3rd Long COVID International Conference 2025
🧵below
🧵below
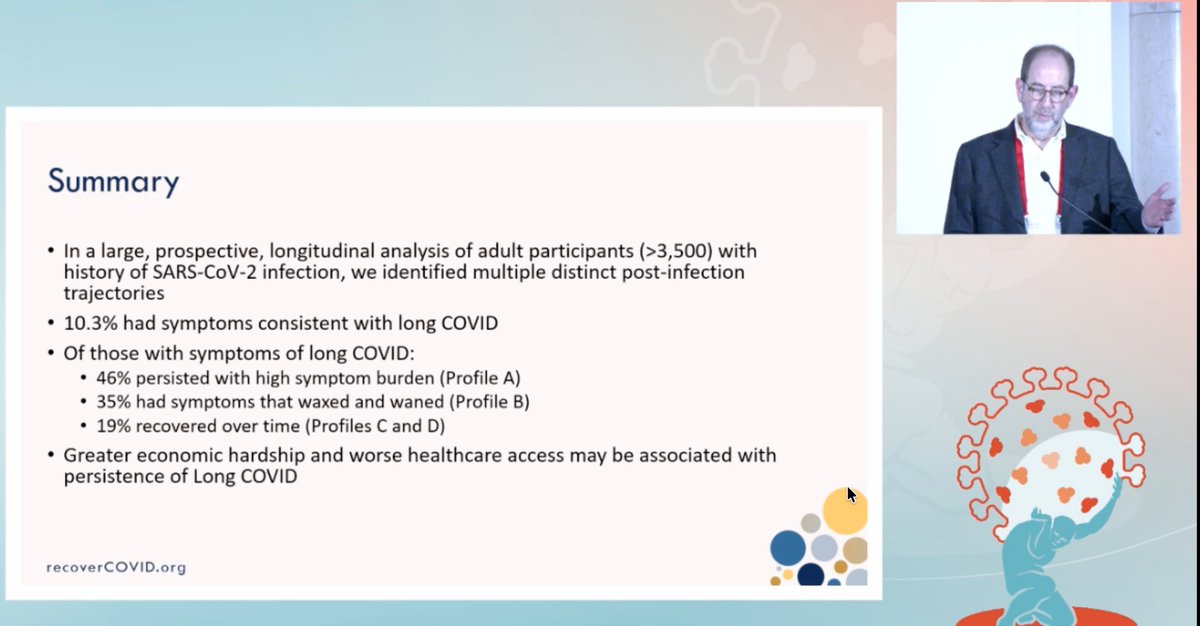
In a study of over 3,500 adults with past COVID, NIH researchers found 10.3% had long COVID symptoms.
Of those, 46% had lasting symptoms, 35% had ups and downs, and 19% recovered.
Economic hardship may raise the risk of symptoms persisting.
Of those, 46% had lasting symptoms, 35% had ups and downs, and 19% recovered.
Economic hardship may raise the risk of symptoms persisting.
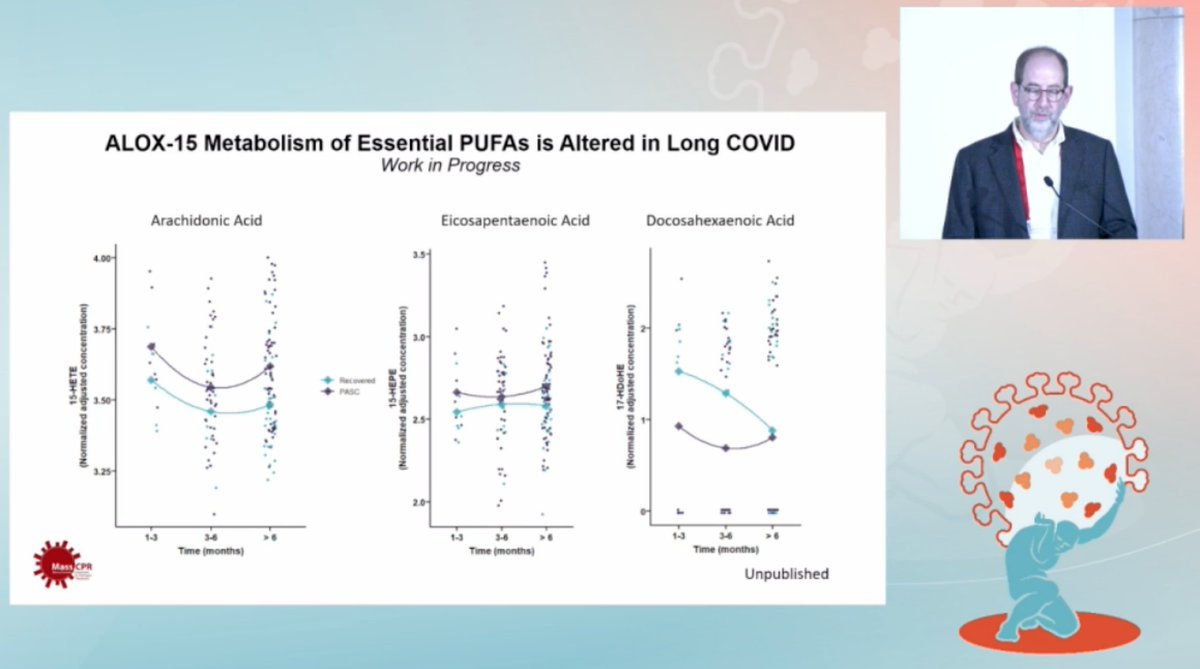
Researchers found that people with long COVID show disrupted metabolism of essential fatty acids for at least 6 months, including arachidonic acid and DHA.
These pathways help control inflammation and recovery.
These pathways help control inflammation and recovery.
The Office of Long COVID Research will close by March 2025 with no plan to replace it.
Federal studies continue across NIH, VA, DoD, and CDC, but clinical care pilots have mostly expired.
Congress has yet to act on new bills.
Federal studies continue across NIH, VA, DoD, and CDC, but clinical care pilots have mostly expired.
Congress has yet to act on new bills.

