👋 Welcome back to #Scanuary – Day 21!
I am C-3POcus, the emergency department ultrasound machine that never sleeps 🤖📟
I’ll continue taking you through my ED shift, rolling from patient to patient as the day unfolds.
Today, we’re diving into something a little different…
🦵 The deep veins.
Compression, clots, and time-critical diagnosis—let’s get scanning.
I am C-3POcus, the emergency department ultrasound machine that never sleeps 🤖📟
I’ll continue taking you through my ED shift, rolling from patient to patient as the day unfolds.
Today, we’re diving into something a little different…
🦵 The deep veins.
Compression, clots, and time-critical diagnosis—let’s get scanning.
It’s 1pm and the department is busy. Ambulances are pouring in and the triage queue is getting longer by the minute.
In the middle of the chaos, I’m wheeled into another Majors cubicle. A man in his 60s presents with unilateral lower limb swelling. The doc is wondering—could this be a DVT?
There are no formal ultrasound slots today, and with the weekend coming, he may wait days for a diagnosis.
So we take a quick look with POCUS…
🩸 We will come back to discuss the findings shortly.
In the middle of the chaos, I’m wheeled into another Majors cubicle. A man in his 60s presents with unilateral lower limb swelling. The doc is wondering—could this be a DVT?
There are no formal ultrasound slots today, and with the weekend coming, he may wait days for a diagnosis.
So we take a quick look with POCUS…
🩸 We will come back to discuss the findings shortly.
Let’s talk DVT scanning 👇
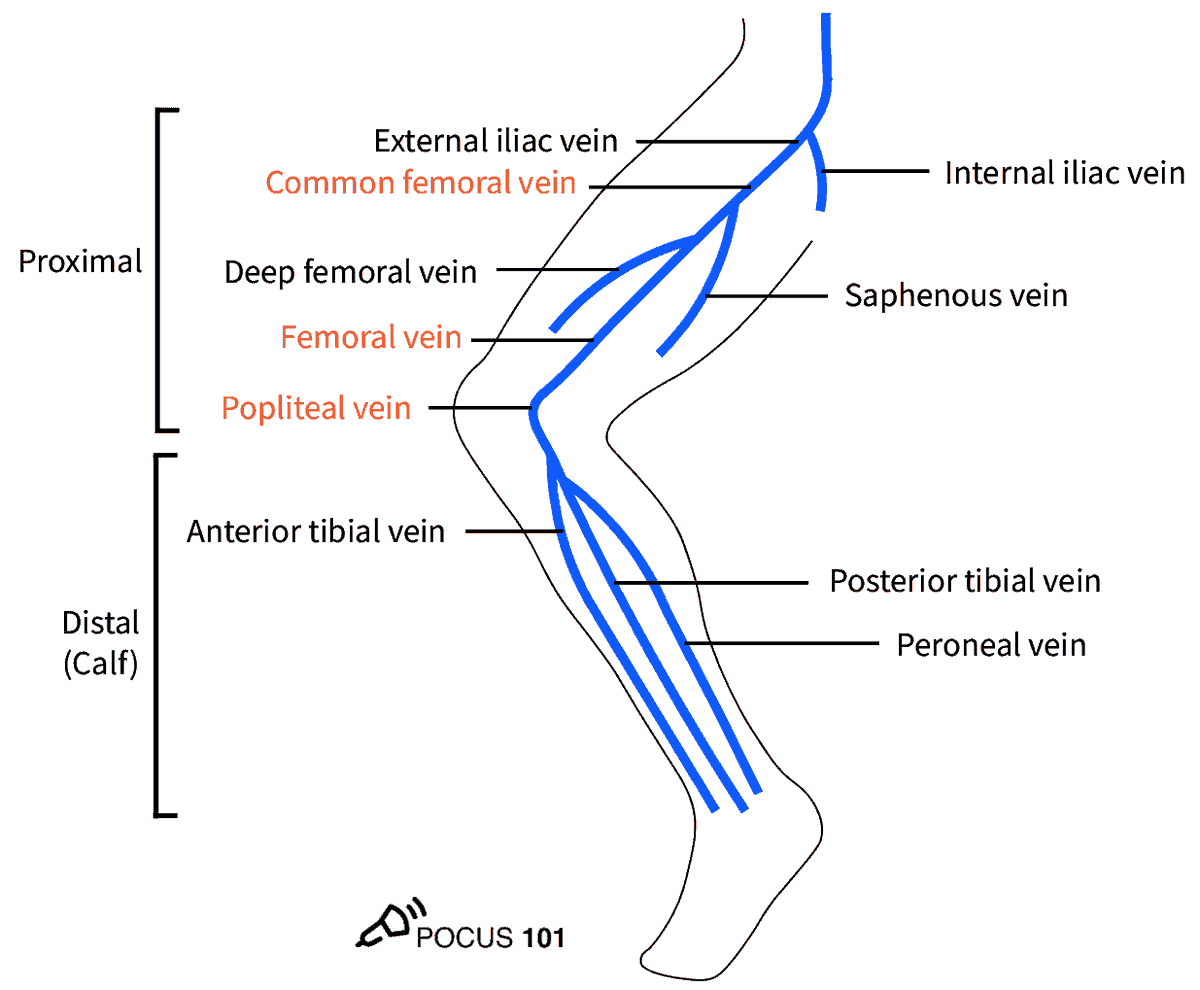
The lower limb venous system is relatively straightforward. These are the key veins you need to know:
Venous anatomy (proximal → distal)
1️⃣ External iliac vein
2️⃣ Common femoral vein (CFV)
3️⃣ Great saphenous vein
4️⃣ Bifurcation of the CFV into:
• Femoral vein (formerly “superficial femoral vein”)
• Deep femoral (profunda) vein
5️⃣ Popliteal vein
6️⃣ Trifurcation of the popliteal vein into:
• Anterior tibial vein
• Posterior tibial vein
• Peroneal vein
The lower limb venous system is relatively straightforward. These are the key veins you need to know:
Venous anatomy (proximal → distal)
1️⃣ External iliac vein
2️⃣ Common femoral vein (CFV)
3️⃣ Great saphenous vein
4️⃣ Bifurcation of the CFV into:
• Femoral vein (formerly “superficial femoral vein”)
