Persistent Immune Dysregulation during Long COVID is Manifested in Antibodies Targeting Envelope and Nucleocapsid Proteins
🔥YOUR ATTENTION, VERY INTERESTING AND IMPORTANT USA PREPRINT! #LEONARDI_EFFECT
Long COVID is characterized by persistent, profound immune dysregulation, including skewed antibodies, chronically activated T cells, elevated inflammation, and autoreactive responses, lasting at least six months and consistent with ongoing viral/antigen persistence.
➡️Let me try to dig into this study:
1. Persistent antibody skewing in Long COVID (LC):
- Participants with LC show elevated IgG titers against SARS-CoV-2 Envelope and Nucleocapsid proteins lasting up to 6 months post-infection, unlike convalescents.
- In contrast, IgG responses to Spike protein are significantly lower, with a bias toward IgG1 and IgG3 subclasses.
2. Cellular immune alterations:
- Longitudinal CyTOF profiling reveals increased circulating T follicular helper cells (cTFH) and mucosa-associated invariant T (MAIT) cells in LC, correlating strongly with high anti-Envelope IgG levels.
3. Systemic inflammation and cytokines:
- LC is associated with augmented serum levels of LIF, IL-11, Eotaxin-3, and HMGB-1, indicating ONGOING IMMUNE ACTIVATION!
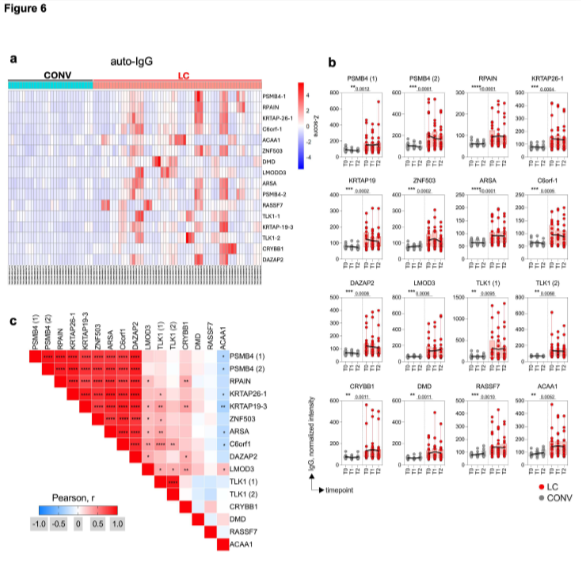
4. Autoreactivity:
- Significantly higher rates of autoantibodies in LC compared to recovered individuals, pointing to BROADER IMMUNE DYSREGULATION.
5. Duration/ Implications:
- These humoral, cellular, and molecular perturbations persist for at least 6 months, supporting hypotheses of viral/antigenic persistence (possibly mucosal), dysregulated antibody production, and autoimmunity as drivers of diverse LC phenotypes.
6. Clinical relevance:
- The findings highlight the need for targeted therapies addressing persistent viral elements, aberrant humoral responses, and autoimmunity, and emphasize longitudinal immune profiling for diagnostics and therapeutic monitoring in Long COVID.
7. Limitations:
- The study does not mention reinfections, multiple infections, breakthrough infections, or specific SARS-CoV-2 variants (such as Delta or Omicron), or any vaccination related factors, it’s solely focused on LC patients!
‼️So, for those still in doubt, if that's even possible, this study proves unambiguously the #Leonardi_effect, showing Long COVID involves PERSISTENT, SEVERE IMMUNE DYSREGULATION, skewed IgG against Envelope/Nucleocapsid, chronically activated T cells, sustained inflammation, and autoimmunity, lasting ≥6 months, here pointing to ongoing viral/antigenic persistence! #AVOIDSARS2
FYI: @fitterhappierAJ
researchsquare.com/article/rs-830…
🔥YOUR ATTENTION, VERY INTERESTING AND IMPORTANT USA PREPRINT! #LEONARDI_EFFECT
Long COVID is characterized by persistent, profound immune dysregulation, including skewed antibodies, chronically activated T cells, elevated inflammation, and autoreactive responses, lasting at least six months and consistent with ongoing viral/antigen persistence.
➡️Let me try to dig into this study:
1. Persistent antibody skewing in Long COVID (LC):
- Participants with LC show elevated IgG titers against SARS-CoV-2 Envelope and Nucleocapsid proteins lasting up to 6 months post-infection, unlike convalescents.
- In contrast, IgG responses to Spike protein are significantly lower, with a bias toward IgG1 and IgG3 subclasses.
2. Cellular immune alterations:
- Longitudinal CyTOF profiling reveals increased circulating T follicular helper cells (cTFH) and mucosa-associated invariant T (MAIT) cells in LC, correlating strongly with high anti-Envelope IgG levels.
3. Systemic inflammation and cytokines:
- LC is associated with augmented serum levels of LIF, IL-11, Eotaxin-3, and HMGB-1, indicating ONGOING IMMUNE ACTIVATION!
4. Autoreactivity:
- Significantly higher rates of autoantibodies in LC compared to recovered individuals, pointing to BROADER IMMUNE DYSREGULATION.
5. Duration/ Implications:
- These humoral, cellular, and molecular perturbations persist for at least 6 months, supporting hypotheses of viral/antigenic persistence (possibly mucosal), dysregulated antibody production, and autoimmunity as drivers of diverse LC phenotypes.
6. Clinical relevance:
- The findings highlight the need for targeted therapies addressing persistent viral elements, aberrant humoral responses, and autoimmunity, and emphasize longitudinal immune profiling for diagnostics and therapeutic monitoring in Long COVID.
7. Limitations:
- The study does not mention reinfections, multiple infections, breakthrough infections, or specific SARS-CoV-2 variants (such as Delta or Omicron), or any vaccination related factors, it’s solely focused on LC patients!
‼️So, for those still in doubt, if that's even possible, this study proves unambiguously the #Leonardi_effect, showing Long COVID involves PERSISTENT, SEVERE IMMUNE DYSREGULATION, skewed IgG against Envelope/Nucleocapsid, chronically activated T cells, sustained inflammation, and autoimmunity, lasting ≥6 months, here pointing to ongoing viral/antigenic persistence! #AVOIDSARS2
FYI: @fitterhappierAJ
researchsquare.com/article/rs-830…
• • •
Missing some Tweet in this thread? You can try to
force a refresh