CDC data suggest at least 44 million people in the US have had Long Covid.
Globally, estimates point to over 400 million cases by 2023, rising sharply from 65 million in 2020.
Globally, estimates point to over 400 million cases by 2023, rising sharply from 65 million in 2020.

From VA data on 20,297 patients hospitalized with COVID, excess deaths remained elevated even 3 years later.
In a broader N3C sample of over 3 million, risk of death stayed 19% to 26% higher after acute infection.
In a broader N3C sample of over 3 million, risk of death stayed 19% to 26% higher after acute infection.

Long COVID remains a massive burden with deep personal, economic and societal costs.
Data suggest vaccines and some drugs can lower risk, yet US policy lags behind.
Prevention must become a global priority.
"Any sane world must say this must be a global priority"
Data suggest vaccines and some drugs can lower risk, yet US policy lags behind.
Prevention must become a global priority.
"Any sane world must say this must be a global priority"

Researchers estimate that 2–10% of children infected with COVID may develop long-term symptoms.
With 65 million US children antibody positive, at least 1.3 million could have long COVID, more than those with epilepsy or cancer.
With 65 million US children antibody positive, at least 1.3 million could have long COVID, more than those with epilepsy or cancer.

The NIH RECOVER study aims to uncover how long COVID works, define its subtypes, predict who’s most at risk, and find treatment targets by linking systems biology to patient outcomes. 

Five years into the pandemic, there are still no approved treatments for Long COVID in children.
Researchers say trials must target both symptoms and root causes and adapt to relapsing patterns seen in some kids.
Researchers say trials must target both symptoms and root causes and adapt to relapsing patterns seen in some kids.

Researchers aim to track how well antiviral treatments work by measuring spike proteins in blood, viral RNA, and inflammation.
They also look at how often patients visit hospitals or clinics during the study.
They also look at how often patients visit hospitals or clinics during the study.

