
#zentensivist #FUSIC Haemodynamics National Lead. ICS trustee. BSE level 2. BJJ ⬛️⬛️🟥⬛️ @Turningthe_Tide. No politics, just #foamed #pocus #haemodynamics
2 subscribers
How to get URL link on X (Twitter) App



 2️⃣
2️⃣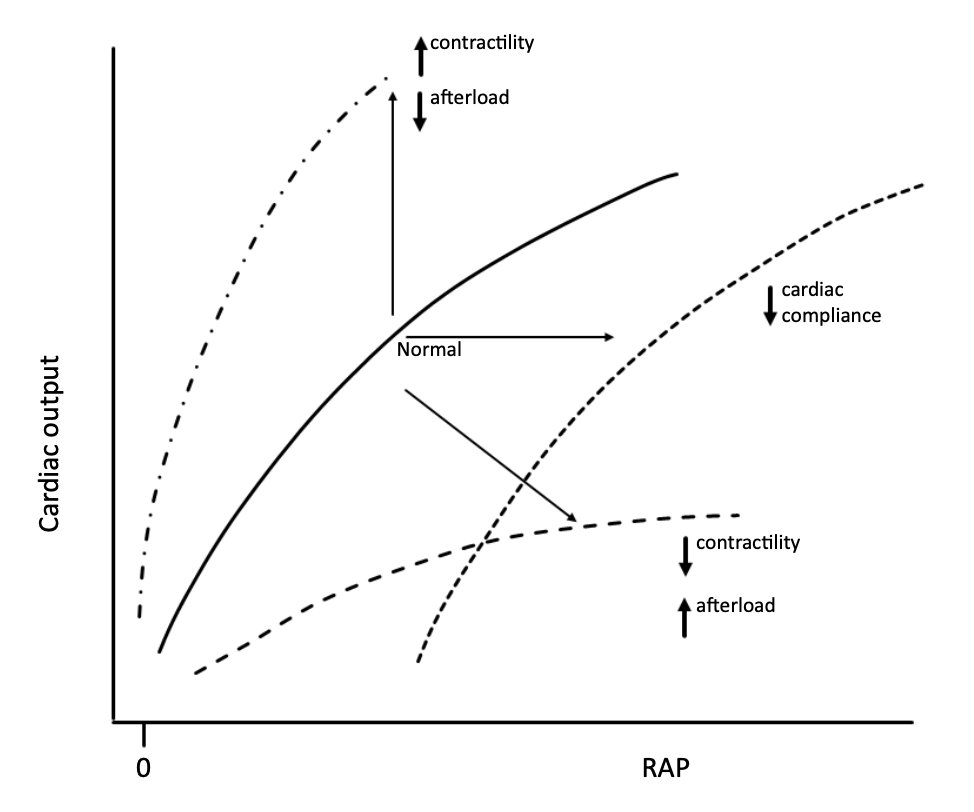
 2/
2/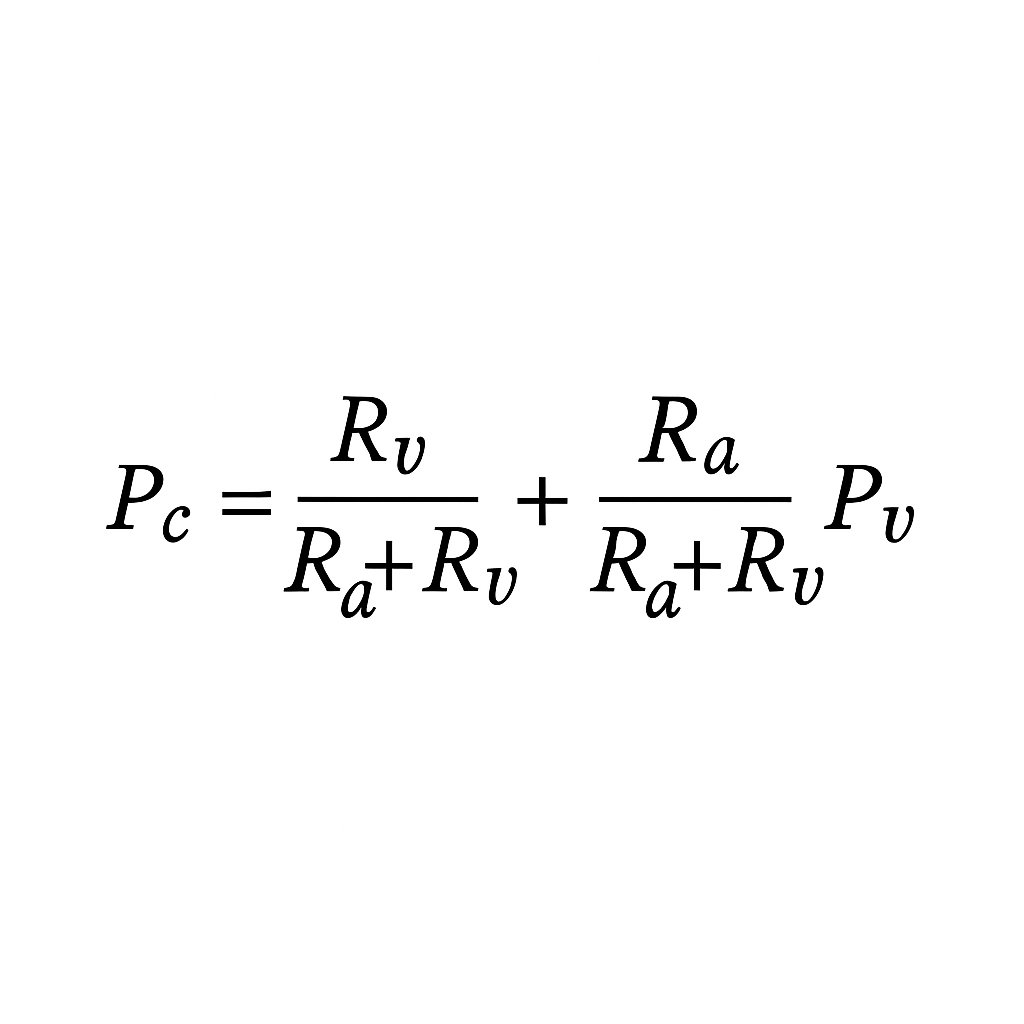
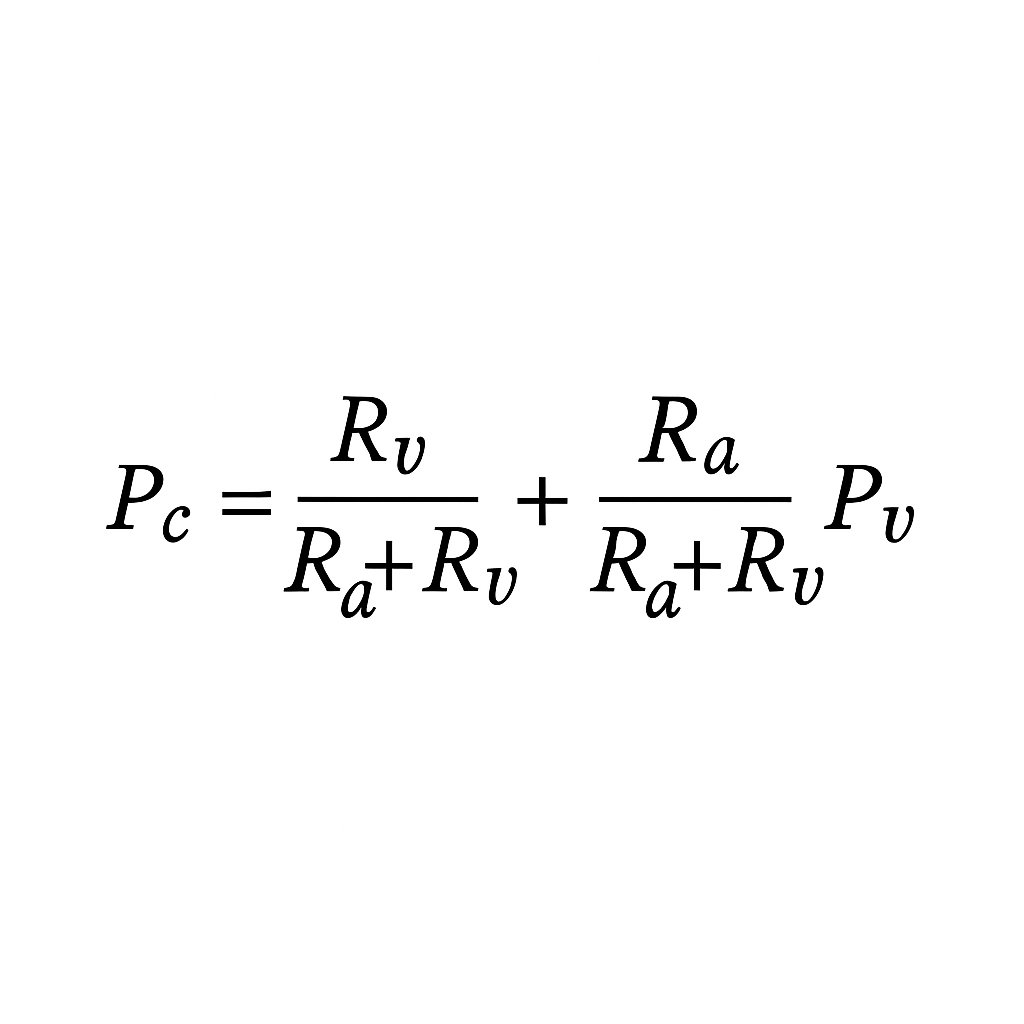
https://twitter.com/NephroP/status/1974492082916962714Venous congestion ↑RAP → ↑venous pressure (Pv) → potentially ↑capillary pressure (Pc).