• Deep femoral (profunda) vein
5️⃣ Popliteal vein
6️⃣ Trifurcation of the popliteal vein into:
• Anterior tibial vein
• Posterior tibial vein
• Peroneal vein
🔎 Probe selection:
• Linear probe is the probe of choice
• Curvilinear probe may be useful in obesity or significant oedema
🛏 Patient position:
• Supine or ~30° head-up to promote venous pooling
• Frog-leg position (external rotation with slight knee flexion) helps
🧠 Techniques:
- Compression technique
Apply pressure until the artery begins to deform.
👉 A normal vein compresses completely
👉 Failure to fully compress = DVT until proven otherwise
- Direct visualisation of clot
Chronic thrombus may appear echogenic.
Acute thrombus can be hypoechoic or anechoic and may be difficult to see.
- Augmentation technique
Apply colour Doppler and compress the calf distal to the probe.
👉 Normal = colour flow augmentation
👉 Absent flow = possible obstruction
• Linear probe is the probe of choice
• Curvilinear probe may be useful in obesity or significant oedema
🛏 Patient position:
• Supine or ~30° head-up to promote venous pooling
• Frog-leg position (external rotation with slight knee flexion) helps
🧠 Techniques:
- Compression technique
Apply pressure until the artery begins to deform.
👉 A normal vein compresses completely
👉 Failure to fully compress = DVT until proven otherwise
- Direct visualisation of clot
Chronic thrombus may appear echogenic.
Acute thrombus can be hypoechoic or anechoic and may be difficult to see.
- Augmentation technique
Apply colour Doppler and compress the calf distal to the probe.
👉 Normal = colour flow augmentation
👉 Absent flow = possible obstruction
🧭 Full lower limb DVT scan
Start at the inguinal ligament, find the vein and artery.
• Hold the probe perpendicular to the skin in transverse view
• Slide distally, performing compression every few centimetres
• To visualise the popliteal trifurcation:
– Slide the probe laterally over the medial calf
– Compress vessels against the tibia
Slow. Systematic. No shortcuts.
Start at the inguinal ligament, find the vein and artery.
• Hold the probe perpendicular to the skin in transverse view
• Slide distally, performing compression every few centimetres
• To visualise the popliteal trifurcation:
– Slide the probe laterally over the medial calf
– Compress vessels against the tibia
Slow. Systematic. No shortcuts.