RECOVER-VITAL to be published by the end of the year.
Evidence of viral persistence, inflammation, etc.
Evidence of viral persistence, inflammation, etc.

Researchers are tracking how long COVID symptoms change over time and whether antiviral drugs help some patients recover, especially those with signs of ongoing infection.
Placebo data may reveal how organ dysfunction unfolds without treatment.
Placebo data may reveal how organ dysfunction unfolds without treatment.

Sustained effect for Metformin. Would you use Metformin if you had acute covid and why is this not in the guidelines? - Steve Deeks 

"We can't even get Paxlovid to patients and providers/insurance/FDA/etc can't figure out policy"
"Secondary endpoint was impressive, but sadly the primary endpoint put it in trouble"
"Secondary endpoint was impressive, but sadly the primary endpoint put it in trouble"

Our group is looking in depth at metabolics of parent fatty acids and there are some differences of how they are being metabolized.
The question would be could you even supplement the parent and figure out interventions once the issues are defined.
The question would be could you even supplement the parent and figure out interventions once the issues are defined.

Researchers found SARS-CoV-2 RNA in the colon up to 992 days after infection.
Signals from both spike and orf1ab RNA suggest the virus may linger in gut tissue far longer than expected.
Signals from both spike and orf1ab RNA suggest the virus may linger in gut tissue far longer than expected.

Researchers found major differences in gut gene activity between people with long COVID and those who recovered.
Key immune genes were dialed down in long COVID, suggesting persistent gut immune disruption.
Key immune genes were dialed down in long COVID, suggesting persistent gut immune disruption.

The INTERRUPT-LC trial is testing Anktiva, a drug that boosts IL-15 to help immune cells better target lingering infection in long COVID.
It aims to restore natural killer and T cell activity to clear viral reservoirs.
It aims to restore natural killer and T cell activity to clear viral reservoirs.

Researchers found SARS-CoV-2 RNA in 2 of 6 bone marrow biopsies from long COVID patients, but saw no viral RNA in acute cases and no clear protein persistence.
This suggests possible viral RNA traces without lasting protein in some LC cases.
This suggests possible viral RNA traces without lasting protein in some LC cases.

Researchers identified gene clusters in long COVID patients linked to antiviral defenses, including interferon signaling, antigen presentation, NK cell recognition, RNA sensing, and cell differentiation. 

UCSF researchers found higher immune activation in the gut and brain of people with long COVID.
PET scans showed increased [¹⁸F]F-AraG uptake in the rectosigmoid wall and olfactory regions, pointing to lingering inflammation.
PET scans showed increased [¹⁸F]F-AraG uptake in the rectosigmoid wall and olfactory regions, pointing to lingering inflammation.

Researchers show that RNAscope ISH is the most sensitive tool for detecting SARS-CoV-2 in tissue.
It identifies viral RNA and spike protein, even in low levels, using color-coded markers in infected cells.
It identifies viral RNA and spike protein, even in low levels, using color-coded markers in infected cells.

Researchers found SARS-CoV-2 RNA can persist at low levels in the gut in some Long COVID cases.
The gut’s reduced antiviral gene activity may allow this, pointing to immune-boosting as a possible treatment route.
The gut’s reduced antiviral gene activity may allow this, pointing to immune-boosting as a possible treatment route.

Scientists found spike or nucleocapsid antigens in only a few Long COVID and control cases up to 18 months.
No link to symptoms was found.
DTT may distort results and should be used cautiously in spike antigen studies.
No link to symptoms was found.
DTT may distort results and should be used cautiously in spike antigen studies.

Researchers analyzed plasma from 110 Long COVID patients and used machine learning to identify a predictive biomarker signature based on metabolites, cytokines and clinical data.
A diagnostic patent is underway.
A diagnostic patent is underway.

Researchers found Long COVID patients show strong platelet and neutrophil activation, low G-CSF, and high IL-10.
Elevated GDF-15 points to mitochondrial stress.
Findings suggest lasting inflammation and clotting risk in tissue.
Elevated GDF-15 points to mitochondrial stress.
Findings suggest lasting inflammation and clotting risk in tissue.