 2/
2/
 2. Heterogeneity (noise, even in “real” diseases)
2. Heterogeneity (noise, even in “real” diseases)
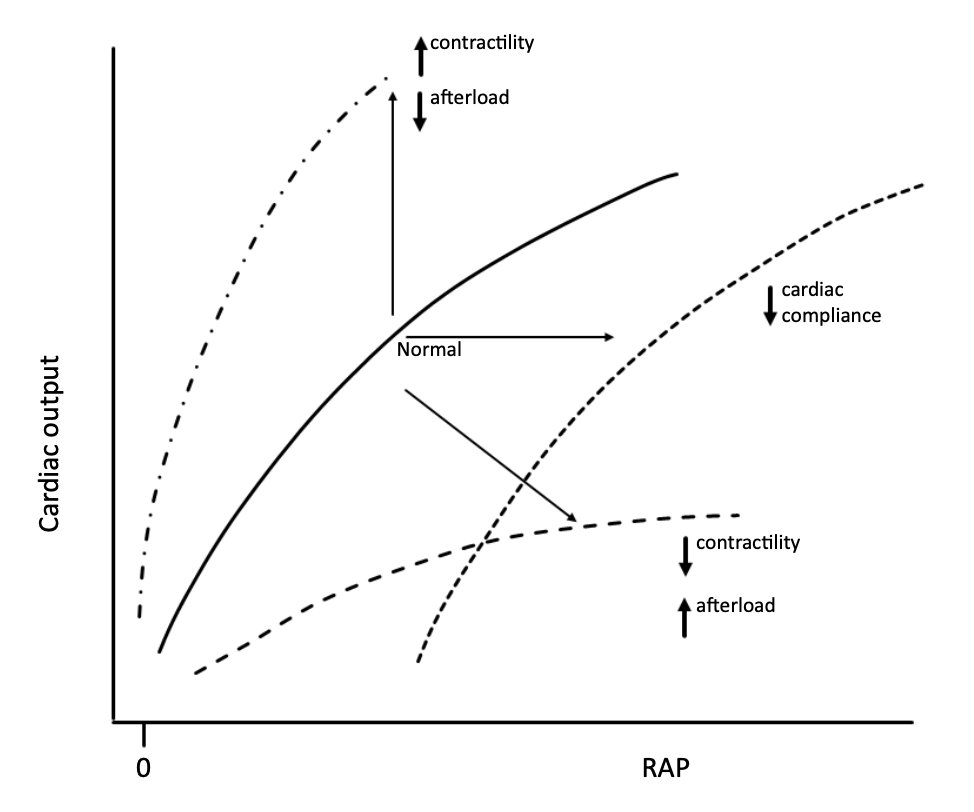
https://twitter.com/icmteaching/status/19567518386669529712/