Astrocyte-Mediated Hippocampal Damage in the Pathogenesis of Dysexecutive Syndrome Following COVID-19: A Narrative Review.
🔥Another interesting review study from Italy: Hippocampal dysfunction post C19!
➡️"SARS-CoV-2 infection has been implicated in hippocampal damage, contributing to the pathogenesis of dysexecutive syndrome observed in post-COVID-19 patients."
➡️"Given the growing prevalence of long-COVID worldwide, understanding how SARS-CoV-2 affects hippocampal structure and function has become an urgent scientific and clinical priority."
➡️"The hippocampus—crucial for memory, emotional regulation, and executive functioning—is especially susceptible to viral-driven neuroinflammatory cascades."
➡️"SARS-CoV-2 triggers astrocyte and microglia activation, disrupts blood–brain barrier integrity, and induces cytokine-mediated neurotoxicity, ultimately impairing neuroplasticity and neurogenesis."
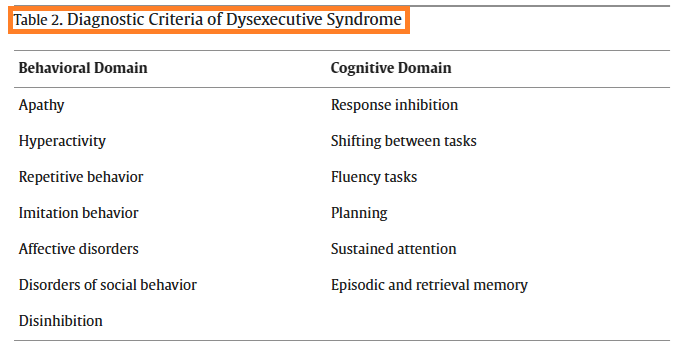
➡️"These mechanisms converge to produce cognitive and affective disturbances—most notably fatigue, apathy, low mood, and executive dysfunction—that typify dysexecutive syndrome in long-COVID."
➡️Review Key Points:
1. SARS-CoV-2 triggers astrocyte/microglia activation → hippocampal damage via cytokines and BBB disruption.
2. Leads to impaired neurogenesis/plasticity and dysexecutive symptoms (fatigue, apathy, executive dysfunction).
3. Neuroinflammation-driven "depression" differs from primary psychiatric disorders.
4. Vaccination provides neuroprotection against these mechanisms.
5. Calls for anti-inflammatory therapies, cognitive rehab, and long-term research.
➡️"The evidence reviewed indicates that SARS-CoV-2 infection may precipitate hippocampal dysfunction through a convergence of astrocytic infection, microglial activation, blood–brain barrier disruption, and impaired neurogenesis."
➡️"These mechanisms provide a biologically plausible framework for understanding the dysexecutive phenotype frequently observed in post-COVID-19 patients — characterized by fatigue, apathy, motivational decline, and cognitive inefficiency rather than purely affective disturbance."
➡️"Recognizing the hippocampal–glial contribution to these symptoms has direct diagnostic and therapeutic implications."
➡️‼️"Clinicians should be attentive to executive and motivational deficits in post-COVID-19 presentations and avoid attributing them solely to primary depressive disorders."
➡️"These findings reinforce the view that the hippocampus represents a critical interface between immune activation and cognitive-affective regulation in COVID-19, and that protecting its structural and functional integrity should be regarded as a key objective in the clinical management of affected patients."
So, SARS-CoV-2's insidious assault on the brain, via astrocyte-driven neuroinflammation and hippocampal destruction, unleashes a disturbing dysexecutive syndrome—marked by fatigue, apathy, and cognitive impairment—that persists long after the virus clears, masquerading as depression while eroding memory, executive function, and quality of life in millions of post-COVID survivors!
Add now the possible cumulative reinfection impact?
sciencedirect.com/science/articl…
🔥Another interesting review study from Italy: Hippocampal dysfunction post C19!
➡️"SARS-CoV-2 infection has been implicated in hippocampal damage, contributing to the pathogenesis of dysexecutive syndrome observed in post-COVID-19 patients."
➡️"Given the growing prevalence of long-COVID worldwide, understanding how SARS-CoV-2 affects hippocampal structure and function has become an urgent scientific and clinical priority."
➡️"The hippocampus—crucial for memory, emotional regulation, and executive functioning—is especially susceptible to viral-driven neuroinflammatory cascades."
➡️"SARS-CoV-2 triggers astrocyte and microglia activation, disrupts blood–brain barrier integrity, and induces cytokine-mediated neurotoxicity, ultimately impairing neuroplasticity and neurogenesis."
➡️"These mechanisms converge to produce cognitive and affective disturbances—most notably fatigue, apathy, low mood, and executive dysfunction—that typify dysexecutive syndrome in long-COVID."
➡️Review Key Points:
1. SARS-CoV-2 triggers astrocyte/microglia activation → hippocampal damage via cytokines and BBB disruption.
2. Leads to impaired neurogenesis/plasticity and dysexecutive symptoms (fatigue, apathy, executive dysfunction).
3. Neuroinflammation-driven "depression" differs from primary psychiatric disorders.
4. Vaccination provides neuroprotection against these mechanisms.
5. Calls for anti-inflammatory therapies, cognitive rehab, and long-term research.
➡️"The evidence reviewed indicates that SARS-CoV-2 infection may precipitate hippocampal dysfunction through a convergence of astrocytic infection, microglial activation, blood–brain barrier disruption, and impaired neurogenesis."
➡️"These mechanisms provide a biologically plausible framework for understanding the dysexecutive phenotype frequently observed in post-COVID-19 patients — characterized by fatigue, apathy, motivational decline, and cognitive inefficiency rather than purely affective disturbance."
➡️"Recognizing the hippocampal–glial contribution to these symptoms has direct diagnostic and therapeutic implications."
➡️‼️"Clinicians should be attentive to executive and motivational deficits in post-COVID-19 presentations and avoid attributing them solely to primary depressive disorders."
➡️"These findings reinforce the view that the hippocampus represents a critical interface between immune activation and cognitive-affective regulation in COVID-19, and that protecting its structural and functional integrity should be regarded as a key objective in the clinical management of affected patients."
So, SARS-CoV-2's insidious assault on the brain, via astrocyte-driven neuroinflammation and hippocampal destruction, unleashes a disturbing dysexecutive syndrome—marked by fatigue, apathy, and cognitive impairment—that persists long after the virus clears, masquerading as depression while eroding memory, executive function, and quality of life in millions of post-COVID survivors!
Add now the possible cumulative reinfection impact?
sciencedirect.com/science/articl…
• • •
Missing some Tweet in this thread? You can try to
force a refresh