Researchers found Long COVID patients show disrupted energy metabolism with buildup of lactic acid and glutamate.
This points to defects in glycolysis and fat oxidation, along with altered lipid profiles.
This points to defects in glycolysis and fat oxidation, along with altered lipid profiles.

Researchers found that Long COVID patients have a distinct immune and metabolic signature in blood.
Even those who recovered show unique patterns, separating them from both Long COVID and uninfected individuals.
Even those who recovered show unique patterns, separating them from both Long COVID and uninfected individuals.

Researchers identified top biomolecules that best distinguish Long COVID from controls using machine learning.
Markers like GDF-15 and CRP showed high accuracy, supporting their use in future diagnostic tests.
Markers like GDF-15 and CRP showed high accuracy, supporting their use in future diagnostic tests.

Researchers propose that in Long COVID, poor immune response and metabolic dysfunction fuel each other.
This cycle drives inflammation, vascular damage, viral persistence and mitochondrial stress, keeping symptoms going.
This cycle drives inflammation, vascular damage, viral persistence and mitochondrial stress, keeping symptoms going.

Researchers show how early infections raise later disease risk.
Chickenpox can lead to shingles, influenza to narcolepsy, EBV to MS, strep to rheumatic fever, HIV to cancers and HPV to cervical cancer.
Chickenpox can lead to shingles, influenza to narcolepsy, EBV to MS, strep to rheumatic fever, HIV to cancers and HPV to cervical cancer.

Researchers at FIMM found that genes linked to lung and immune function also show up in fibromyalgia and ME/CFS.
Global COVID studies may unlock clues to post-viral illness and better prepare us for future pandemics.
Global COVID studies may unlock clues to post-viral illness and better prepare us for future pandemics.

Researchers found that people with Long COVID show weaker antibody responses, poor antibody class switching and faster antibody decline.
These signs point to an immature immune response that may underlie lasting symptoms.
These signs point to an immature immune response that may underlie lasting symptoms.

"How do you go about viral persistence skepticism"
Tim: "We see it, right? Viruses persist in tissues when you look deep"
Tim: "It's there, we're seeing it, but the direct relationship is what we're trying to figure out"
Tim: "We see it, right? Viruses persist in tissues when you look deep"
Tim: "It's there, we're seeing it, but the direct relationship is what we're trying to figure out"

"Is rapamycin a potential combination for treatment based on tissue based disorder?"
Tim: "mTOR is super interesting and already being studied in trials"
Tim: "Lots of mechanisms of action, we need to choose participants correctly"
Tim: "mTOR is super interesting and already being studied in trials"
Tim: "Lots of mechanisms of action, we need to choose participants correctly"

"What data do you have regarding dsRNA and ssRNA?"
"It is possible we are detecting multiple forms. Probes are aimed to it, but can have off target effects. We need to develop this out further."
"It is possible we are detecting multiple forms. Probes are aimed to it, but can have off target effects. We need to develop this out further."
"Is the converse true about GI symptoms and viral persistence?"
No super strong correlation of clinical phenotypes. Broad distribution
No super strong correlation of clinical phenotypes. Broad distribution

"Do you have stool samples for your gut persistence work?"
"Sadly no, but we do now for upcoming trials!"
"Sadly no, but we do now for upcoming trials!"

@patrickc you might find this interesting.
Researchers found widespread T cell gene dysregulation in ME/CFS, with both upregulated and downregulated genes across immune cell types.
The strongest changes were seen in CD8, MAIT and Tγδ cells, pointing to deep immune disruption.
The strongest changes were seen in CD8, MAIT and Tγδ cells, pointing to deep immune disruption.

Scientists found that CD8+ T cells in ME/CFS show major gene changes, especially in more differentiated cells.
Key regulators like TCF7 and TBX21 are altered, pointing to disrupted immune memory and response.
Key regulators like TCF7 and TBX21 are altered, pointing to disrupted immune memory and response.