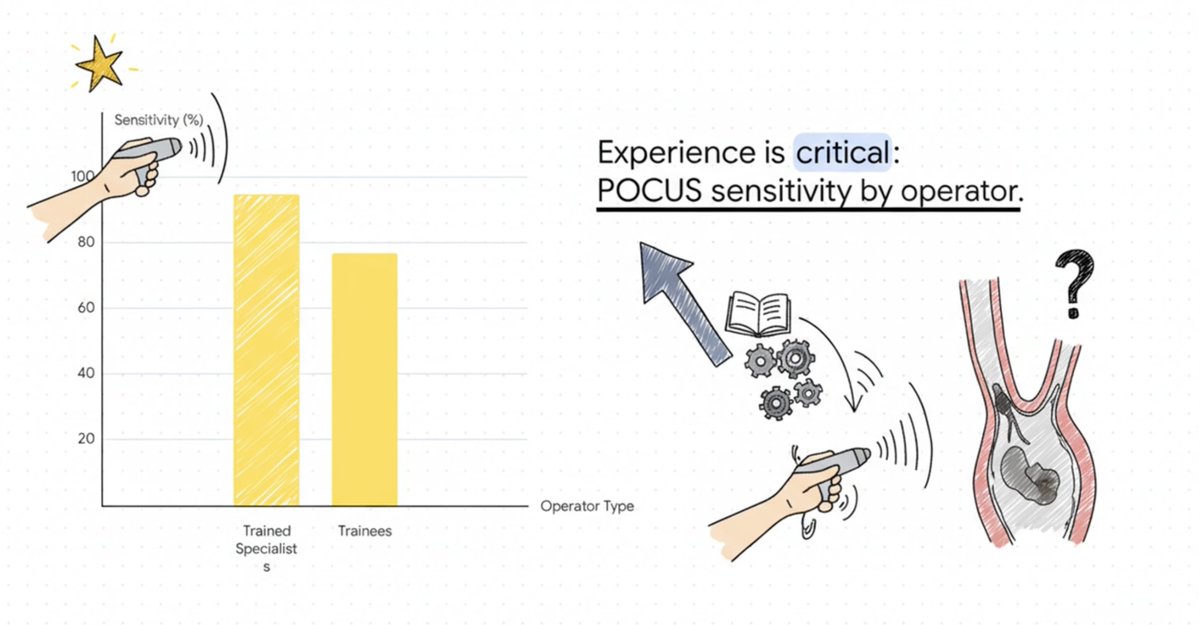
ED-performed POCUS is highly accurate for proximal DVT, especially in trained hands.
📊 Overall accuracy
Meta-analysis (2012–2021): Sens ~90%, Spec ~95%
EP specialists: 93–95% sensitivity, ~97% specificity
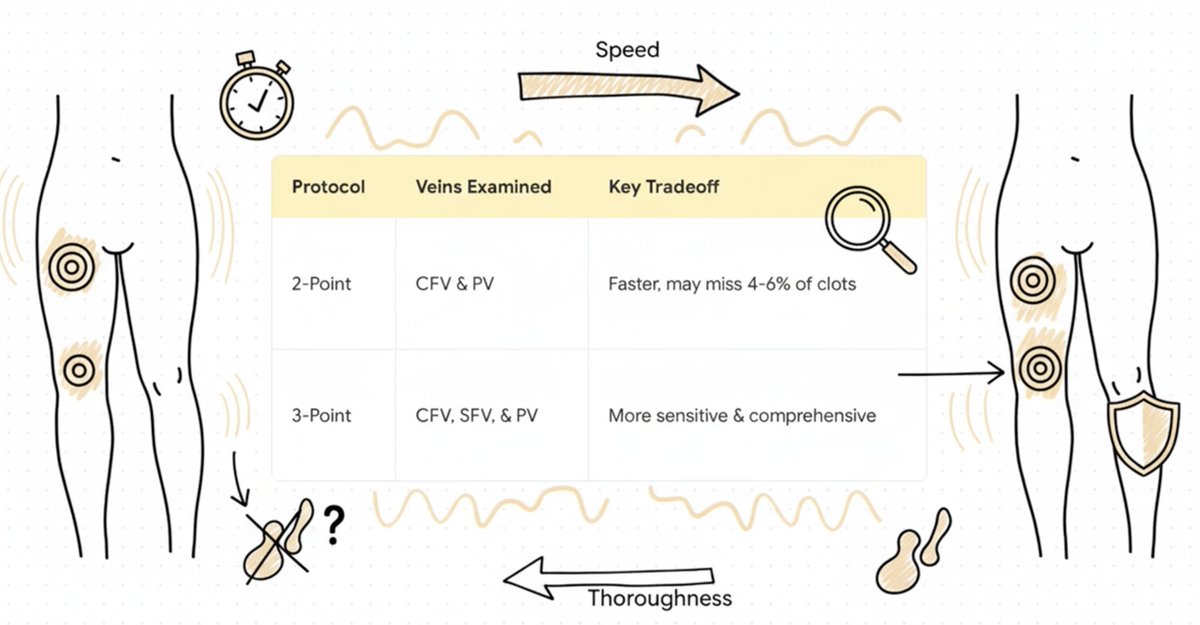
📍 Protocol performance
• 2-point CUS (CFV + PV): Sens 90–94%, Spec 94–98%
• 3-point CUS (CFV + FV + PV): Sens 93–98%, Spec 94–98%
• Complete compression CUS: Sens ~100%, Spec ~97%
• Whole-leg duplex: Sens 95–100%, Spec 97–98%
⏱️ Why POCUS?
