Since the nonsense yesterday when a public health body erroneously stated that 80% of infections diseases are spread by contact....
I promised a thread....
Lets start with the @WHO Hand hygiene guideline
@LazarusLong13
I promised a thread....
Lets start with the @WHO Hand hygiene guideline
@LazarusLong13
In Section 9 of WHO HH guideline the relationship of HCAI and hospital pathogens is revealed
2 assertions are made
A) Semmelweis used an antiseptic and it reduced puerperal fever.
B) Substantial evidence for hand antisepsis reducing HCAI is contained in citations 58, 179, 180
2 assertions are made
A) Semmelweis used an antiseptic and it reduced puerperal fever.
B) Substantial evidence for hand antisepsis reducing HCAI is contained in citations 58, 179, 180

Assertion A
Semmelweis did not use nor recommend an antiseptic. He recommended and used a disinfectant. Excerpt from his univ web site.
The procedure reduced PF but was intolerable & burnt HCWs' skin.
NB IS knew it was coming from the PM room and should have stopped PM visits
Semmelweis did not use nor recommend an antiseptic. He recommended and used a disinfectant. Excerpt from his univ web site.
The procedure reduced PF but was intolerable & burnt HCWs' skin.
NB IS knew it was coming from the PM room and should have stopped PM visits

Oliver Wendall Holmes had recommended NEVER to do post mortems and midwifery - 4-years before Semmelweis started in Vienna.
NB Semmelweis was behind on his reading!
NB Semmelweis was behind on his reading!

Semmelweis recommended the wrong control measure (disinfection) and not the correct one - stop PM room visits by doctors. Thus the WHO in their 2009 guidance got their first assertion wrong.
It was not an antiseptic - it was an intolerable to use in the long term disinfectant.
It was not an antiseptic - it was an intolerable to use in the long term disinfectant.
Well that is convenient because the WHO cites 58, 179 & 180 and 179 & 180 just happen to be the same 2 citations included in the WHOs citation 58 as 66 and 67 



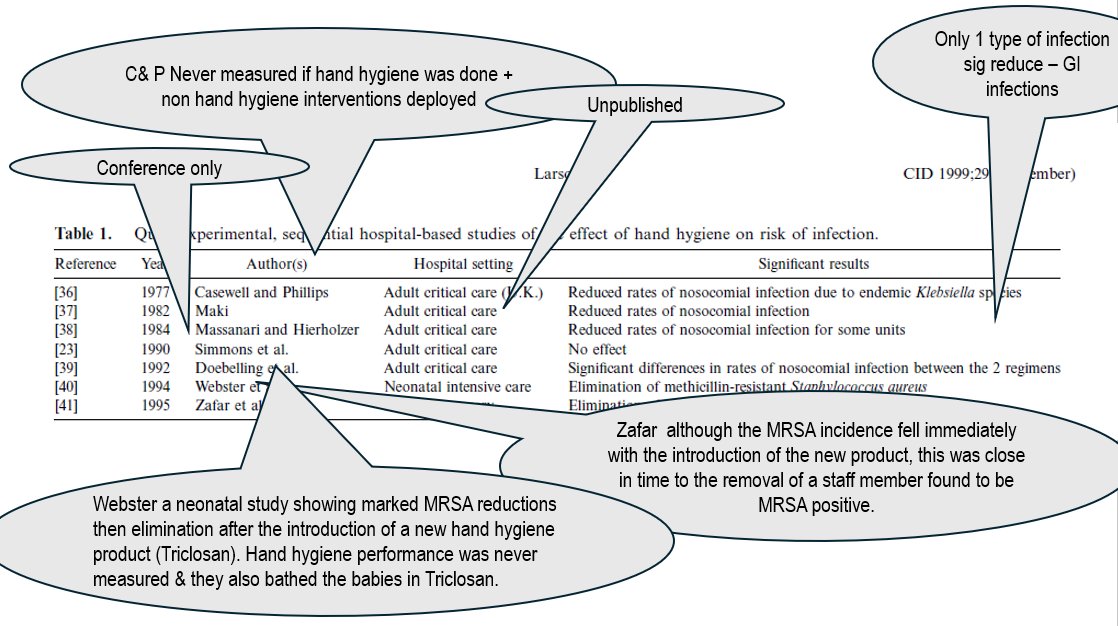
Well here is the Larson 1988 paper - I am not bowled over or drowning in evidence here
179 / 66 citation numbers
179 / 66 citation numbers

I am still looking for evidence that HH is the single most important measure to prevent HAI.
Clearly Pneumonia are not caused by HH, SSIs are the patient's own flora entering to infect via the air... UTI own flora, etc. etc.
Clearly Pneumonia are not caused by HH, SSIs are the patient's own flora entering to infect via the air... UTI own flora, etc. etc.
Pathogens are released in bursts into the air....
Enough with overstating the impact of hand hygiene. Is it important yes! But at least as important are the pathogens travelling via the air.
Enough with overstating the impact of hand hygiene. Is it important yes! But at least as important are the pathogens travelling via the air.

• • •
Missing some Tweet in this thread? You can try to
force a refresh