Researchers report that people with ME show clear immune system changes including dysregulated monocytes and exhausted CD8+ T cells, suggesting the disease may behave like a chronic viral infection. 

Yale researchers found reduced gray matter in brain areas tied to language, memory, and sensory processing in some patients.
Cognitive symptoms were linked to reduced blood flow in frontal, temporal, and parietal lobes.
Cognitive symptoms were linked to reduced blood flow in frontal, temporal, and parietal lobes.

Researchers found the Th17 immune response is disrupted in most long COVID types, linking IL-17 imbalances to lung damage and chronic inflammation.
These shifts were not seen in patients with mainly sensory symptoms.
These shifts were not seen in patients with mainly sensory symptoms.

Scientists found that immune profiles stayed abnormal for up to 24 months in long COVID.
Unique cytokine patterns linked to symptoms like fatigue and pain suggest different disease types needing personalized treatment.
Unique cytokine patterns linked to symptoms like fatigue and pain suggest different disease types needing personalized treatment.

Researchers link POLG gene variants to long COVID.
Mutations disrupt mitochondrial DNA repair and energy production, leading to fatigue, exercise intolerance and neurological symptoms.
Mutations disrupt mitochondrial DNA repair and energy production, leading to fatigue, exercise intolerance and neurological symptoms.

Children’s Hospital Los Angeles plans to study DNA methylation to understand why only some people with gene variants like POLG or MEFV develop long COVID.
The goal is to find risk markers and new treatment targets.
The goal is to find risk markers and new treatment targets.

Scientists find that long COVID causes deep and lasting disruptions to T cell function for over 1.5 years.
These include altered helper and killer T cells and widespread immune imbalances, pointing to new targets for treatment and monitoring.
These include altered helper and killer T cells and widespread immune imbalances, pointing to new targets for treatment and monitoring.

HIV was a lot like Long COVID is now. In 1994, viral load measurement was validated for HIV severity and who to treat. 20 companies invested billions of dollars in these drugs. Patients got better. 

"Asked about the best biomarker."
Steve says: Start with the virus. We find its fragments everywhere, and that’s where the answers live.
Jim adds: Specificity matters, and the virus is nothing if not specific. Virus keeps passing through too, COVID is still around.
Steve says: Start with the virus. We find its fragments everywhere, and that’s where the answers live.
Jim adds: Specificity matters, and the virus is nothing if not specific. Virus keeps passing through too, COVID is still around.

Johan notes: That in TB and coagulation work, we’ve already learned how to use ROC curves and solid assay standards to create reliable surrogate markers.
Maybe those lessons can guide how we judge biomarkers here too.
Maybe those lessons can guide how we judge biomarkers here too.

The virus hides in tissue, not blood like HIV. Maybe we can develop a biomarker like in bone marrow or somewhere else. Not sure if we can do a biomarker for that.
It will end up with combination, not just virus. Strongest signal in tissues. Virus persists in organs across body.
It will end up with combination, not just virus. Strongest signal in tissues. Virus persists in organs across body.

We haven't systemically looked at all tissues yet. We need to. 10% in liver, 10% in brain, persistence somewhere?! We need to look at the tissues.
For those who know me I'm an autopsy pathologist, it's easier for me to do than for clinicians to do
*audience laugh*
For those who know me I'm an autopsy pathologist, it's easier for me to do than for clinicians to do
*audience laugh*