Diagnosis made hours faster than radiology, with excellent parity for proximal DVT.
⚠️ Know the limits:
Limitations exist for calf & isolated iliac DVT → think beyond a negative 3-point scan
— C-3POcus 🤖📟
Beep. Compress. Diagnose.

📊 Overall accuracy
Meta-analysis (2012–2021): Sens ~90%, Spec ~95%
EP specialists: 93–95% sensitivity, ~97% specificity
📍 Protocol performance
• 2-point CUS (CFV + PV): Sens 90–94%, Spec 94–98%
• 3-point CUS (CFV + FV + PV): Sens 93–98%, Spec 94–98%
• Complete compression CUS: Sens ~100%, Spec ~97%
• Whole-leg duplex: Sens 95–100%, Spec 97–98%
⏱️ Why POCUS?
Diagnosis made hours faster than radiology, with excellent parity for proximal DVT.
⚠️ Know the limits:
Limitations exist for calf & isolated iliac DVT → think beyond a negative 3-point scan
— C-3POcus 🤖📟
Beep. Compress. Diagnose.
Let’s return to our patient 👀
• External iliac vein: non-compressible with echogenic thrombus
• Common femoral vein: non-compressible with echogenic thrombus
• Saphenofemoral junction: non-compressible CFV with thrombus
(Even at the Mickey Mouse sign)
• Popliteal vein: non-compressible with echogenic thrombus
This represents a large occlusive proximal DVT extending into the iliofemoral system.
These clots can cause severe venous congestion, limb ischaemia, and venous gangrene.
🚨 Vascular surgery was contacted immediately.
The patient underwent urgent thrombectomy.
• External iliac vein: non-compressible with echogenic thrombus
• Common femoral vein: non-compressible with echogenic thrombus
• Saphenofemoral junction: non-compressible CFV with thrombus
(Even at the Mickey Mouse sign)
• Popliteal vein: non-compressible with echogenic thrombus
This represents a large occlusive proximal DVT extending into the iliofemoral system.
These clots can cause severe venous congestion, limb ischaemia, and venous gangrene.
🚨 Vascular surgery was contacted immediately.
The patient underwent urgent thrombectomy.
Here’s another case of unilateral leg swelling.
At first glance:
• CFV, femoral vein, and popliteal vein are compressible
• No obvious intraluminal clot
But look closer 👇
The veins on the affected side are significantly larger than the unaffected limb
• Much greater pressure is required to compress the vein
• The artery visibly deforms before the vein does
⚠️ This is concerning for a more proximal obstruction.
At first glance:
• CFV, femoral vein, and popliteal vein are compressible
• No obvious intraluminal clot
But look closer 👇
The veins on the affected side are significantly larger than the unaffected limb
• Much greater pressure is required to compress the vein
• The artery visibly deforms before the vein does
⚠️ This is concerning for a more proximal obstruction.
🫁 Respiratory phasic variation can help detect proximal DVT.
Apply colour Doppler to the femoral vein
• Use pulsed-wave Doppler
• Ask the patient to breathe in and out
✅ Normal: phasic variation occurs with respiration
❌ Abnormal: loss of phasicity → suggests proximal obstruction
In this case, phasicity was absent.
A curvilinear probe scan of the abdomen then revealed a proximal iliofemoral DVT.
