functioning lymphatics.
The “oedematous but dry” idea is a relic – and has driven decades of harmful fluid overload.
16/
Next up:
Albumin — 70 years, 700 studies, zero sustained benefit.
And why almost everything people think it does is actually just lymph flow.
#MedX #ICU #FluidTherapy #Physiology
Next up:
Albumin — 70 years, 700 studies, zero sustained benefit.
And why almost everything people think it does is actually just lymph flow.
#MedX #ICU #FluidTherapy #Physiology
• • •
Missing some Tweet in this thread? You can try to
force a refresh