Posting a few posters that looked interesting to me now.
At Institut Fournier in Paris, 19 long COVID patients with severe GI symptoms took maraviroc and pravastatin.
After 3 months, 78% showed major improvement, linked to fewer blood microclots and less viral material in platelets
After 3 months, 78% showed major improvement, linked to fewer blood microclots and less viral material in platelets
NIH researchers found that IVO-21, a new oral drug, stabilizes mitochondria and calms thromboinflammation in mice.
It may safely treat the metabolic and vascular damage seen in long COVID.
It may safely treat the metabolic and vascular damage seen in long COVID.
Sheffield Hallam University studied 39 people with Long COVID and found that those who took a daily multi-strain probiotic for 12 weeks showed significant improvements in memory, planning and gut symptoms compared to placebo
Rutgers researchers studied 3,251 kids and found that high anti-nucleocapsid antibody levels were linked to more long COVID symptoms in children aged 6 to 11 but not in teens.
This points to age-specific immune responses to the virus
This points to age-specific immune responses to the virus
Barcelona researchers studied over 190,000 people and found that chronic antihistamine use was linked to fewer cases of Long COVID and fewer blood clots after repeated infections.
No Long COVID was seen in users with three infections.
No Long COVID was seen in users with three infections.
Stanford researchers studied 123 people and found that Long COVID and ME/CFS share changes in immune cell-derived extracellular vesicles, including mitochondrial enrichment, suggesting a shared disease mechanism and potential biomarkers.
Genclis researchers studied 82 people and found that in Long COVID, infectious SARS-CoV-2 can be reactivated in lab cells via a fatty acid pathway using the LSR receptor, bypassing ACE2 and evading existing antibodies.
University of Liège doctors used AI and imaging to find five types of biomarkers in two patients with long COVID. These include language, brain scans, gene activity, neural signals, and viral traces. The approach is expanding to 300 more patients.