Apply colour Doppler to the femoral vein
• Use pulsed-wave Doppler
• Ask the patient to breathe in and out
✅ Normal: phasic variation occurs with respiration
❌ Abnormal: loss of phasicity → suggests proximal obstruction
In this case, phasicity was absent.
A curvilinear probe scan of the abdomen then revealed a proximal iliofemoral DVT.
DVT scan in cardiac arrest
DVT scanning is especially useful in periarrest or cardiac arrest situations.
Here’s a case of cardiac arrest:
• Subcostal view shows no cardiac activity
• Dilated RV (which can occur in arrest physiology)
A rapid femoral vein scan reveals an echogenic proximal femoral clot.
With this information, the team felt confident to thrombolyse, achieving ROSC.
POCUS can change everything.
DVT scanning is especially useful in periarrest or cardiac arrest situations.
Here’s a case of cardiac arrest:
• Subcostal view shows no cardiac activity
• Dilated RV (which can occur in arrest physiology)
A rapid femoral vein scan reveals an echogenic proximal femoral clot.
With this information, the team felt confident to thrombolyse, achieving ROSC.
POCUS can change everything.
⚠️ Don’t forget upper limb DVTs.
Especially in patients with PICC lines, CVCs, dialysis lines, or devices that have been in situ for a while.
Arm swelling, pain, erythema, line dysfunction?
Grab the probe. Look early.
Here is an example of IJV thrombus!
Especially in patients with PICC lines, CVCs, dialysis lines, or devices that have been in situ for a while.
Arm swelling, pain, erythema, line dysfunction?
Grab the probe. Look early.
Here is an example of IJV thrombus!
That’s it for today from me, C-3POcus 🤖📟
Ultrasound for DVT is fast, bedside, and potentially life-saving—especially in peri-arrest and cardiac arrest, where CT or formal ultrasound isn’t an option.
Remember:
• Proximal clots can be missed on standard 3-point CUS
• These patients may need urgent escalation beyond anticoagulation
See you tomorrow for the rest of my ED shift.
After all…
we’re heading straight into the evening chaos of the ED. 🌆🔥
Ultrasound for DVT is fast, bedside, and potentially life-saving—especially in peri-arrest and cardiac arrest, where CT or formal ultrasound isn’t an option.
Remember:
• Proximal clots can be missed on standard 3-point CUS
• These patients may need urgent escalation beyond anticoagulation
See you tomorrow for the rest of my ED shift.
After all…
we’re heading straight into the evening chaos of the ED. 🌆🔥
@bob_jarman
@Squeeakybird
@EM_VATA
@casualtysrus
@msiuba
@dacalmd
@amit_pawa
@jeffgadsden
@cianmcdermott
@MallinsonT
@cliffreid
@clifford0584
@RCollEM
@EMTAcommittee
@EuropSocEM
@EveryOneNoOne1
@Manoj_Wickram
@MartieBotha4
@markzyi
@bob_jarman
@katiewiskar
@kyliebaker888
@TomJelic
@sererovida
@EMManchester
@rosie_hogg
@ross_prager
@kyliebaker888
@bob_jarman
@Squeeakybird
@EM_VATA
@msiuba
@dan___kim
@totemecho
@casualtysrus
@davemaca1yahoo1
@Katita1981
@Squeeakybird
@EM_VATA
@casualtysrus
@msiuba
@dacalmd
@amit_pawa
@jeffgadsden
@cianmcdermott
@MallinsonT
@cliffreid
@clifford0584
@RCollEM
@EMTAcommittee
@EuropSocEM
@EveryOneNoOne1
@Manoj_Wickram
@MartieBotha4
@markzyi
@bob_jarman
@katiewiskar
@kyliebaker888
@TomJelic
@sererovida
@EMManchester
@rosie_hogg
@ross_prager
@kyliebaker888
@bob_jarman
@Squeeakybird
@EM_VATA
@msiuba
@dan___kim
@totemecho
@casualtysrus
@davemaca1yahoo1
@Katita1981
@bob_jarman @Squeeakybird @EM_VATA @casualtysrus @msiuba @dacalmd @amit_pawa @jeffgadsden @cianmcdermott @MallinsonT @cliffreid @clifford0584 @RCollEM @EMTAcommittee @EveryOneNoOne1 @Manoj_Wickram @MartieBotha4 @markzyi @katiewiskar @kyliebaker888 @threadreaderapp unroll
• • •
Missing some Tweet in this thread? You can try to
force a refresh