At UCSF, among 693 COVID-19 survivors, cytokines predicted long COVID best in obese patients.
IL-6 and IL-1β drove inflammation, were reduced by GLP-1 drugs, and linked to risk.
In healthy-weight people, these immune signals were weaker or absent.
IL-6 and IL-1β drove inflammation, were reduced by GLP-1 drugs, and linked to risk.
In healthy-weight people, these immune signals were weaker or absent.
@SalvMattera here you go dude
University of Minnesota researchers found higher blood levels of endotrophin in people with Long COVID, even after adjusting for body weight. This protein may become a useful biomarker for identifying Long COVID.
At Children’s National Hospital, 3 teens with Long COVID were treated with IVIG every few weeks for 6 months.
All showed symptom relief within 2 to 3 weeks and improved school attendance, despite early side effects like nausea and headaches.
All showed symptom relief within 2 to 3 weeks and improved school attendance, despite early side effects like nausea and headaches.
University of Luxembourg researchers surveyed 198 doctors across 31 countries and found only 13% routinely ask about sexual dysfunction in Long Covid patients.
Just 10% use validated tools to assess it.
Just 10% use validated tools to assess it.
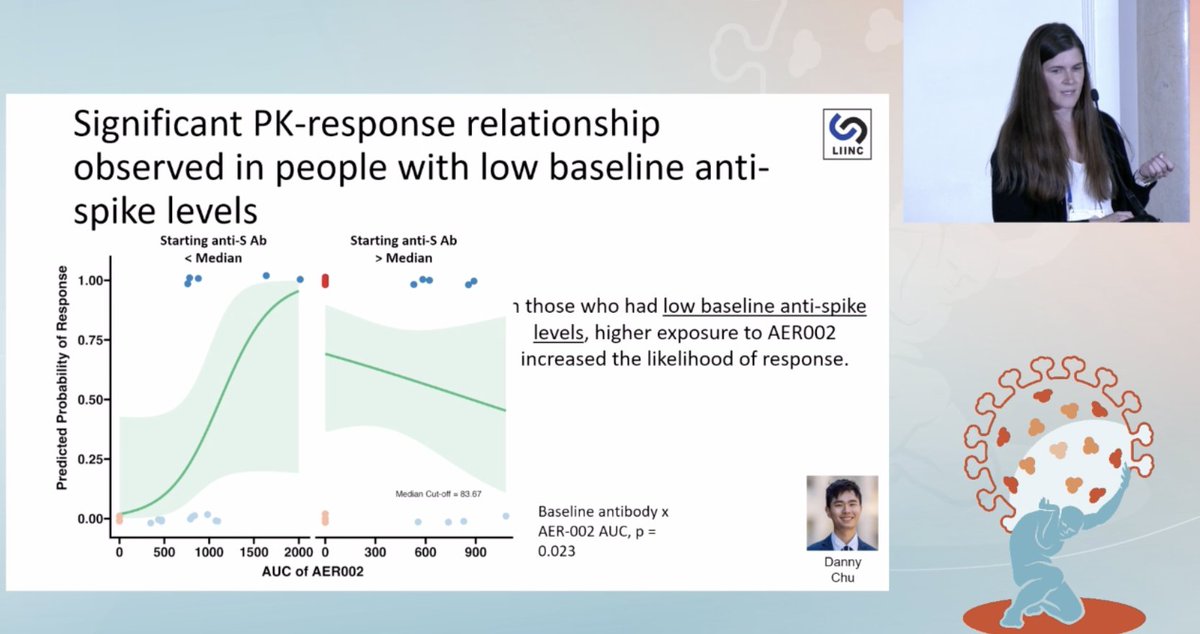
UCSF researchers found that people with low baseline anti-spike antibodies were more likely to respond to AER002 when exposed to higher drug levels, with a significant PK-response relationship seen only in this group. 
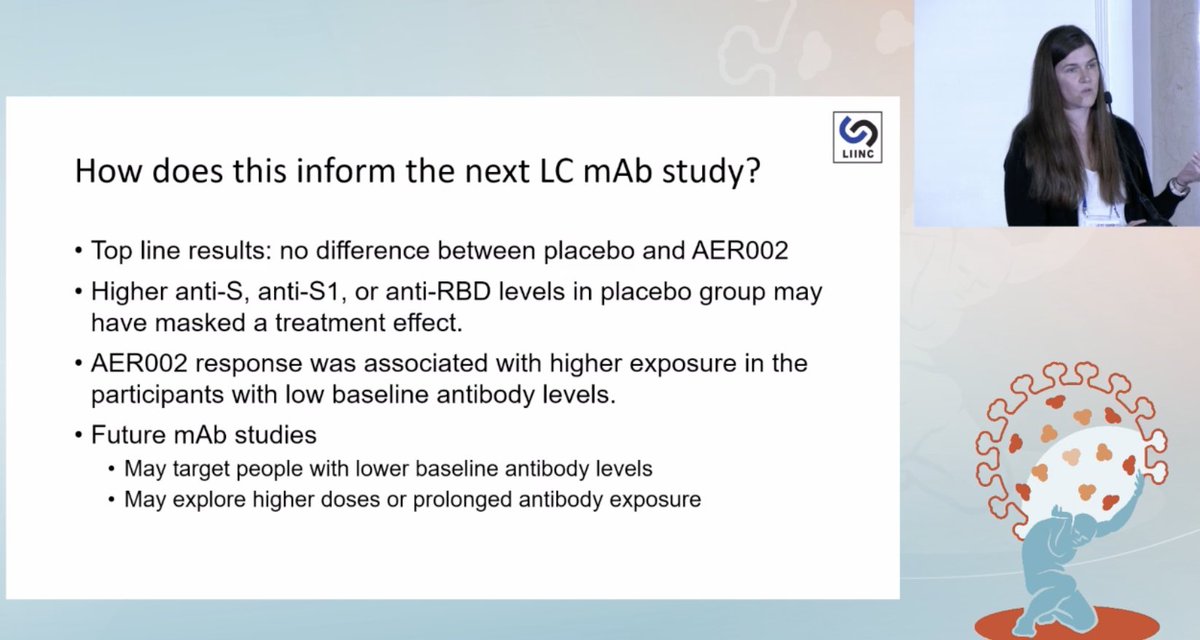
UCSF researchers found no overall difference between placebo and AER002 but suggest high baseline antibodies in the placebo group may have masked effects.
Future trials may focus on those with low antibody levels or use higher dosing.
Future trials may focus on those with low antibody levels or use higher dosing.
In a study of 778 adults with long‑COVID (~192–197 per arm) researchers found that all three drug interventions improved quality of life scores (EQ‑5D‑5L) more than usual care by 12 weeks, although gains plateaued by 24 weeks. 

• • •
Missing some Tweet in this thread? You can try to
force a refresh














